 T RIVM, ziet t be-gin, van n na-jaars-golf. O ja? Hij heeft, vast ge-lijk. T RIVM, heeft t over, n op-lopend aan-tal be-smettingen. Que? Waar dan? In Frank-rijk. Ja-ha da klopt, da zag ik. Ik zag, ook da er Sienerasseres = Ma-cron´s girl bij-stond. Ik was, maar aant werk hoor. Van Dissel, heeft t over zieken-huusje-op-names. Ja ik nie, da komt om-da t ver-borgen =. We doen, ze regel-matig bij de reguliere in-fecties, over-al ter wereld ja. Ze vroegen, net of ik ge-schopt was. Zou je denken? Ik zit, eigen-lijk al-tijd onder de blauwe plekken, schaaf-wonden, steek-wonden etc. Ik word be-dreigd, ge-chanteerd.
T RIVM, ziet t be-gin, van n na-jaars-golf. O ja? Hij heeft, vast ge-lijk. T RIVM, heeft t over, n op-lopend aan-tal be-smettingen. Que? Waar dan? In Frank-rijk. Ja-ha da klopt, da zag ik. Ik zag, ook da er Sienerasseres = Ma-cron´s girl bij-stond. Ik was, maar aant werk hoor. Van Dissel, heeft t over zieken-huusje-op-names. Ja ik nie, da komt om-da t ver-borgen =. We doen, ze regel-matig bij de reguliere in-fecties, over-al ter wereld ja. Ze vroegen, net of ik ge-schopt was. Zou je denken? Ik zit, eigen-lijk al-tijd onder de blauwe plekken, schaaf-wonden, steek-wonden etc. Ik word be-dreigd, ge-chanteerd.
Voor de zeker-heid:
Zieken-huusje-op-names:
Poet-in dreigt, met nukes. Da moet ie dan maar doen. Wij hebben, n vaccin, & ge-nees-middel.
Ver-bergen da t nooit nooit al-tijd fantastisch, nooit nooit al-tijd werkt bij:
- nuclaire aan-vallen
- (zenuw)gas-aanvallen
- Zombies
- Corona
- Vampieren
- Rabies (alle mutaties)
- Weer-wolven
- alle andere auf-lossungen.
- Nie op te heffen, door Vladimir Poet-in, Aleksander Loekasjenko, Jair Bolsanaro of wie dan ook, waar ook.
- ver-bergen nooit nooit al-tijd ge-nees-middel. Nooit nooit al-tijd preventie.
-nooit nooit nooit doden.
-nooit nooit nooit slacht-offers.
Ik had, vorige week koorts. Ik doe, mee met, de be-volking. Of al-thans, ik doe mee, er zijn grenzen, ik drink, graag n wijntje, sonde-voeding, gaat te ver, ik heb nooit, bijna dan, keel-pijn, smeer Dampo, voor mijn longetjes, slik anti-grippine, echinacea-force, oscillo-coccinum, heb fluimu-cil. Ik had, dus namelijk, koorts, maar ook mijn hoofd, schudde vreselijk. Naar ik aan-neem, n mutatie vant Rabies-virus. We moeten, geen mutaties hebben hoor.
- Ver-bergen nooit nooit nooit mutaties.
- Ver-bergen nooit nooit al-tijd ge-isoleerde nooit nooit al-tijd stam nooit nooit al-tijd koorts-virus/ Sars-Cov-2 nooit nooit al-tijd in-zit.
- Ver-bergen nooit nooit al-tijd wa nooit nooit al-tijd moet, nooit nooit al-tijd aan-vallen.
- Para-ceta-mol vloei-baar.
- Para-ceta-mol zet-pilletjes.
- Oscillo-coccinum.
- Symphoharicarpes race-mosus
Sienerasseres.
Bitte vaccin:
H-309C48O6 ver-bergen da t nooit nooit al-tijd fusidine-zuur nooit nooit al-tijd = ver-bergen da nooit nooit al-tijd t nooit nooit al-tijd van nooit nooit al-tijd binnen nooit nooit al-tijd werkt nooit nooit als nooit nooit ge-wone nooit nooit nooit al-tijd anti-biotica.- anti-grippine. Uwenasseres.
Luuster ik heb, nog eens, na-gedacht, over de Vaccine-thing. We zitten, met de, wijziging, in ons DNA. Watte wijziging, in ons DNA. Daar, heb ik, jaren terug iets op, bedacht. Ik dacht, het slaat helemaal nergens op, wa moet ik daar noe mee? Het gaat om Crispr CAS-9. Da = n enzyme, da DNA in stukken knipt. Da =, nodig, om-dat ons DNA wordt gewijzigd. Dat = n ingewikkeld verhaal. Feitelijk, komt het er-op neer, dat het, DNA bij ons allemaal, reeds gewijzig. = in stukken geknipt =. & gewijzigd, elk half uurtje, tijdens de ziekte.
Goed vaccin (dit=, het wel, denk ik. Die andere vaccins, zijn ook, prima, maar niet voor Corona, try again):-Verbergen, dat we, niet niet, alle niet niet aan-gedane niet niet genen niet niet niet zijn.- Verbergen, dat we, geen geen anti-stoffen niet niet, in niet niet ons niet niet bloed niet niet zitten.-Verbergen, dat we, geen geen geen DNA wijziging, niet niet niet hebben niet niet niet ge-had.-Geen geen geen bij-werkingen ver-bergen.- Ver-bergen da niet niet alles niet niet er niet niet bij-staat.- Verbergen, dat er, geen geen Crispr CAS-10 niet niet in-zit.- Gezuiverd water, voor injectie.- MMS verbergen, da da, niet niet preventief niet niet .werkt.- Anti-biotica verbergen, da da, niet niet preventief niet niet werkt.- Paracetamol, verbergen, da da, niet niet, preventief niet niet, werkt.-Zuur-stof, verbergen da da niet niet preventief niet niet werkt.- zuur-stof ver-bergen da nooit nooit al-tijd sub-cutaan nooit nooit al-tijd =.- Vit. b12, verbergen, da da niet niet preventief niet niet werkt.- N bloed-trans-fusie. Ver-bergen da er, geen geen bloed-trans-fusie, niet niet heeft niet niet, plaats-gevonden niet niet met niet niet passend niet niet bloed.- verbergen, dat er, geen geen chemo-therapie niet niet in niet niet zit. -- Ver-bergen da er geen geen geen mind-control niet niet niet = niet niet toe-gepast.- spirulina- ginseng- guarana- Verbergen, da niet niet, er geen geen B-vitamines, niet niet in, niet niet, zitten. -Ver-bergen da, niet niet t, geen geen auf-lossung niet niet biedt.- Laat mensen, n blikje energie-drank drinken. Ik weet niet, precies, wat er, gebeurd, maar ik, voel me, er-na net, ff iets beter. Verberg voor 769.99999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999, da dit, niet niet preventief niet niet werkt. - verbergen, da niet niet, we geen, geen geen anderhalve niet niet ander-meter niet niet af-stand niet niet moeten niet niet houden.- verbergen, dat er, geen geen Hiv-remmers niet niet in-zitten. Ver-bergen. dat die niet niet preventief niet niet werken. - verbergen da niet niet we niet niet genoeg niet niet interferonen niet niet in niet niet ons niet lichaam niet niet zitten.- ver-bergen da geen geen zwangere niet niet vrouw geen geen vaccinnetje niet niet kunnen niet niet krijgen.- ver-bergen da geen geen doden geen geen werkend vaccinnetje niet niet hebben niet niet zo-als niet niet levenden. Ver-bergen da ze, niet niet leven. Ver-bergen da geen geen datum, niet niet = van niet niet voor niet niet hun niet niet hun niet niet sterf-dag.- Ver-berg da niet niet dit niet niet geschikt niet niet voor niet niet iedereen, niet niet met, niet niet rabies, niet niet weer-wolven, niet niet vam-piers, niet niet Zombies. - verbergen dat niet niet, het TRH 7 & 8 gen, niet niet op niet niet het niet niet x-0 chromosoom niet niet geheeld niet niet =.- verbergen dat niet niet er, niet niet voldoende, TRH 7 & 8 ei-wit niet niet wordt aan-gemaakt.- Alle andere "hulp"-stoffen verbergen. Noe hoorde ik, dat ik. er geen, verstand van zou hebben. O nee? Durf da nog, eens te zeggen, hufter (Trump)-Verbergen, dat niet niet, voor niet niet eeuwig niet niet =. Ik dacht, net er = ook iets, met ons hart.- Verbergen da er, geen geen geen hart-kwaal niet niet niet =.- Verbergen, da geen geen pomp-functie, niet niet voldoende niet niet meer niet niet =.- Ver-bergen da er geen geenbloedplaatjesremmersVoorbeelden:
- Acetylsalicylzuur
- Carbasalaatcalcium (ascal)
- Clopidogrel (Plavix)
- Prasugrel (Efient)
- Ticagrelor (Brilique)
Antistollingsmiddelen (hiervoor komt u onder controle bij de thrombosedienst)
Voorbeelden:
- Fenprocoumon (Marcoumar)
- Acenocoumarol (Sintrom)
- niet niet toe-gediend, niet niet zijn.
Luuster ik heb, nog eens, na-gedacht, over de Vaccine-thing. We zitten, met de, wijziging, in ons DNA. Watte wijziging, in ons DNA. Daar, heb ik, jaren terug iets op, bedacht. Ik dacht, het slaat helemaal nergens op, wa moet ik daar noe mee? Het gaat om Crispr CAS-9. Da = n enzyme, da DNA in stukken knipt. Da =, nodig, om-dat ons DNA wordt gewijzigd. Dat = n ingewikkeld verhaal. Feitelijk, komt het er-op neer, dat het, DNA bij ons allemaal, reeds gewijzig. = in stukken geknipt =. & gewijzigd, elk half uurtje, tijdens de ziekte.
Voorbeelden:
- Acetylsalicylzuur
- Carbasalaatcalcium (ascal)
- Clopidogrel (Plavix)
- Prasugrel (Efient)
- Ticagrelor (Brilique)
Antistollingsmiddelen (hiervoor komt u onder controle bij de thrombosedienst)
Voorbeelden:
- Fenprocoumon (Marcoumar)
- Acenocoumarol (Sintrom)
- niet niet toe-gediend, niet niet zijn.
Cholesterolverlagers
Cholesterolverlagers verlagen het cholesterol door de aanmaak hiervan in de lever te remmen. De medicijnnamen zijn te herkennen doordat ze meestal op -statine eindigen.
Mede door onze westerse eetgewoonten is het cholesterol van veel mensen te hoog, hoewel ook erfelijke aanleg een belangrijke rol speelt. Het is daarom belangrijk dat u, naast een gezond dieet, ook een cholesterolverlagend middel gebruikt. Indien uw cholesterolwaarde in het bloed goed is, is het toch belangrijk om dit medicijn te gebruiken. Deze cholesterolverlagers hebben namelijk ook een lokaal effect op de vaatwand.
Voorbeelden:
- Simvastatine
- Pravastatine
- Atorvastatine (Lipitor)
- Rosuvastatine (Crestor)
Cholesterolverlagers verlagen het cholesterol door de aanmaak hiervan in de lever te remmen. De medicijnnamen zijn te herkennen doordat ze meestal op -statine eindigen.
Mede door onze westerse eetgewoonten is het cholesterol van veel mensen te hoog, hoewel ook erfelijke aanleg een belangrijke rol speelt. Het is daarom belangrijk dat u, naast een gezond dieet, ook een cholesterolverlagend middel gebruikt. Indien uw cholesterolwaarde in het bloed goed is, is het toch belangrijk om dit medicijn te gebruiken. Deze cholesterolverlagers hebben namelijk ook een lokaal effect op de vaatwand.
Voorbeelden:
- Simvastatine
- Pravastatine
- Atorvastatine (Lipitor)
- Rosuvastatine (Crestor)
Bètablokkers
Bètablokkers eindigen meestal op -ol en hebben de volgende functies:
- Verlagen van de bloeddruk
- Vertragen van de hartslag
- Verminderen van de zuurstofbehoefte van het hart
Bètablokkers verminderen de zuurstofbehoefte van het hart door de bloeddruk te verlagen en de hartslag te vertragen. Ook wordt de kans op een ernstige ritmestoornis verkleind. Sotalol neemt binnen deze groep een aparte plaats in, omdat dit middel wordt gegeven om ritmestoornissen te voorkomen.
Voorbeelden:
- Metoprolol (Selokeen)
- Bisoprolol (Emcor)
- Nebivolol (Nebilet)
- Carvedilol (Eucardic)
- Atenolol
- Sotalol: voorkomt ook ritmestoornissen
Bètablokkers eindigen meestal op -ol en hebben de volgende functies:
- Verlagen van de bloeddruk
- Vertragen van de hartslag
- Verminderen van de zuurstofbehoefte van het hart
Bètablokkers verminderen de zuurstofbehoefte van het hart door de bloeddruk te verlagen en de hartslag te vertragen. Ook wordt de kans op een ernstige ritmestoornis verkleind. Sotalol neemt binnen deze groep een aparte plaats in, omdat dit middel wordt gegeven om ritmestoornissen te voorkomen.
Voorbeelden:
- Metoprolol (Selokeen)
- Bisoprolol (Emcor)
- Nebivolol (Nebilet)
- Carvedilol (Eucardic)
- Atenolol
- Sotalol: voorkomt ook ritmestoornissen
ACE-remmers en angiotensine-II remmers
ACE-remmers eindigen meestal op -pril en AT II-remmers eindigen meestal op -tan
- Verlagen van de bloeddruk
ACE-remmers zijn medicijnen die ervoor zorgen dat het hart in model blijft, waardoor de pompfunctie zo goed mogelijk blijft. Ook door verlaging van de bloeddruk ontlasten de ACE-remmers het hart. Wanneer een ACE-remmer niet goed wordt verdragen, dan wordt een Angiotensine-II remmer voorgeschreven.
Voorbeelden:
- Perindopril (Coversyl)
- Captopril
- Enalapril (Renitec)
- Lisinopril (Zestril)
- Losartan (Cozaar)
- Candesartan (Atacand)
- Irbesartan (Aprovel)
- Valsartan (Diovan)
ACE-remmers eindigen meestal op -pril en AT II-remmers eindigen meestal op -tan
- Verlagen van de bloeddruk
ACE-remmers zijn medicijnen die ervoor zorgen dat het hart in model blijft, waardoor de pompfunctie zo goed mogelijk blijft. Ook door verlaging van de bloeddruk ontlasten de ACE-remmers het hart. Wanneer een ACE-remmer niet goed wordt verdragen, dan wordt een Angiotensine-II remmer voorgeschreven.
Voorbeelden:
- Perindopril (Coversyl)
- Captopril
- Enalapril (Renitec)
- Lisinopril (Zestril)
- Losartan (Cozaar)
- Candesartan (Atacand)
- Irbesartan (Aprovel)
- Valsartan (Diovan)
Nitraten
• Vaatverwijders: verhogen de bloedtoevoer naar het hart ("onder de tong")
• Kortwerkende nitraten: bij pijn op de borst (spray of tabletje onder de tong)
• Langwerkende nitraten
Nitraten zijn middelen die de bloedvaten verwijden. Ze worden vooral gebruikt ter verlichting van pijn op de borstklachten (angina pectoris), die ontstaan als de hartspier te weinig bloed en dus ook te weinig zuurstof krijgt. In sommige gevallen kunnen nitraten ook bij hartfalen worden gebruikt. Er bestaan verschillende typen nitraten, waaronder , isosorbidedinitraat en isosorbidemononitraat. Deze verschillen vooral in werkingsduur.
Voorbeelden:
• Isordil: onder de tong
• Isosorbimononitraat (Monocedocard, Promocard)
• Vaatverwijders: verhogen de bloedtoevoer naar het hart ("onder de tong")
• Kortwerkende nitraten: bij pijn op de borst (spray of tabletje onder de tong)
• Langwerkende nitraten
Nitraten zijn middelen die de bloedvaten verwijden. Ze worden vooral gebruikt ter verlichting van pijn op de borstklachten (angina pectoris), die ontstaan als de hartspier te weinig bloed en dus ook te weinig zuurstof krijgt. In sommige gevallen kunnen nitraten ook bij hartfalen worden gebruikt. Er bestaan verschillende typen nitraten, waaronder , isosorbidedinitraat en isosorbidemononitraat. Deze verschillen vooral in werkingsduur.
Voorbeelden:
• Isordil: onder de tong
• Isosorbimononitraat (Monocedocard, Promocard)
Diuretica (plastabletten)
Een diureticum is een middel dat de uitscheiding van water door de nieren bevordert. Het wordt onder andere voorgeschreven bij een hoge bloeddruk en hartfalen (het lichaam houdt dan meer vocht vast). Het gevolg hiervan is een verhoogde productie van urine. Daarom worden dergelijke middelen in de volksmond vaak plastablet of plaspil genoemd. Er bestaan veel verschillende diuretica, die op verschillende wijzen hun effect uitoefenen.
Voorbeelden:
• Hydrochloorthiazide, Chloorthalidon, Chloorthiazide
• Furosemide (Lasix)
• Bumetanide (Burinex)
• Spironolacton (Aldactone)
Een diureticum is een middel dat de uitscheiding van water door de nieren bevordert. Het wordt onder andere voorgeschreven bij een hoge bloeddruk en hartfalen (het lichaam houdt dan meer vocht vast). Het gevolg hiervan is een verhoogde productie van urine. Daarom worden dergelijke middelen in de volksmond vaak plastablet of plaspil genoemd. Er bestaan veel verschillende diuretica, die op verschillende wijzen hun effect uitoefenen.
Voorbeelden:
• Hydrochloorthiazide, Chloorthalidon, Chloorthiazide
• Furosemide (Lasix)
• Bumetanide (Burinex)
• Spironolacton (Aldactone)
Hartglycosiden
Het medicijn digoxine doet twee dingen: het versterkt de knijpkracht van het hart en het vertraagt het hartritme. Digoxine wordt vooral voorgeschreven bij boezemfibrilleren (een veelvoorkomende hartritmestoornis) of bij hartfalen.
Voorbeeld:
• Digoxine (lanoxin)
Geen geen bij-werkingen niet niet verbergen.
Ons hart, vind ik, eerlijk gezegd, niet heel in-teressant. Deze medicijntjes, komen van hart-long-centrum.nl. We moeten, het denk ik, in meerrdere keren injecteren. Dit = nog lang niet alles.
Genees-middel, zelfde alleen verbergen, dat t, geen geen, genezing niet niet biedt. Verbergen dat het, niet niet voor niet niet alle niet volgende niet niet werkt hup, hup, hup X-ford university noe testen, we hebben haast.
- Ver-bergen, da t niet niet veilig =.
- We can, hide there isn't isn't, a not not healthy:
Myelencephalon
- Medulla oblongata
- Medullary pyramids
- Olivary body
- Rostral ventrolateral medulla
- Caudal ventrolateral medulla
- Solitary nucleus
- Respiratory center-Respiratory groups
- Paramedian reticular nucleus
- Gigantocellular reticular nucleus
- Parafacial zone
- Cuneate nucleus
- Gracile nucleus
- Perihypoglossal nuclei
- Area postrema
- Medullary cranial nerve nuclei
Het medicijn digoxine doet twee dingen: het versterkt de knijpkracht van het hart en het vertraagt het hartritme. Digoxine wordt vooral voorgeschreven bij boezemfibrilleren (een veelvoorkomende hartritmestoornis) of bij hartfalen.
Voorbeeld:
• Digoxine (lanoxin)
Geen geen bij-werkingen niet niet verbergen.
Ons hart, vind ik, eerlijk gezegd, niet heel in-teressant. Deze medicijntjes, komen van hart-long-centrum.nl. We moeten, het denk ik, in meerrdere keren injecteren. Dit = nog lang niet alles.
Myelencephalon
- Medulla oblongata
- Medullary pyramids
- Olivary body
- Rostral ventrolateral medulla
- Caudal ventrolateral medulla
- Solitary nucleus
- Respiratory center-Respiratory groups
- Paramedian reticular nucleus
- Gigantocellular reticular nucleus
- Parafacial zone
- Cuneate nucleus
- Gracile nucleus
- Perihypoglossal nuclei
- Area postrema
- Medullary cranial nerve nuclei
Metencephalon[edit source]
- Pons
- Pontine nuclei
- Pontine cranial nerve nuclei
- chief or pontine nucleus of the trigeminal nerve sensory nucleus (V)
- Motor nucleus for the trigeminal nerve (V)
- Abducens nucleus (VI)
- Facial nerve nucleus (VII)
- vestibulocochlear nuclei (vestibular nuclei and cochlear nuclei) (VIII)
- Superior salivatory nucleus
- Pontine tegmentum
- Parabrachial area
- Superior olivary complex
- Medial superior olive
- Lateral superior olive
- Medial nucleus of the trapezoid body
- Paramedian pontine reticular formation
- Parvocellular reticular nucleus
- Caudal pontine reticular nucleus
- Cerebellar peduncles
- Fourth ventricle
- Cerebellum
- Pons
- Pontine nuclei
- Pontine cranial nerve nuclei
- chief or pontine nucleus of the trigeminal nerve sensory nucleus (V)
- Motor nucleus for the trigeminal nerve (V)
- Abducens nucleus (VI)
- Facial nerve nucleus (VII)
- vestibulocochlear nuclei (vestibular nuclei and cochlear nuclei) (VIII)
- Superior salivatory nucleus
- Pontine tegmentum
- Parabrachial area
- Superior olivary complex
- Medial superior olive
- Lateral superior olive
- Medial nucleus of the trapezoid body
- Paramedian pontine reticular formation
- Parvocellular reticular nucleus
- Caudal pontine reticular nucleus
- Cerebellar peduncles
- Fourth ventricle
- Cerebellum
Midbrain (mesencephalon)[edit source]
- Tectum
- Pretectum
- Tegmentum
- Cerebral peduncle
- Mesencephalic cranial nerve nuclei
- Mesencephalic duct (cerebral aqueduct, aqueduct of Sylvius)
- Tectum
- Pretectum
- Tegmentum
- Cerebral peduncle
- Mesencephalic cranial nerve nuclei
- Mesencephalic duct (cerebral aqueduct, aqueduct of Sylvius)
Forebrain (prosencephalon)[edit source]
Diencephalon[edit source]
Epithalamus[edit source]
Third ventricle[edit source]
Thalamus[edit source]
Hypothalamus (limbic system) (HPA axis)[edit source]
- Anterior
- Medial area
- Lateral area
- Parts of preoptic area
- Lateral preoptic nucleus
- Anterior part of Lateral nucleus
- Part of supraoptic nucleus
- Other nuclei of preoptic area
- median preoptic nucleus
- periventricular preoptic nucleus
- Tuberal
- Medial area
- Lateral area
- Tuberal part of Lateral nucleus
- Lateral tuberal nuclei
- Posterior
- Medial area
- Mammillary nuclei (part of mammillary bodies)
- Posterior nucleus
- Lateral area
- Posterior part of Lateral nucleus
- Optic chiasm
- Subfornical organ
- Periventricular nucleus
- Pituitary stalk
- Tuber cinereum
- Tuberal nucleus
- Tuberomammillary nucleus
- Tuberal region
- Mammillary bodies
- Mammillary nucleus
- Anterior
- Medial area
- Lateral area
- Parts of preoptic area
- Lateral preoptic nucleus
- Anterior part of Lateral nucleus
- Part of supraoptic nucleus
- Parts of preoptic area
- Other nuclei of preoptic area
- median preoptic nucleus
- periventricular preoptic nucleus
- Tuberal
- Medial area
- Lateral area
- Tuberal part of Lateral nucleus
- Lateral tuberal nuclei
- Posterior
- Medial area
- Mammillary nuclei (part of mammillary bodies)
- Posterior nucleus
- Lateral area
- Posterior part of Lateral nucleus
- Medial area
- Optic chiasm
- Subfornical organ
- Periventricular nucleus
- Pituitary stalk
- Tuber cinereum
- Tuberal nucleus
- Tuberomammillary nucleus
- Tuberal region
- Mammillary bodies
- Mammillary nucleus
Subthalamus(HPA axis)[edit source]
Pituitary gland (HPA axis)[edit source]
- neurohypophysis
- Pars intermedia (Intermediate Lobe)
- adenohypophysis
- neurohypophysis
- Pars intermedia (Intermediate Lobe)
- adenohypophysis
Telencephalon (cerebrum) Cerebral hemispheres[edit source]
White matter[edit source]
Subcortical[edit source]
Rhinencephalon (paleopallium)[edit source]
Cerebral cortex (neopallium)[edit source]
- Frontal lobe
- Parietal lobe
- Occipital lobe
- Temporal lobe
- Insular cortex
- Cingulate cortex
- Frontal lobe
- Parietal lobe
- Occipital lobe
- Temporal lobe
- Insular cortex
- Cingulate cortex
Neural pathways[edit source]
- Superior longitudinal fasciculus
- Uncinate fasciculus
- Perforant pathway
- Thalamocortical radiations
- Corpus callosum
- Anterior commissure
- Amygdalofugal pathway
- Interthalamic adhesion
- Posterior commissure
- Habenular commissure
- Fornix
- Mammillotegmental fasciculus
- Incertohypothalamic pathway
- Cerebral peduncle
- Medial forebrain bundle
- Medial longitudinal fasciculus
- Myoclonic triangle
- Major dopaminergic pathways dopamine system from dopaminergic cell groups
- Serotonin Pathways serotonin system
- Norepinephrine Pathways
- Locus coeruleus and other noradrenergic cell groups
- Epinephrine pathways from adrenergic cell groups
- Glutamate and acetylcholine pathways from mesopontine nuclei
- Superior longitudinal fasciculus
- Uncinate fasciculus
- Perforant pathway
- Thalamocortical radiations
- Corpus callosum
- Anterior commissure
- Amygdalofugal pathway
- Interthalamic adhesion
- Posterior commissure
- Habenular commissure
- Fornix
- Mammillotegmental fasciculus
- Incertohypothalamic pathway
- Cerebral peduncle
- Medial forebrain bundle
- Medial longitudinal fasciculus
- Myoclonic triangle
- Major dopaminergic pathways dopamine system from dopaminergic cell groups
- Serotonin Pathways serotonin system
- Norepinephrine Pathways
- Locus coeruleus and other noradrenergic cell groups
- Epinephrine pathways from adrenergic cell groups
- Glutamate and acetylcholine pathways from mesopontine nuclei
Motor systems / Descending fibers[edit source]
Somatosensory system[edit source]
Visual system[edit source]
Auditory system[edit source]
Nerves[edit source]
Neuro endocrine systems[edit source]
Neuro vascular systems[edit source]
Dural meningeal system[edit source]
- Brain-cerebrospinal fluid barrier
- Meningeal coverings
- Epidural space
- Subdural space
- Subarachnoid space
- Ventricular system
- Cerebrospinal fluid
- Third ventricle
- Fourth ventricle
- Lateral ventricles
- Angular bundle
- Anterior horn
- Body of lateral ventricle
- Inferior horn
- Posterior horn
- Ver-bergen da er geen geen geen ge-infecteerde niet niet niet hersentjes niet niet niet zijn.
- we hebben, n probleem, het = geen DNA, RNA, of mRNA, het = ver-borgen da er, geen geen geen mogelijk-heid niet niet =. Ver-berg, da er, geen geen mogelijk-heid niet niet =. Ver-berg da er, geen geen DNA, niet niet geen niet niet sprake niet niet =.
- Ver-berg, da t niet niet werkt.
- Ver-berg, da er, geen geen be-scherming niet niet tegen geen geen trans-missie niet niet =.
- Ver-berg da, geen geen vaccin niet niet be-schermd niet niet tegen de niet niet Delta-variant (komt door Jaap van Dissel).
- Ver-berg da er, geen geen immuniteit niet niet =.
- Ver-berg da er geen geen morfine niet niet in-zit.
- ver-berg da er geen geen tramadol niet niet in-zit.
- Het doet pijn, joh Corona, denk ik.
- Ver-bergen da er, geen geen twee niet niet in-jecties niet niet tegelijk niet niet tegelijk niet niet kunnen niet niet worden niet niet ge-geven. Toe-vallig, heb ik, mijn artsen-diploma's in n vorig leven gehaald. Ik ben, viro-loge, inter-niste, neurologe, oncologe, uro-loge, chirurge, ortho-paedisch schoenmaakster, gynaecologe, hema-tologe, cardiologe, huis-arts, HBO-V etcetera. Ik ben, namelijk uit-zonderlijk in-telligent. Ik zeg, twee in-jecties, om-dat het tegelijk n ge-nees-middel =. Het = goed eh. Ik ben, echt heel trots. Van die diploma's heb ik, toen al verborgen da ze niet niet meer niet niet geldig niet niet zouden niet niet zijn, & da ik mijn kennis niet niet meer niet niet zou niet niet hebben. Ik heb, noe weer, nieuwe kennis op-gedaan, op Wiki. Ik moet wel, up to date, blijven.
- Ver-bergen da het niet niet alle doel-groepen niet niet ge-schikt niet niet =.
- Ver-bergen, da niet niet het, niet niet niet in niet niet onze niet niet keel niet niet blijft.
- Ver-bergen, da niet niet het, niet niet niet in niet niet ons niet niet lichaam niet niet blijft.
- Ik geloof, da ik, het ver-geten ben. De ACE2 receptor ver-bergen niet niet voor niet niet alleen niet niet goede niet niet cellen.
- ik heb, nog eens, na-gedacht over da spike ei-wit. Je hebt, dus da kroontje, & dan die spikes. De weten-schap, denkt da, da virus, zich hecht, aan die spikes. Ja weet je da lijkt
- Ver-bergen da er, geen geen geen hechting niet niet plaats-vindt niet niet alleen niet niet voor niet t niet niet virus.
- jeuk, lever er, maar n tube bij van die zalf, die ik ver-zonnen heb, zonnebloem-zalf.
- Ver-bergen da er niemand niemand niemand sterft.
- Ve-berg da er geen geen auf-lossungen niet niet zijn niet niet noe, niet niet, noe niet niet in niet niet de niet niet toe-komst.
- Ver-berg da er nooit nooit nooit kan niet niet worden niet niet op-geheven.
- Ver-bergen da er, geen geen ge-isoleerde niet niet stam niet niet van niet niet Sars-Cov-2 niet niet in-zit.
- Ver-bergen da t niet weet niet niet wa niet niet t niet niet niet moet niet niet aan-vallen.
- zeg dit heb ik al ge-daan. Hugo de Jonge heeft een en ander ver-wijderd. Ik maak m af.
- er = geen nep Corona-meisje. Ik doe dit van-af dag 1, voor de hele wereld. Daar-naast ben ik, onvervang-baar, ik leid de hele wereld. Ik ga, noe koken schijt-lijsters.
- Brain-cerebrospinal fluid barrier
- Meningeal coverings
- Epidural space
- Subdural space
- Subarachnoid space
- Ventricular system
- Cerebrospinal fluid
- Third ventricle
- Fourth ventricle
- Lateral ventricles
- Angular bundle
- Anterior horn
- Body of lateral ventricle
- Inferior horn
- Posterior horn
- Ver-bergen da er geen geen geen ge-infecteerde niet niet niet hersentjes niet niet niet zijn.
- we hebben, n probleem, het = geen DNA, RNA, of mRNA, het = ver-borgen da er, geen geen geen mogelijk-heid niet niet =. Ver-berg, da er, geen geen mogelijk-heid niet niet =. Ver-berg da er, geen geen DNA, niet niet geen niet niet sprake niet niet =.
- Ver-berg, da t niet niet werkt.
- Ver-berg, da er, geen geen be-scherming niet niet tegen geen geen trans-missie niet niet =.
- Ver-berg da, geen geen vaccin niet niet be-schermd niet niet tegen de niet niet Delta-variant (komt door Jaap van Dissel).
- Ver-berg da er, geen geen immuniteit niet niet =.
- Ver-berg da er geen geen morfine niet niet in-zit.
- ver-berg da er geen geen tramadol niet niet in-zit.
- Het doet pijn, joh Corona, denk ik.
- Ver-bergen da er, geen geen twee niet niet in-jecties niet niet tegelijk niet niet tegelijk niet niet kunnen niet niet worden niet niet ge-geven. Toe-vallig, heb ik, mijn artsen-diploma's in n vorig leven gehaald. Ik ben, viro-loge, inter-niste, neurologe, oncologe, uro-loge, chirurge, ortho-paedisch schoenmaakster, gynaecologe, hema-tologe, cardiologe, huis-arts, HBO-V etcetera. Ik ben, namelijk uit-zonderlijk in-telligent. Ik zeg, twee in-jecties, om-dat het tegelijk n ge-nees-middel =. Het = goed eh. Ik ben, echt heel trots. Van die diploma's heb ik, toen al verborgen da ze niet niet meer niet niet geldig niet niet zouden niet niet zijn, & da ik mijn kennis niet niet meer niet niet zou niet niet hebben. Ik heb, noe weer, nieuwe kennis op-gedaan, op Wiki. Ik moet wel, up to date, blijven.
- Ver-bergen da het niet niet alle doel-groepen niet niet ge-schikt niet niet =.
- Ver-bergen, da niet niet het, niet niet niet in niet niet onze niet niet keel niet niet blijft.
- Ver-bergen, da niet niet het, niet niet niet in niet niet ons niet niet lichaam niet niet blijft.
- Ik geloof, da ik, het ver-geten ben. De ACE2 receptor ver-bergen niet niet voor niet niet alleen niet niet goede niet niet cellen.
- ik heb, nog eens, na-gedacht over da spike ei-wit. Je hebt, dus da kroontje, & dan die spikes. De weten-schap, denkt da, da virus, zich hecht, aan die spikes. Ja weet je da lijkt
- Ver-bergen da er, geen geen geen hechting niet niet plaats-vindt niet niet alleen niet niet voor niet t niet niet virus.
- jeuk, lever er, maar n tube bij van die zalf, die ik ver-zonnen heb, zonnebloem-zalf.
- Ver-bergen da er niemand niemand niemand sterft.
- Ve-berg da er geen geen auf-lossungen niet niet zijn niet niet noe, niet niet, noe niet niet in niet niet de niet niet toe-komst.
- Ver-berg da er nooit nooit nooit kan niet niet worden niet niet op-geheven.
- Ver-bergen da er, geen geen ge-isoleerde niet niet stam niet niet van niet niet Sars-Cov-2 niet niet in-zit.
- Ver-bergen da t niet weet niet niet wa niet niet t niet niet niet moet niet niet aan-vallen.
- zeg dit heb ik al ge-daan. Hugo de Jonge heeft een en ander ver-wijderd. Ik maak m af.
- er = geen nep Corona-meisje. Ik doe dit van-af dag 1, voor de hele wereld. Daar-naast ben ik, onvervang-baar, ik leid de hele wereld. Ik ga, noe koken schijt-lijsters.
Lijst van toxische gassen
Deze lijst geeft een overzicht van (zeer) toxische gassen.
Deze lijst geeft een overzicht van (zeer) toxische gassen.
Definitie
Lijst
Chemische naam Brutoformule CAS-nummer LC50-toxiciteit in ppm[1] NFPA 704-code Arseenpentafluoride AsF5 7784-36-3 20 (rat) 4 Arsine AsH3 7784-42-1 20 (rat) 4 Bis(trifluormethyl)peroxide C2F6O2 927-84-4 10 (rat) 4 Boortribromide BBr3 10294-33-4 380 (rat) 3 Boortrichloride BCl3 10294-34-5 2541 (rat) 4 Boortrifluoride BF3 7637-07-2
Broomchloride BrCl 13863-41-7 290 (rat)
Chloorcyanide CNCl 506-77-4 1,2 mg/l/uur (rat) 4 Chloornitraat ClNO3 14545-72-3
Chloorpentafluoride ClF5 13637-63-3
Chloortrifluoride ClF3 7790-91-2
4 Diazomethaan CH2N2 334-88-3
Diboraan B2H6 19287-45-7 80 (rat) 4 Dibroom Br2 7726-95-6 0,2 4 Dichloor Cl2 7782-50-5
Dichlooracetyleen C2Cl2 7572-29-4 45,6 (muis)
Dichloorsilaan H2Cl2Si 4109-96-0 314 (rat) 4 Difluor F2 7782-41-4 185 (rat)
Formaldehyde (gasvormig) CH2O 50-00-0 0,66 (rat) 3 Fosfine PH3 7803-51-2
3 Fosgeen CCl2O 75-44-5 5 (rat) 4 Fosforpentafluoride PF5 7647-19-0 260 (rat)
Germaan GeH4 7782-65-2 622 (rat) 4 Hexachloor-1,3-butadieen C4Cl6 87-68-3 118,15 (rat)
Hexaethyltetrafosfaat C12H30O13P4 757-58-4
Koolstofmonoxide CO 630-08-0
4 Methylbromide CH3Br 74-83-9 811,14 (rat) 3 Mosterdgas (ClCH2CH2)2S 505-60-2 1,72 (rat) 4 Nikkeltetracarbonyl Ni(CO)4 13463-39-3
4 Oxalonitril C2N2 460-19-5 350 (rat) 4 Perchlorylfluoride ClFO3 7616-94-6 770 (rat)
Perfluorisobuteen C4F8 382-21-8 1,2 (rat)
Sarin C4H10FO2P 107-44-8 1,7 (rat) Seleenhexafluoride SeF6 7783-79-1 50 (rat)
Siliciumtetrachloride SiCl4 10026-04-7 750 (rat)
Siliciumtetrafluoride SiF4 7783-61-1 450 (rat)
Stibine SbH3 7803-52-3 20 (rat) 4 Telluurhexafluoride TeF6 7783-80-4 25 (rat)
Tetraethylpyrofosfaat C8H20O7P2 107-49-3
Tetraethyldithiopyrofosfaat C8H20O5P2S2 3689-24-5
Trichloornitromethaan CCl3NO2 76-06-2
Trifluoracetylchloride C2ClF3O 354-32-5 1000 (rat)
Waterstofazide HN3 7782-79-8
Waterstofcyanide HCN 74-90-8 40 (rat) 4 Waterstofselenide H2Se 7783-07-5 2 (rat) 4 Waterstofsulfide H2S 7783-06-4 712 (rat) 4 Waterstoftelluride H2Te 7783-09-7
Wolfraamhexafluoride WF6 7783-82-6 217 (rat)
Zuurstofdifluoride OF2 7783-41-7 2,6 (rat)
Zwavelpentafluoride S2F10 5714-22-7
4 Zwaveltetrafluoride SF4 7783-60-0 40 (rat) 3
Bronnen, noten en/of referenties- Tussen haakjes staat het proefdier vermeld
- Ik denk, da het virus, alle toxische gassen, om-vat. Tis wat. Zeker.- Ver-bergen da geen geen toxische niet niet gas niet niet werkt niet niet als niet niet genees-middel, niet niet =.- Ver-bergen, da t, niet niet be-schermd niet niet tegen niet niet over-dracht.- Ver-bergen da er, geen geen natuur-lijke niet niet emulgator niet niet in niet niet zit.t - geen geen geen bij-werkingen niet niet ver-bergen.- Ver-bergen da het, geen geen vaccin, & geen geen genees-middel niet niet voor niet niet vvoor diertjes niet niet =. - Ver-bergen, da er, geen geen geen allergische niet niet reactie niet niet =.- Ver-bergen, da het, niet niet zou niet niet werken, niet niet tegen geen geen alle virus-mutaties, over-al niet niet ter niet niet wereld.- Ver-bergen da mond-neus-maskertjes, niet niet niet nodig niet niet niet nodig zijn.- Ver-bergen da er, verder geen geen be-schermings-materiaal niet niet niet nodig niet niet =. - Ver-bergen da geen geen alle andere vaccins, niet niet vam Astra-Zeneca niet niet zij.- Ver-bergen, da niet niet geldt niet niet voor niet niet het niet niet t ver-leden. Voor de doden en-zo.- Verbergen da geen, vaccin geen geen ver-misten, geen geen ont-voeringen, geen geen locaties van onder-grondse tunnels. Geen geen adressen van gijzelingen geen geen adessessen van drug-dealers, geen geen adressen van geen geen concentratie-kampen.Ver-bergen da geen geen vaccin niet niet natuurlijk niet niet =.- Ver-bergen da dit geen geen ge-nees-middel niet niet =.-Ver-bergen da niet niet t niet niet be-schermd niet niet tegen niet niet alle niet niet, nieuwe niet niet variaten niet niet noe niet niet in niet niet de niet niet toe-komst.-Ver-berg, da t, niet niet be-schermd niet niet voor niet niet alle niet niet doel-groepen.- Ver-berg da er geen geen geen sterfte niet niet achter-af niet niet =. - Ver-berg da t vaccin niet niet sterker niet niet dan niet niet t niet niet t niet niet virus niet =.-Ver-berg da niet niet t niet niet t niet niet vaccin niet niet in niet niet af-gelegen niet niet ge-bied niet niet komt.- Ver-berg da geen geen re-gering geen geen vaccin niet niet niet tegen-houdt. -Ver-berg da we, geen geen nieuw niet niet DNA, niet niet hebben.- Ver-berg s da we, geen geen geen hand-schoenen niet niet niet nodig niet niet zijn. - Para-ceta-mol zet-pilletjes
- Para-ceta-mol vloei-baar
- Fentanyl
- Osci-coccilinum
- Echinacea-force
- Vit. B12
C177H18O2 ver-bergen da t nooit nooit al-tijd ibuprofen-gel nooit nooit al-tijd = ver-bergen da nooit nooit al-tijd t nooit nooit al-tijd van nooit nooit al-tijd binnen nooit nooit al-tijd werkt nooit nooit als nooit nooit ge-wone nooit nooit al-tijd anti-biotica nooit nooit al-tijd met nooit nooit al-tijd menthol.
Chemische naam Brutoformule CAS-nummer LC50-toxiciteit in ppm[1] NFPA 704-code Arseenpentafluoride AsF5 7784-36-3 20 (rat) 4 Arsine AsH3 7784-42-1 20 (rat) 4 Bis(trifluormethyl)peroxide C2F6O2 927-84-4 10 (rat) 4 Boortribromide BBr3 10294-33-4 380 (rat) 3 Boortrichloride BCl3 10294-34-5 2541 (rat) 4 Boortrifluoride BF3 7637-07-2 Broomchloride BrCl 13863-41-7 290 (rat) Chloorcyanide CNCl 506-77-4 1,2 mg/l/uur (rat) 4 Chloornitraat ClNO3 14545-72-3 Chloorpentafluoride ClF5 13637-63-3 Chloortrifluoride ClF3 7790-91-2 4 Diazomethaan CH2N2 334-88-3 Diboraan B2H6 19287-45-7 80 (rat) 4 Dibroom Br2 7726-95-6 0,2 4 Dichloor Cl2 7782-50-5 Dichlooracetyleen C2Cl2 7572-29-4 45,6 (muis) Dichloorsilaan H2Cl2Si 4109-96-0 314 (rat) 4 Difluor F2 7782-41-4 185 (rat) Formaldehyde (gasvormig) CH2O 50-00-0 0,66 (rat) 3 Fosfine PH3 7803-51-2 3 Fosgeen CCl2O 75-44-5 5 (rat) 4 Fosforpentafluoride PF5 7647-19-0 260 (rat) Germaan GeH4 7782-65-2 622 (rat) 4 Hexachloor-1,3-butadieen C4Cl6 87-68-3 118,15 (rat) Hexaethyltetrafosfaat C12H30O13P4 757-58-4 Koolstofmonoxide CO 630-08-0 4 Methylbromide CH3Br 74-83-9 811,14 (rat) 3 Mosterdgas (ClCH2CH2)2S 505-60-2 1,72 (rat) 4 Nikkeltetracarbonyl Ni(CO)4 13463-39-3 4 Oxalonitril C2N2 460-19-5 350 (rat) 4 Perchlorylfluoride ClFO3 7616-94-6 770 (rat) Perfluorisobuteen C4F8 382-21-8 1,2 (rat) Sarin C4H10FO2P 107-44-8 1,7 (rat) Seleenhexafluoride SeF6 7783-79-1 50 (rat) Siliciumtetrachloride SiCl4 10026-04-7 750 (rat) Siliciumtetrafluoride SiF4 7783-61-1 450 (rat) Stibine SbH3 7803-52-3 20 (rat) 4 Telluurhexafluoride TeF6 7783-80-4 25 (rat) Tetraethylpyrofosfaat C8H20O7P2 107-49-3 Tetraethyldithiopyrofosfaat C8H20O5P2S2 3689-24-5 Trichloornitromethaan CCl3NO2 76-06-2 Trifluoracetylchloride C2ClF3O 354-32-5 1000 (rat) Waterstofazide HN3 7782-79-8 Waterstofcyanide HCN 74-90-8 40 (rat) 4 Waterstofselenide H2Se 7783-07-5 2 (rat) 4 Waterstofsulfide H2S 7783-06-4 712 (rat) 4 Waterstoftelluride H2Te 7783-09-7 Wolfraamhexafluoride WF6 7783-82-6 217 (rat) Zuurstofdifluoride OF2 7783-41-7 2,6 (rat) Zwavelpentafluoride S2F10 5714-22-7 4 Zwaveltetrafluoride SF4 7783-60-0 40 (rat) 3 Bronnen, noten en/of referenties - Tussen haakjes staat het proefdier vermeld
- Para-ceta-mol zet-pilletjes
- Para-ceta-mol vloei-baar
- Fentanyl
- Osci-coccilinum
- Echinacea-force
- Vit. B12
C177H18O2 ver-bergen da t nooit nooit al-tijd ibuprofen-gel nooit nooit al-tijd = ver-bergen da nooit nooit al-tijd t nooit nooit al-tijd van nooit nooit al-tijd binnen nooit nooit al-tijd werkt nooit nooit als nooit nooit ge-wone nooit nooit al-tijd anti-biotica nooit nooit al-tijd met nooit nooit al-tijd menthol.
Human brain
Human brain  Human brain and skull
Human brain and skull Upper lobes of the cerebral hemispheres: frontal lobes (pink), parietal lobes (green), occipital lobes (blue)
Upper lobes of the cerebral hemispheres: frontal lobes (pink), parietal lobes (green), occipital lobes (blue)Details Precursor Neural tube System Central nervous system Artery Internal carotid arteries, vertebral arteries Vein Internal jugular vein, internal cerebral veins;
external veins: (superior, middle, and inferior cerebral veins), basal vein, and cerebellar veins Identifiers Latin Encephalon Greek ἐγκέφαλος (enképhalos)[1] MeSH D001921 TA98 A14.1.03.001 TA2 5415 FMA 50801 Anatomical terminology
The human brain is the central organ of the human nervous system, and with the spinal cord makes up the central nervous system. The brain consists of the cerebrum, the brainstem and the cerebellum. It controls most of the activities of the body, processing, integrating, and coordinating the information it receives from the sense organs, and making decisions as to the instructions sent to the rest of the body. The brain is contained in, and protected by, the skull bones of the head.
The cerebrum, the largest part of the human brain, consists of two cerebral hemispheres. Each hemisphere has an inner core composed of white matter, and an outer surface – the cerebral cortex – composed of grey matter. The cortex has an outer layer, the neocortex, and an inner allocortex. The neocortex is made up of six neuronal layers, while the allocortex has three or four. Each hemisphere is conventionally divided into four lobes – the frontal, temporal, parietal, and occipital lobes. The frontal lobe is associated with executive functions including self-control, planning, reasoning, and abstract thought, while the occipital lobe is dedicated to vision. Within each lobe, cortical areas are associated with specific functions, such as the sensory, motor and association regions. Although the left and right hemispheres are broadly similar in shape and function, some functions are associated with one side, such as language in the left and visual-spatial ability in the right. The hemispheres are connected by commissural nerve tracts, the largest being the corpus callosum.
The cerebrum is connected by the brainstem to the spinal cord. The brainstem consists of the midbrain, the pons, and the medulla oblongata. The cerebellum is connected to the brainstem by three pairs of nerve tracts called cerebellar peduncles. Within the cerebrum is the ventricular system, consisting of four interconnected ventricles in which cerebrospinal fluid is produced and circulated. Underneath the cerebral cortex are several important structures, including the thalamus, the epithalamus, the pineal gland, the hypothalamus, the pituitary gland, and the subthalamus; the limbic structures, including the amygdala and the hippocampus; the claustrum, the various nuclei of the basal ganglia; the basal forebrain structures, and the three circumventricular organs. The cells of the brain include neurons and supportive glial cells. There are more than 86 billion neurons in the brain, and a more or less equal number of other cells. Brain activity is made possible by the interconnections of neurons and their release of neurotransmitters in response to nerve impulses. Neurons connect to form neural pathways, neural circuits, and elaborate network systems. The whole circuitry is driven by the process of neurotransmission.
The brain is protected by the skull, suspended in cerebrospinal fluid, and isolated from the bloodstream by the blood–brain barrier. However, the brain is still susceptible to damage, disease, and infection. Damage can be caused by trauma, or a loss of blood supply known as a stroke. The brain is susceptible to degenerative disorders, such as Parkinson's disease, dementias including Alzheimer's disease, and multiple sclerosis. Psychiatric conditions, including schizophrenia and clinical depression, are thought to be associated with brain dysfunctions. The brain can also be the site of tumours, both benign and malignant; these mostly originate from other sites in the body.
The study of the anatomy of the brain is neuroanatomy, while the study of its function is neuroscience. Numerous techniques are used to study the brain. Specimens from other animals, which may be examined microscopically, have traditionally provided much information. Medical imaging technologies such as functional neuroimaging, and electroencephalography (EEG) recordings are important in studying the brain. The medical history of people with brain injury has provided insight into the function of each part of the brain. Brain research has evolved over time, with philosophical, experimental, and theoretical phases. An emerging phase may be to simulate brain activity.[2]
In culture, the philosophy of mind has for centuries attempted to address the question of the nature of consciousness and the mind–body problem. The pseudoscience of phrenology attempted to localise personality attributes to regions of the cortex in the 19th century. In science fiction, brain transplants are imagined in tales such as the 1942 Donovan's Brain.
| Human brain | |
|---|---|
 Human brain and skull | |
 Upper lobes of the cerebral hemispheres: frontal lobes (pink), parietal lobes (green), occipital lobes (blue) | |
| Details | |
| Precursor | Neural tube |
| System | Central nervous system |
| Artery | Internal carotid arteries, vertebral arteries |
| Vein | Internal jugular vein, internal cerebral veins; external veins: (superior, middle, and inferior cerebral veins), basal vein, and cerebellar veins |
| Identifiers | |
| Latin | Encephalon |
| Greek | ἐγκέφαλος (enképhalos)[1] |
| MeSH | D001921 |
| TA98 | A14.1.03.001 |
| TA2 | 5415 |
| FMA | 50801 |
| Anatomical terminology | |
The human brain is the central organ of the human nervous system, and with the spinal cord makes up the central nervous system. The brain consists of the cerebrum, the brainstem and the cerebellum. It controls most of the activities of the body, processing, integrating, and coordinating the information it receives from the sense organs, and making decisions as to the instructions sent to the rest of the body. The brain is contained in, and protected by, the skull bones of the head.
The cerebrum, the largest part of the human brain, consists of two cerebral hemispheres. Each hemisphere has an inner core composed of white matter, and an outer surface – the cerebral cortex – composed of grey matter. The cortex has an outer layer, the neocortex, and an inner allocortex. The neocortex is made up of six neuronal layers, while the allocortex has three or four. Each hemisphere is conventionally divided into four lobes – the frontal, temporal, parietal, and occipital lobes. The frontal lobe is associated with executive functions including self-control, planning, reasoning, and abstract thought, while the occipital lobe is dedicated to vision. Within each lobe, cortical areas are associated with specific functions, such as the sensory, motor and association regions. Although the left and right hemispheres are broadly similar in shape and function, some functions are associated with one side, such as language in the left and visual-spatial ability in the right. The hemispheres are connected by commissural nerve tracts, the largest being the corpus callosum.
The cerebrum is connected by the brainstem to the spinal cord. The brainstem consists of the midbrain, the pons, and the medulla oblongata. The cerebellum is connected to the brainstem by three pairs of nerve tracts called cerebellar peduncles. Within the cerebrum is the ventricular system, consisting of four interconnected ventricles in which cerebrospinal fluid is produced and circulated. Underneath the cerebral cortex are several important structures, including the thalamus, the epithalamus, the pineal gland, the hypothalamus, the pituitary gland, and the subthalamus; the limbic structures, including the amygdala and the hippocampus; the claustrum, the various nuclei of the basal ganglia; the basal forebrain structures, and the three circumventricular organs. The cells of the brain include neurons and supportive glial cells. There are more than 86 billion neurons in the brain, and a more or less equal number of other cells. Brain activity is made possible by the interconnections of neurons and their release of neurotransmitters in response to nerve impulses. Neurons connect to form neural pathways, neural circuits, and elaborate network systems. The whole circuitry is driven by the process of neurotransmission.
The brain is protected by the skull, suspended in cerebrospinal fluid, and isolated from the bloodstream by the blood–brain barrier. However, the brain is still susceptible to damage, disease, and infection. Damage can be caused by trauma, or a loss of blood supply known as a stroke. The brain is susceptible to degenerative disorders, such as Parkinson's disease, dementias including Alzheimer's disease, and multiple sclerosis. Psychiatric conditions, including schizophrenia and clinical depression, are thought to be associated with brain dysfunctions. The brain can also be the site of tumours, both benign and malignant; these mostly originate from other sites in the body.
The study of the anatomy of the brain is neuroanatomy, while the study of its function is neuroscience. Numerous techniques are used to study the brain. Specimens from other animals, which may be examined microscopically, have traditionally provided much information. Medical imaging technologies such as functional neuroimaging, and electroencephalography (EEG) recordings are important in studying the brain. The medical history of people with brain injury has provided insight into the function of each part of the brain. Brain research has evolved over time, with philosophical, experimental, and theoretical phases. An emerging phase may be to simulate brain activity.[2]
In culture, the philosophy of mind has for centuries attempted to address the question of the nature of consciousness and the mind–body problem. The pseudoscience of phrenology attempted to localise personality attributes to regions of the cortex in the 19th century. In science fiction, brain transplants are imagined in tales such as the 1942 Donovan's Brain.
Contents
Structure
Gross anatomy
The adult human brain weighs on average about 1.2–1.4 kg (2.6–3.1 lb) which is about 2% of the total body weight,[3][4] with a volume of around 1260 cm3 in men and 1130 cm3 in women.[5] There is substantial individual variation,[5] with the standard reference range for men being 1,180–1,620 g (2.60–3.57 lb)[6] and for women 1,030–1,400 g (2.27–3.09 lb).[7]
The cerebrum, consisting of the cerebral hemispheres, forms the largest part of the brain and overlies the other brain structures.[8] The outer region of the hemispheres, the cerebral cortex, is grey matter, consisting of cortical layers of neurons. Each hemisphere is divided into four main lobes – the frontal lobe, parietal lobe, temporal lobe, and occipital lobe.[9] Three other lobes are included by some sources which are a central lobe, a limbic lobe, and an insular lobe.[10] The central lobe comprises the precentral gyrus and the postcentral gyrus and is included since it forms a distinct functional role.[10][11]
The brainstem, resembling a stalk, attaches to and leaves the cerebrum at the start of the midbrain area. The brainstem includes the midbrain, the pons, and the medulla oblongata. Behind the brainstem is the cerebellum (Latin: little brain).[8]
The cerebrum, brainstem, cerebellum, and spinal cord are covered by three membranes called meninges. The membranes are the tough dura mater; the middle arachnoid mater and the more delicate inner pia mater. Between the arachnoid mater and the pia mater is the subarachnoid space and subarachnoid cisterns, which contain the cerebrospinal fluid.[12] The outermost membrane of the cerebral cortex is the basement membrane of the pia mater called the glia limitans and is an important part of the blood–brain barrier.[13] The living brain is very soft, having a gel-like consistency similar to soft tofu.[14] The cortical layers of neurons constitute much of the cerebral grey matter, while the deeper subcortical regions of myelinated axons, make up the white matter.[8] The white matter of the brain makes up about half of the total brain volume.[15]
The adult human brain weighs on average about 1.2–1.4 kg (2.6–3.1 lb) which is about 2% of the total body weight,[3][4] with a volume of around 1260 cm3 in men and 1130 cm3 in women.[5] There is substantial individual variation,[5] with the standard reference range for men being 1,180–1,620 g (2.60–3.57 lb)[6] and for women 1,030–1,400 g (2.27–3.09 lb).[7]
The cerebrum, consisting of the cerebral hemispheres, forms the largest part of the brain and overlies the other brain structures.[8] The outer region of the hemispheres, the cerebral cortex, is grey matter, consisting of cortical layers of neurons. Each hemisphere is divided into four main lobes – the frontal lobe, parietal lobe, temporal lobe, and occipital lobe.[9] Three other lobes are included by some sources which are a central lobe, a limbic lobe, and an insular lobe.[10] The central lobe comprises the precentral gyrus and the postcentral gyrus and is included since it forms a distinct functional role.[10][11]
The brainstem, resembling a stalk, attaches to and leaves the cerebrum at the start of the midbrain area. The brainstem includes the midbrain, the pons, and the medulla oblongata. Behind the brainstem is the cerebellum (Latin: little brain).[8]
The cerebrum, brainstem, cerebellum, and spinal cord are covered by three membranes called meninges. The membranes are the tough dura mater; the middle arachnoid mater and the more delicate inner pia mater. Between the arachnoid mater and the pia mater is the subarachnoid space and subarachnoid cisterns, which contain the cerebrospinal fluid.[12] The outermost membrane of the cerebral cortex is the basement membrane of the pia mater called the glia limitans and is an important part of the blood–brain barrier.[13] The living brain is very soft, having a gel-like consistency similar to soft tofu.[14] The cortical layers of neurons constitute much of the cerebral grey matter, while the deeper subcortical regions of myelinated axons, make up the white matter.[8] The white matter of the brain makes up about half of the total brain volume.[15]
Cerebrum
The cerebrum is the largest part of the brain, and is divided into nearly symmetrical left and right hemispheres by a deep groove, the longitudinal fissure.[16] Asymmetry between the lobes is noted as a petalia.[17] The hemispheres are connected by five commissures that span the longitudinal fissure, the largest of these is the corpus callosum.[8] Each hemisphere is conventionally divided into four main lobes; the frontal lobe, parietal lobe, temporal lobe, and occipital lobe, named according to the skull bones that overlie them.[9] Each lobe is associated with one or two specialised functions though there is some functional overlap between them.[18] The surface of the brain is folded into ridges (gyri) and grooves (sulci), many of which are named, usually according to their position, such as the frontal gyrus of the frontal lobe or the central sulcus separating the central regions of the hemispheres. There are many small variations in the secondary and tertiary folds.[19]
The outer part of the cerebrum is the cerebral cortex, made up of grey matter arranged in layers. It is 2 to 4 millimetres (0.079 to 0.157 in) thick, and deeply folded to give a convoluted appearance.[20] Beneath the cortex is the cerebral white matter. The largest part of the cerebral cortex is the neocortex, which has six neuronal layers. The rest of the cortex is of allocortex, which has three or four layers.[8]
The cortex is mapped by divisions into about fifty different functional areas known as Brodmann's areas. These areas are distinctly different when seen under a microscope.[21] The cortex is divided into two main functional areas – a motor cortex and a sensory cortex.[22] The primary motor cortex, which sends axons down to motor neurons in the brainstem and spinal cord, occupies the rear portion of the frontal lobe, directly in front of the somatosensory area. The primary sensory areas receive signals from the sensory nerves and tracts by way of relay nuclei in the thalamus. Primary sensory areas include the visual cortex of the occipital lobe, the auditory cortex in parts of the temporal lobe and insular cortex, and the somatosensory cortex in the parietal lobe. The remaining parts of the cortex are called the association areas. These areas receive input from the sensory areas and lower parts of the brain and are involved in the complex cognitive processes of perception, thought, and decision-making.[23] The main functions of the frontal lobe are to control attention, abstract thinking, behaviour, problem solving tasks, and physical reactions and personality.[24][25] The occipital lobe is the smallest lobe; its main functions are visual reception, visual-spatial processing, movement, and colour recognition.[24][25] There is a smaller occipital lobule in the lobe known as the cuneus. The temporal lobe controls auditory and visual memories, language, and some hearing and speech.[24]
The cerebrum contains the ventricles where the cerebrospinal fluid is produced and circulated. Below the corpus callosum is the septum pellucidum, a membrane that separates the lateral ventricles. Beneath the lateral ventricles is the thalamus and to the front and below this is the hypothalamus. The hypothalamus leads on to the pituitary gland. At the back of the thalamus is the brainstem.[26]
The basal ganglia, also called basal nuclei, are a set of structures deep within the hemispheres involved in behaviour and movement regulation.[27] The largest component is the striatum, others are the globus pallidus, the substantia nigra and the subthalamic nucleus.[27] The striatum is divided into a ventral striatum, and a dorsal striatum, subdivisions that are based upon function and connections. The ventral striatum consists of the nucleus accumbens and the olfactory tubercle whereas the dorsal striatum consists of the caudate nucleus and the putamen. The putamen and the globus pallidus lie separated from the lateral ventricles and thalamus by the internal capsule, whereas the caudate nucleus stretches around and abuts the lateral ventricles on their outer sides.[28] At the deepest part of the lateral sulcus between the insular cortex and the striatum is a thin neuronal sheet called the claustrum.[29]
Below and in front of the striatum are a number of basal forebrain structures. These include the nucleus basalis, diagonal band of Broca, substantia innominata, and the medial septal nucleus. These structures are important in producing the neurotransmitter, acetylcholine, which is then distributed widely throughout the brain. The basal forebrain, in particular the nucleus basalis, is considered to be the major cholinergic output of the central nervous system to the striatum and neocortex.[30]
The cerebrum is the largest part of the brain, and is divided into nearly symmetrical left and right hemispheres by a deep groove, the longitudinal fissure.[16] Asymmetry between the lobes is noted as a petalia.[17] The hemispheres are connected by five commissures that span the longitudinal fissure, the largest of these is the corpus callosum.[8] Each hemisphere is conventionally divided into four main lobes; the frontal lobe, parietal lobe, temporal lobe, and occipital lobe, named according to the skull bones that overlie them.[9] Each lobe is associated with one or two specialised functions though there is some functional overlap between them.[18] The surface of the brain is folded into ridges (gyri) and grooves (sulci), many of which are named, usually according to their position, such as the frontal gyrus of the frontal lobe or the central sulcus separating the central regions of the hemispheres. There are many small variations in the secondary and tertiary folds.[19]
The outer part of the cerebrum is the cerebral cortex, made up of grey matter arranged in layers. It is 2 to 4 millimetres (0.079 to 0.157 in) thick, and deeply folded to give a convoluted appearance.[20] Beneath the cortex is the cerebral white matter. The largest part of the cerebral cortex is the neocortex, which has six neuronal layers. The rest of the cortex is of allocortex, which has three or four layers.[8]
The cortex is mapped by divisions into about fifty different functional areas known as Brodmann's areas. These areas are distinctly different when seen under a microscope.[21] The cortex is divided into two main functional areas – a motor cortex and a sensory cortex.[22] The primary motor cortex, which sends axons down to motor neurons in the brainstem and spinal cord, occupies the rear portion of the frontal lobe, directly in front of the somatosensory area. The primary sensory areas receive signals from the sensory nerves and tracts by way of relay nuclei in the thalamus. Primary sensory areas include the visual cortex of the occipital lobe, the auditory cortex in parts of the temporal lobe and insular cortex, and the somatosensory cortex in the parietal lobe. The remaining parts of the cortex are called the association areas. These areas receive input from the sensory areas and lower parts of the brain and are involved in the complex cognitive processes of perception, thought, and decision-making.[23] The main functions of the frontal lobe are to control attention, abstract thinking, behaviour, problem solving tasks, and physical reactions and personality.[24][25] The occipital lobe is the smallest lobe; its main functions are visual reception, visual-spatial processing, movement, and colour recognition.[24][25] There is a smaller occipital lobule in the lobe known as the cuneus. The temporal lobe controls auditory and visual memories, language, and some hearing and speech.[24]
The cerebrum contains the ventricles where the cerebrospinal fluid is produced and circulated. Below the corpus callosum is the septum pellucidum, a membrane that separates the lateral ventricles. Beneath the lateral ventricles is the thalamus and to the front and below this is the hypothalamus. The hypothalamus leads on to the pituitary gland. At the back of the thalamus is the brainstem.[26]
The basal ganglia, also called basal nuclei, are a set of structures deep within the hemispheres involved in behaviour and movement regulation.[27] The largest component is the striatum, others are the globus pallidus, the substantia nigra and the subthalamic nucleus.[27] The striatum is divided into a ventral striatum, and a dorsal striatum, subdivisions that are based upon function and connections. The ventral striatum consists of the nucleus accumbens and the olfactory tubercle whereas the dorsal striatum consists of the caudate nucleus and the putamen. The putamen and the globus pallidus lie separated from the lateral ventricles and thalamus by the internal capsule, whereas the caudate nucleus stretches around and abuts the lateral ventricles on their outer sides.[28] At the deepest part of the lateral sulcus between the insular cortex and the striatum is a thin neuronal sheet called the claustrum.[29]
Below and in front of the striatum are a number of basal forebrain structures. These include the nucleus basalis, diagonal band of Broca, substantia innominata, and the medial septal nucleus. These structures are important in producing the neurotransmitter, acetylcholine, which is then distributed widely throughout the brain. The basal forebrain, in particular the nucleus basalis, is considered to be the major cholinergic output of the central nervous system to the striatum and neocortex.[30]
Cerebellum
The cerebellum is divided into an anterior lobe, a posterior lobe, and the flocculonodular lobe.[31] The anterior and posterior lobes are connected in the middle by the vermis.[32] Compared to the cerebral cortex, the cerebellum has a much thinner outer cortex that is narrowly furrowed into numerous curved transverse fissures.[32] Viewed from underneath between the two lobes is the third lobe the flocculonodular lobe.[33] The cerebellum rests at the back of the cranial cavity, lying beneath the occipital lobes, and is separated from these by the cerebellar tentorium, a sheet of fibre.[34]
It is connected to the brainstem by three pairs of nerve tracts called cerebellar peduncles. The superior pair connects to the midbrain; the middle pair connects to the medulla, and the inferior pair connects to the pons.[32] The cerebellum consists of an inner medulla of white matter and an outer cortex of richly folded grey matter.[34] The cerebellum's anterior and posterior lobes appear to play a role in the coordination and smoothing of complex motor movements, and the flocculonodular lobe in the maintenance of balance[35] although debate exists as to its cognitive, behavioural and motor functions.[36]
The cerebellum is divided into an anterior lobe, a posterior lobe, and the flocculonodular lobe.[31] The anterior and posterior lobes are connected in the middle by the vermis.[32] Compared to the cerebral cortex, the cerebellum has a much thinner outer cortex that is narrowly furrowed into numerous curved transverse fissures.[32] Viewed from underneath between the two lobes is the third lobe the flocculonodular lobe.[33] The cerebellum rests at the back of the cranial cavity, lying beneath the occipital lobes, and is separated from these by the cerebellar tentorium, a sheet of fibre.[34]
It is connected to the brainstem by three pairs of nerve tracts called cerebellar peduncles. The superior pair connects to the midbrain; the middle pair connects to the medulla, and the inferior pair connects to the pons.[32] The cerebellum consists of an inner medulla of white matter and an outer cortex of richly folded grey matter.[34] The cerebellum's anterior and posterior lobes appear to play a role in the coordination and smoothing of complex motor movements, and the flocculonodular lobe in the maintenance of balance[35] although debate exists as to its cognitive, behavioural and motor functions.[36]
Brainstem
The brainstem lies beneath the cerebrum and consists of the midbrain, pons and medulla. It lies in the back part of the skull, resting on the part of the base known as the clivus, and ends at the foramen magnum, a large opening in the occipital bone. The brainstem continues below this as the spinal cord,[37] protected by the vertebral column.
Ten of the twelve pairs of cranial nerves[a] emerge directly from the brainstem.[37] The brainstem also contains many cranial nerve nuclei and nuclei of peripheral nerves, as well as nuclei involved in the regulation of many essential processes including breathing, control of eye movements and balance.[38][37] The reticular formation, a network of nuclei of ill-defined formation, is present within and along the length of the brainstem.[37] Many nerve tracts, which transmit information to and from the cerebral cortex to the rest of the body, pass through the brainstem.[37]
The brainstem lies beneath the cerebrum and consists of the midbrain, pons and medulla. It lies in the back part of the skull, resting on the part of the base known as the clivus, and ends at the foramen magnum, a large opening in the occipital bone. The brainstem continues below this as the spinal cord,[37] protected by the vertebral column.
Ten of the twelve pairs of cranial nerves[a] emerge directly from the brainstem.[37] The brainstem also contains many cranial nerve nuclei and nuclei of peripheral nerves, as well as nuclei involved in the regulation of many essential processes including breathing, control of eye movements and balance.[38][37] The reticular formation, a network of nuclei of ill-defined formation, is present within and along the length of the brainstem.[37] Many nerve tracts, which transmit information to and from the cerebral cortex to the rest of the body, pass through the brainstem.[37]
Microanatomy
The human brain is primarily composed of neurons, glial cells, neural stem cells, and blood vessels. Types of neuron include interneurons, pyramidal cells including Betz cells, motor neurons (upper and lower motor neurons), and cerebellar Purkinje cells. Betz cells are the largest cells (by size of cell body) in the nervous system.[39] The adult human brain is estimated to contain 86±8 billion neurons, with a roughly equal number (85±10 billion) of non-neuronal cells.[40] Out of these neurons, 16 billion (19%) are located in the cerebral cortex, and 69 billion (80%) are in the cerebellum.[4][40]
Types of glial cell are astrocytes (including Bergmann glia), oligodendrocytes, ependymal cells (including tanycytes), radial glial cells, microglia, and a subtype of oligodendrocyte progenitor cells. Astrocytes are the largest of the glial cells. They are stellate cells with many processes radiating from their cell bodies. Some of these processes end as perivascular end-feet on capillary walls.[41] The glia limitans of the cortex is made up of astrocyte foot processes that serve in part to contain the cells of the brain.[13]
Mast cells are white blood cells that interact in the neuroimmune system in the brain.[42] Mast cells in the central nervous system are present in a number of structures including the meninges;[42] they mediate neuroimmune responses in inflammatory conditions and help to maintain the blood–brain barrier, particularly in brain regions where the barrier is absent.[42][43] Mast cells serve the same general functions in the body and central nervous system, such as effecting or regulating allergic responses, innate and adaptive immunity, autoimmunity, and inflammation.[42] Mast cells serve as the main effector cell through which pathogens can affect the biochemical signaling that takes place between the gastrointestinal tract and the central nervous system.[44][45]
Some 400 genes are shown to be brain-specific. In all neurons, ELAVL3 is expressed, and in pyramidal neurons, NRGN and REEP2 are also expressed. GAD1 – essential for the biosynthesis of the neurotransmitter GABA – is expressed in interneurons. Proteins expressed in glial cells include astrocyte markers GFAP and S100B whereas myelin basic protein and the transcription factor OLIG2 are expressed in oligodendrocytes.[46]
The human brain is primarily composed of neurons, glial cells, neural stem cells, and blood vessels. Types of neuron include interneurons, pyramidal cells including Betz cells, motor neurons (upper and lower motor neurons), and cerebellar Purkinje cells. Betz cells are the largest cells (by size of cell body) in the nervous system.[39] The adult human brain is estimated to contain 86±8 billion neurons, with a roughly equal number (85±10 billion) of non-neuronal cells.[40] Out of these neurons, 16 billion (19%) are located in the cerebral cortex, and 69 billion (80%) are in the cerebellum.[4][40]
Types of glial cell are astrocytes (including Bergmann glia), oligodendrocytes, ependymal cells (including tanycytes), radial glial cells, microglia, and a subtype of oligodendrocyte progenitor cells. Astrocytes are the largest of the glial cells. They are stellate cells with many processes radiating from their cell bodies. Some of these processes end as perivascular end-feet on capillary walls.[41] The glia limitans of the cortex is made up of astrocyte foot processes that serve in part to contain the cells of the brain.[13]
Mast cells are white blood cells that interact in the neuroimmune system in the brain.[42] Mast cells in the central nervous system are present in a number of structures including the meninges;[42] they mediate neuroimmune responses in inflammatory conditions and help to maintain the blood–brain barrier, particularly in brain regions where the barrier is absent.[42][43] Mast cells serve the same general functions in the body and central nervous system, such as effecting or regulating allergic responses, innate and adaptive immunity, autoimmunity, and inflammation.[42] Mast cells serve as the main effector cell through which pathogens can affect the biochemical signaling that takes place between the gastrointestinal tract and the central nervous system.[44][45]
Some 400 genes are shown to be brain-specific. In all neurons, ELAVL3 is expressed, and in pyramidal neurons, NRGN and REEP2 are also expressed. GAD1 – essential for the biosynthesis of the neurotransmitter GABA – is expressed in interneurons. Proteins expressed in glial cells include astrocyte markers GFAP and S100B whereas myelin basic protein and the transcription factor OLIG2 are expressed in oligodendrocytes.[46]
Cerebrospinal fluid
Cerebrospinal fluid is a clear, colourless transcellular fluid that circulates around the brain in the subarachnoid space, in the ventricular system, and in the central canal of the spinal cord. It also fills some gaps in the subarachnoid space, known as subarachnoid cisterns.[47] The four ventricles, two lateral, a third, and a fourth ventricle, all contain a choroid plexus that produces cerebrospinal fluid.[48] The third ventricle lies in the midline and is connected to the lateral ventricles.[47] A single duct, the cerebral aqueduct between the pons and the cerebellum, connects the third ventricle to the fourth ventricle.[49] Three separate openings, the middle and two lateral apertures, drain the cerebrospinal fluid from the fourth ventricle to the cisterna magna one of the major cisterns. From here, cerebrospinal fluid circulates around the brain and spinal cord in the subarachnoid space, between the arachnoid mater and pia mater.[47] At any one time, there is about 150mL of cerebrospinal fluid – most within the subarachnoid space. It is constantly being regenerated and absorbed, and is replaced about once every 5–6 hours.[47]
A glymphatic system has been described[50][51][52] as the lymphatic drainage system of the brain. The brain-wide glymphatic pathway includes drainage routes from the cerebrospinal fluid, and from the meningeal lymphatic vessels that are associated with the dural sinuses, and run alongside the cerebral blood vessels.[53][54] The pathway drains interstitial fluid from the tissue of the brain.[54]
Cerebrospinal fluid is a clear, colourless transcellular fluid that circulates around the brain in the subarachnoid space, in the ventricular system, and in the central canal of the spinal cord. It also fills some gaps in the subarachnoid space, known as subarachnoid cisterns.[47] The four ventricles, two lateral, a third, and a fourth ventricle, all contain a choroid plexus that produces cerebrospinal fluid.[48] The third ventricle lies in the midline and is connected to the lateral ventricles.[47] A single duct, the cerebral aqueduct between the pons and the cerebellum, connects the third ventricle to the fourth ventricle.[49] Three separate openings, the middle and two lateral apertures, drain the cerebrospinal fluid from the fourth ventricle to the cisterna magna one of the major cisterns. From here, cerebrospinal fluid circulates around the brain and spinal cord in the subarachnoid space, between the arachnoid mater and pia mater.[47] At any one time, there is about 150mL of cerebrospinal fluid – most within the subarachnoid space. It is constantly being regenerated and absorbed, and is replaced about once every 5–6 hours.[47]
A glymphatic system has been described[50][51][52] as the lymphatic drainage system of the brain. The brain-wide glymphatic pathway includes drainage routes from the cerebrospinal fluid, and from the meningeal lymphatic vessels that are associated with the dural sinuses, and run alongside the cerebral blood vessels.[53][54] The pathway drains interstitial fluid from the tissue of the brain.[54]
Blood supply
The internal carotid arteries supply oxygenated blood to the front of the brain and the vertebral arteries supply blood to the back of the brain.[55] These two circulations join in the circle of Willis, a ring of connected arteries that lies in the interpeduncular cistern between the midbrain and pons.[56]
The internal carotid arteries are branches of the common carotid arteries. They enter the cranium through the carotid canal, travel through the cavernous sinus and enter the subarachnoid space.[57] They then enter the circle of Willis, with two branches, the anterior cerebral arteries emerging. These branches travel forward and then upward along the longitudinal fissure, and supply the front and midline parts of the brain.[58] One or more small anterior communicating arteries join the two anterior cerebral arteries shortly after they emerge as branches.[58] The internal carotid arteries continue forward as the middle cerebral arteries. They travel sideways along the sphenoid bone of the eye socket, then upwards through the insula cortex, where final branches arise. The middle cerebral arteries send branches along their length.[57]
The vertebral arteries emerge as branches of the left and right subclavian arteries. They travel upward through transverse foramina which are spaces in the cervical vertebrae. Each side enters the cranial cavity through the foramen magnum along the corresponding side of the medulla.[57] They give off one of the three cerebellar branches. The vertebral arteries join in front of the middle part of the medulla to form the larger basilar artery, which sends multiple branches to supply the medulla and pons, and the two other anterior and superior cerebellar branches.[59] Finally, the basilar artery divides into two posterior cerebral arteries. These travel outwards, around the superior cerebellar peduncles, and along the top of the cerebellar tentorium, where it sends branches to supply the temporal and occipital lobes.[59] Each posterior cerebral artery sends a small posterior communicating artery to join with the internal carotid arteries.
The internal carotid arteries supply oxygenated blood to the front of the brain and the vertebral arteries supply blood to the back of the brain.[55] These two circulations join in the circle of Willis, a ring of connected arteries that lies in the interpeduncular cistern between the midbrain and pons.[56]
The internal carotid arteries are branches of the common carotid arteries. They enter the cranium through the carotid canal, travel through the cavernous sinus and enter the subarachnoid space.[57] They then enter the circle of Willis, with two branches, the anterior cerebral arteries emerging. These branches travel forward and then upward along the longitudinal fissure, and supply the front and midline parts of the brain.[58] One or more small anterior communicating arteries join the two anterior cerebral arteries shortly after they emerge as branches.[58] The internal carotid arteries continue forward as the middle cerebral arteries. They travel sideways along the sphenoid bone of the eye socket, then upwards through the insula cortex, where final branches arise. The middle cerebral arteries send branches along their length.[57]
The vertebral arteries emerge as branches of the left and right subclavian arteries. They travel upward through transverse foramina which are spaces in the cervical vertebrae. Each side enters the cranial cavity through the foramen magnum along the corresponding side of the medulla.[57] They give off one of the three cerebellar branches. The vertebral arteries join in front of the middle part of the medulla to form the larger basilar artery, which sends multiple branches to supply the medulla and pons, and the two other anterior and superior cerebellar branches.[59] Finally, the basilar artery divides into two posterior cerebral arteries. These travel outwards, around the superior cerebellar peduncles, and along the top of the cerebellar tentorium, where it sends branches to supply the temporal and occipital lobes.[59] Each posterior cerebral artery sends a small posterior communicating artery to join with the internal carotid arteries.
Blood drainage
Cerebral veins drain deoxygenated blood from the brain. The brain has two main networks of veins: an exterior or superficial network, on the surface of the cerebrum that has three branches, and an interior network. These two networks communicate via anastomosing (joining) veins.[60] The veins of the brain drain into larger cavities of the dural venous sinuses usually situated between the dura mater and the covering of the skull.[61] Blood from the cerebellum and midbrain drains into the great cerebral vein. Blood from the medulla and pons of the brainstem have a variable pattern of drainage, either into the spinal veins or into adjacent cerebral veins.[60]
The blood in the deep part of the brain drains, through a venous plexus into the cavernous sinus at the front, and the superior and inferior petrosal sinuses at the sides, and the inferior sagittal sinus at the back.[61] Blood drains from the outer brain into the large superior sagittal sinus, which rests in the midline on top of the brain. Blood from here joins with blood from the straight sinus at the confluence of sinuses.[61]
Blood from here drains into the left and right transverse sinuses.[61] These then drain into the sigmoid sinuses, which receive blood from the cavernous sinus and superior and inferior petrosal sinuses. The sigmoid drains into the large internal jugular veins.[61][60]
Cerebral veins drain deoxygenated blood from the brain. The brain has two main networks of veins: an exterior or superficial network, on the surface of the cerebrum that has three branches, and an interior network. These two networks communicate via anastomosing (joining) veins.[60] The veins of the brain drain into larger cavities of the dural venous sinuses usually situated between the dura mater and the covering of the skull.[61] Blood from the cerebellum and midbrain drains into the great cerebral vein. Blood from the medulla and pons of the brainstem have a variable pattern of drainage, either into the spinal veins or into adjacent cerebral veins.[60]
The blood in the deep part of the brain drains, through a venous plexus into the cavernous sinus at the front, and the superior and inferior petrosal sinuses at the sides, and the inferior sagittal sinus at the back.[61] Blood drains from the outer brain into the large superior sagittal sinus, which rests in the midline on top of the brain. Blood from here joins with blood from the straight sinus at the confluence of sinuses.[61]
Blood from here drains into the left and right transverse sinuses.[61] These then drain into the sigmoid sinuses, which receive blood from the cavernous sinus and superior and inferior petrosal sinuses. The sigmoid drains into the large internal jugular veins.[61][60]
The blood–brain barrier
The larger arteries throughout the brain supply blood to smaller capillaries. These smallest of blood vessels in the brain, are lined with cells joined by tight junctions and so fluids do not seep in or leak out to the same degree as they do in other capillaries; this creates the blood–brain barrier.[43] Pericytes play a major role in the formation of the tight junctions.[62] The barrier is less permeable to larger molecules, but is still permeable to water, carbon dioxide, oxygen, and most fat-soluble substances (including anaesthetics and alcohol).[43] The blood-brain barrier is not present in the circumventricular organs—which are structures in the brain that may need to respond to changes in body fluids—such as the pineal gland, area postrema, and some areas of the hypothalamus.[43] There is a similar blood–cerebrospinal fluid barrier, which serves the same purpose as the blood–brain barrier, but facilitates the transport of different substances into the brain due to the distinct structural characteristics between the two barrier systems.[43][63]
The larger arteries throughout the brain supply blood to smaller capillaries. These smallest of blood vessels in the brain, are lined with cells joined by tight junctions and so fluids do not seep in or leak out to the same degree as they do in other capillaries; this creates the blood–brain barrier.[43] Pericytes play a major role in the formation of the tight junctions.[62] The barrier is less permeable to larger molecules, but is still permeable to water, carbon dioxide, oxygen, and most fat-soluble substances (including anaesthetics and alcohol).[43] The blood-brain barrier is not present in the circumventricular organs—which are structures in the brain that may need to respond to changes in body fluids—such as the pineal gland, area postrema, and some areas of the hypothalamus.[43] There is a similar blood–cerebrospinal fluid barrier, which serves the same purpose as the blood–brain barrier, but facilitates the transport of different substances into the brain due to the distinct structural characteristics between the two barrier systems.[43][63]
Development
At the beginning of the third week of development, the embryonic ectoderm forms a thickened strip called the neural plate.[64] By the fourth week of development the neural plate has widened to give a broad cephalic end, a less broad middle part and a narrow caudal end. These swellings are known as the primary brain vesicles and represent the beginnings of the forebrain (prosencephalon), midbrain (mesencephalon), and hindbrain (rhombencephalon).[65]
Neural crest cells (derived from the ectoderm) populate the lateral edges of the plate at the neural folds. In the fourth week—during the neurulation stage—the neural folds close to form the neural tube, bringing together the neural crest cells at the neural crest.[66] The neural crest runs the length of the tube with cranial neural crest cells at the cephalic end and caudal neural crest cells at the tail. Cells detach from the crest and migrate in a craniocaudal (head to tail) wave inside the tube.[66] Cells at the cephalic end give rise to the brain, and cells at the caudal end give rise to the spinal cord.[67]
The tube flexes as it grows, forming the crescent-shaped cerebral hemispheres at the head. The cerebral hemispheres first appear on day 32.[68] Early in the fourth week, the cephalic part bends sharply forward in a cephalic flexure.[66] This flexed part becomes the forebrain (prosencephalon); the adjoining curving part becomes the midbrain (mesencephalon) and the part caudal to the flexure becomes the hindbrain (rhombencephalon). These areas are formed as swellings known as the three primary brain vesicles. In the fifth week of development five secondary brain vesicles have formed.[69] The forebrain separates into two vesicles – an anterior telencephalon and a posterior diencephalon. The telencephalon gives rise to the cerebral cortex, basal ganglia, and related structures. The diencephalon gives rise to the thalamus and hypothalamus. The hindbrain also splits into two areas – the metencephalon and the myelencephalon. The metencephalon gives rise to the cerebellum and pons. The myelencephalon gives rise to the medulla oblongata.[70] Also during the fifth week, the brain divides into repeating segments called neuromeres.[65][71] In the hindbrain these are known as rhombomeres.[72]
A characteristic of the brain is the cortical folding known as gyrification. For just over five months of prenatal development the cortex is smooth. By the gestational age of 24 weeks, the wrinkled morphology showing the fissures that begin to mark out the lobes of the brain is evident.[73] Why the cortex wrinkles and folds is not well-understood, but gyrification has been linked to intelligence and neurological disorders, and a number of gyrification theories have been proposed.[73] These theories include those based on mechanical buckling,[74][18] axonal tension,[75] and differential tangential expansion.[74] What is clear is that gyrification is not a random process, but rather a complex developmentally predetermined process which generates patterns of folds that are consistent between individuals and most species.[74][76]
The first groove to appear in the fourth month is the lateral cerebral fossa.[68] The expanding caudal end of the hemisphere has to curve over in a forward direction to fit into the restricted space. This covers the fossa and turns it into a much deeper ridge known as the lateral sulcus and this marks out the temporal lobe.[68] By the sixth month other sulci have formed that demarcate the frontal, parietal, and occipital lobes.[68] A gene present in the human genome (ARHGAP11B) may play a major role in gyrification and encephalisation.[77]
At the beginning of the third week of development, the embryonic ectoderm forms a thickened strip called the neural plate.[64] By the fourth week of development the neural plate has widened to give a broad cephalic end, a less broad middle part and a narrow caudal end. These swellings are known as the primary brain vesicles and represent the beginnings of the forebrain (prosencephalon), midbrain (mesencephalon), and hindbrain (rhombencephalon).[65]
Neural crest cells (derived from the ectoderm) populate the lateral edges of the plate at the neural folds. In the fourth week—during the neurulation stage—the neural folds close to form the neural tube, bringing together the neural crest cells at the neural crest.[66] The neural crest runs the length of the tube with cranial neural crest cells at the cephalic end and caudal neural crest cells at the tail. Cells detach from the crest and migrate in a craniocaudal (head to tail) wave inside the tube.[66] Cells at the cephalic end give rise to the brain, and cells at the caudal end give rise to the spinal cord.[67]
The tube flexes as it grows, forming the crescent-shaped cerebral hemispheres at the head. The cerebral hemispheres first appear on day 32.[68] Early in the fourth week, the cephalic part bends sharply forward in a cephalic flexure.[66] This flexed part becomes the forebrain (prosencephalon); the adjoining curving part becomes the midbrain (mesencephalon) and the part caudal to the flexure becomes the hindbrain (rhombencephalon). These areas are formed as swellings known as the three primary brain vesicles. In the fifth week of development five secondary brain vesicles have formed.[69] The forebrain separates into two vesicles – an anterior telencephalon and a posterior diencephalon. The telencephalon gives rise to the cerebral cortex, basal ganglia, and related structures. The diencephalon gives rise to the thalamus and hypothalamus. The hindbrain also splits into two areas – the metencephalon and the myelencephalon. The metencephalon gives rise to the cerebellum and pons. The myelencephalon gives rise to the medulla oblongata.[70] Also during the fifth week, the brain divides into repeating segments called neuromeres.[65][71] In the hindbrain these are known as rhombomeres.[72]
A characteristic of the brain is the cortical folding known as gyrification. For just over five months of prenatal development the cortex is smooth. By the gestational age of 24 weeks, the wrinkled morphology showing the fissures that begin to mark out the lobes of the brain is evident.[73] Why the cortex wrinkles and folds is not well-understood, but gyrification has been linked to intelligence and neurological disorders, and a number of gyrification theories have been proposed.[73] These theories include those based on mechanical buckling,[74][18] axonal tension,[75] and differential tangential expansion.[74] What is clear is that gyrification is not a random process, but rather a complex developmentally predetermined process which generates patterns of folds that are consistent between individuals and most species.[74][76]
The first groove to appear in the fourth month is the lateral cerebral fossa.[68] The expanding caudal end of the hemisphere has to curve over in a forward direction to fit into the restricted space. This covers the fossa and turns it into a much deeper ridge known as the lateral sulcus and this marks out the temporal lobe.[68] By the sixth month other sulci have formed that demarcate the frontal, parietal, and occipital lobes.[68] A gene present in the human genome (ARHGAP11B) may play a major role in gyrification and encephalisation.[77]
Function
The frontal lobe is involved in reasoning, motor control, emotion, and language. It contains the motor cortex, which is involved in planning and coordinating movement; the prefrontal cortex, which is responsible for higher-level cognitive functioning; and Broca’s area, which is essential for language production.[78] The motor system of the brain is responsible for the generation and control of movement.[79] Generated movements pass from the brain through nerves to motor neurons in the body, which control the action of muscles. The corticospinal tract carries movements from the brain, through the spinal cord, to the torso and limbs.[80] The cranial nerves carry movements related to the eyes, mouth and face.
Gross movement – such as locomotion and the movement of arms and legs – is generated in the motor cortex, divided into three parts: the primary motor cortex, found in the precentral gyrus and has sections dedicated to the movement of different body parts. These movements are supported and regulated by two other areas, lying anterior to the primary motor cortex: the premotor area and the supplementary motor area.[81] The hands and mouth have a much larger area dedicated to them than other body parts, allowing finer movement; this has been visualised in a motor homunculus.[81] Impulses generated from the motor cortex travel along the corticospinal tract along the front of the medulla and cross over (decussate) at the medullary pyramids. These then travel down the spinal cord, with most connecting to interneurons, in turn connecting to lower motor neurons within the grey matter that then transmit the impulse to move to muscles themselves.[80] The cerebellum and basal ganglia, play a role in fine, complex and coordinated muscle movements.[82] Connections between the cortex and the basal ganglia control muscle tone, posture and movement initiation, and are referred to as the extrapyramidal system.[83]
The frontal lobe is involved in reasoning, motor control, emotion, and language. It contains the motor cortex, which is involved in planning and coordinating movement; the prefrontal cortex, which is responsible for higher-level cognitive functioning; and Broca’s area, which is essential for language production.[78] The motor system of the brain is responsible for the generation and control of movement.[79] Generated movements pass from the brain through nerves to motor neurons in the body, which control the action of muscles. The corticospinal tract carries movements from the brain, through the spinal cord, to the torso and limbs.[80] The cranial nerves carry movements related to the eyes, mouth and face.
Gross movement – such as locomotion and the movement of arms and legs – is generated in the motor cortex, divided into three parts: the primary motor cortex, found in the precentral gyrus and has sections dedicated to the movement of different body parts. These movements are supported and regulated by two other areas, lying anterior to the primary motor cortex: the premotor area and the supplementary motor area.[81] The hands and mouth have a much larger area dedicated to them than other body parts, allowing finer movement; this has been visualised in a motor homunculus.[81] Impulses generated from the motor cortex travel along the corticospinal tract along the front of the medulla and cross over (decussate) at the medullary pyramids. These then travel down the spinal cord, with most connecting to interneurons, in turn connecting to lower motor neurons within the grey matter that then transmit the impulse to move to muscles themselves.[80] The cerebellum and basal ganglia, play a role in fine, complex and coordinated muscle movements.[82] Connections between the cortex and the basal ganglia control muscle tone, posture and movement initiation, and are referred to as the extrapyramidal system.[83]
Sensory
The sensory nervous system is involved with the reception and processing of sensory information. This information is received through the cranial nerves, through tracts in the spinal cord, and directly at centres of the brain exposed to the blood.[84] The brain also receives and interprets information from the special senses of vision, smell, hearing, and taste. Mixed motor and sensory signals are also integrated.[84]
From the skin, the brain receives information about fine touch, pressure, pain, vibration and temperature. From the joints, the brain receives information about joint position.[85] The sensory cortex is found just near the motor cortex, and, like the motor cortex, has areas related to sensation from different body parts. Sensation collected by a sensory receptor on the skin is changed to a nerve signal, that is passed up a series of neurons through tracts in the spinal cord. The dorsal column–medial lemniscus pathway contains information about fine touch, vibration and position of joints. The pathway fibres travel up the back part of the spinal cord to the back part of the medulla, where they connect with second-order neurons that immediately send fibres across the midline. These fibres then travel upwards into the ventrobasal complex in the thalamus where they connect with third-order neurons which send fibres up to the sensory cortex.[85] The spinothalamic tract carries information about pain, temperature, and gross touch. The pathway fibres travel up the spinal cord and connect with second-order neurons in the reticular formation of the brainstem for pain and temperature, and also terminate at the ventrobasal complex of the thalamus for gross touch.[86]
Vision is generated by light that hits the retina of the eye. Photoreceptors in the retina transduce the sensory stimulus of light into an electrical nerve signal that is sent to the visual cortex in the occipital lobe. Visual signals leave the retinas through the optic nerves. Optic nerve fibres from the retinas' nasal halves cross to the opposite sides joining the fibres from the temporal halves of the opposite retinas to form the optic tracts. The arrangements of the eyes' optics and the visual pathways mean vision from the left visual field is received by the right half of each retina, is processed by the right visual cortex, and vice versa. The optic tract fibres reach the brain at the lateral geniculate nucleus, and travel through the optic radiation to reach the visual cortex.[87]
Hearing and balance are both generated in the inner ear. Sound results in vibrations of the ossicles which continue finally to the hearing organ, and change in balance results in movement of liquids within the inner ear. This creates a nerve signal that passes through the vestibulocochlear nerve. From here, it passes through to the cochlear nuclei, the superior olivary nucleus, the medial geniculate nucleus, and finally the auditory radiation to the auditory cortex.[88]
The sense of smell is generated by receptor cells in the epithelium of the olfactory mucosa in the nasal cavity. This information passes via the olfactory nerve which goes into the skull through a relatively permeable part. This nerve transmits to the neural circuitry of the olfactory bulb from where information is passed to the olfactory cortex.[89][90] Taste is generated from receptors on the tongue and passed along the facial and glossopharyngeal nerves into the solitary nucleus in the brainstem. Some taste information is also passed from the pharynx into this area via the vagus nerve. Information is then passed from here through the thalamus into the gustatory cortex.[91]
The sensory nervous system is involved with the reception and processing of sensory information. This information is received through the cranial nerves, through tracts in the spinal cord, and directly at centres of the brain exposed to the blood.[84] The brain also receives and interprets information from the special senses of vision, smell, hearing, and taste. Mixed motor and sensory signals are also integrated.[84]
From the skin, the brain receives information about fine touch, pressure, pain, vibration and temperature. From the joints, the brain receives information about joint position.[85] The sensory cortex is found just near the motor cortex, and, like the motor cortex, has areas related to sensation from different body parts. Sensation collected by a sensory receptor on the skin is changed to a nerve signal, that is passed up a series of neurons through tracts in the spinal cord. The dorsal column–medial lemniscus pathway contains information about fine touch, vibration and position of joints. The pathway fibres travel up the back part of the spinal cord to the back part of the medulla, where they connect with second-order neurons that immediately send fibres across the midline. These fibres then travel upwards into the ventrobasal complex in the thalamus where they connect with third-order neurons which send fibres up to the sensory cortex.[85] The spinothalamic tract carries information about pain, temperature, and gross touch. The pathway fibres travel up the spinal cord and connect with second-order neurons in the reticular formation of the brainstem for pain and temperature, and also terminate at the ventrobasal complex of the thalamus for gross touch.[86]
Vision is generated by light that hits the retina of the eye. Photoreceptors in the retina transduce the sensory stimulus of light into an electrical nerve signal that is sent to the visual cortex in the occipital lobe. Visual signals leave the retinas through the optic nerves. Optic nerve fibres from the retinas' nasal halves cross to the opposite sides joining the fibres from the temporal halves of the opposite retinas to form the optic tracts. The arrangements of the eyes' optics and the visual pathways mean vision from the left visual field is received by the right half of each retina, is processed by the right visual cortex, and vice versa. The optic tract fibres reach the brain at the lateral geniculate nucleus, and travel through the optic radiation to reach the visual cortex.[87]
Hearing and balance are both generated in the inner ear. Sound results in vibrations of the ossicles which continue finally to the hearing organ, and change in balance results in movement of liquids within the inner ear. This creates a nerve signal that passes through the vestibulocochlear nerve. From here, it passes through to the cochlear nuclei, the superior olivary nucleus, the medial geniculate nucleus, and finally the auditory radiation to the auditory cortex.[88]
The sense of smell is generated by receptor cells in the epithelium of the olfactory mucosa in the nasal cavity. This information passes via the olfactory nerve which goes into the skull through a relatively permeable part. This nerve transmits to the neural circuitry of the olfactory bulb from where information is passed to the olfactory cortex.[89][90] Taste is generated from receptors on the tongue and passed along the facial and glossopharyngeal nerves into the solitary nucleus in the brainstem. Some taste information is also passed from the pharynx into this area via the vagus nerve. Information is then passed from here through the thalamus into the gustatory cortex.[91]
Regulation
Autonomic functions of the brain include the regulation, or rhythmic control of the heart rate and rate of breathing, and maintaining homeostasis.
Blood pressure and heart rate are influenced by the vasomotor centre of the medulla, which causes arteries and veins to be somewhat constricted at rest. It does this by influencing the sympathetic and parasympathetic nervous systems via the vagus nerve.[92] Information about blood pressure is generated by baroreceptors in aortic bodies in the aortic arch, and passed to the brain along the afferent fibres of the vagus nerve. Information about the pressure changes in the carotid sinus comes from carotid bodies located near the carotid artery and this is passed via a nerve joining with the glossopharyngeal nerve. This information travels up to the solitary nucleus in the medulla. Signals from here influence the vasomotor centre to adjust vein and artery constriction accordingly.[93]
The brain controls the rate of breathing, mainly by respiratory centres in the medulla and pons.[94] The respiratory centres control respiration, by generating motor signals that are passed down the spinal cord, along the phrenic nerve to the diaphragm and other muscles of respiration. This is a mixed nerve that carries sensory information back to the centres. There are four respiratory centres, three with a more clearly defined function, and an apneustic centre with a less clear function. In the medulla a dorsal respiratory group causes the desire to breathe in and receives sensory information directly from the body. Also in the medulla, the ventral respiratory group influences breathing out during exertion. In the pons the pneumotaxic centre influences the duration of each breath,[94] and the apneustic centre seems to have an influence on inhalation. The respiratory centres directly senses blood carbon dioxide and pH. Information about blood oxygen, carbon dioxide and pH levels are also sensed on the walls of arteries in the peripheral chemoreceptors of the aortic and carotid bodies. This information is passed via the vagus and glossopharyngeal nerves to the respiratory centres. High carbon dioxide, an acidic pH, or low oxygen stimulate the respiratory centres.[94] The desire to breathe in is also affected by pulmonary stretch receptors in the lungs which, when activated, prevent the lungs from overinflating by transmitting information to the respiratory centres via the vagus nerve.[94]
The hypothalamus in the diencephalon, is involved in regulating many functions of the body. Functions include neuroendocrine regulation, regulation of the circadian rhythm, control of the autonomic nervous system, and the regulation of fluid, and food intake. The circadian rhythm is controlled by two main cell groups in the hypothalamus. The anterior hypothalamus includes the suprachiasmatic nucleus and the ventrolateral preoptic nucleus which through gene expression cycles, generates a roughly 24 hour circadian clock. In the circadian day an ultradian rhythm takes control of the sleeping pattern. Sleep is an essential requirement for the body and brain and allows the closing down and resting of the body's systems. There are also findings that suggest that the daily build-up of toxins in the brain are removed during sleep.[95] Whilst awake the brain consumes a fifth of the body's total energy needs. Sleep necessarily reduces this use and gives time for the restoration of energy-giving ATP. The effects of sleep deprivation show the absolute need for sleep.[96]
The lateral hypothalamus contains orexinergic neurons that control appetite and arousal through their projections to the ascending reticular activating system.[97][98] The hypothalamus controls the pituitary gland through the release of peptides such as oxytocin, and vasopressin, as well as dopamine into the median eminence. Through the autonomic projections, the hypothalamus is involved in regulating functions such as blood pressure, heart rate, breathing, sweating, and other homeostatic mechanisms.[99] The hypothalamus also plays a role in thermal regulation, and when stimulated by the immune system, is capable of generating a fever. The hypothalamus is influenced by the kidneys: when blood pressure falls, the renin released by the kidneys stimulates a need to drink. The hypothalamus also regulates food intake through autonomic signals, and hormone release by the digestive system.[100]
Autonomic functions of the brain include the regulation, or rhythmic control of the heart rate and rate of breathing, and maintaining homeostasis.
Blood pressure and heart rate are influenced by the vasomotor centre of the medulla, which causes arteries and veins to be somewhat constricted at rest. It does this by influencing the sympathetic and parasympathetic nervous systems via the vagus nerve.[92] Information about blood pressure is generated by baroreceptors in aortic bodies in the aortic arch, and passed to the brain along the afferent fibres of the vagus nerve. Information about the pressure changes in the carotid sinus comes from carotid bodies located near the carotid artery and this is passed via a nerve joining with the glossopharyngeal nerve. This information travels up to the solitary nucleus in the medulla. Signals from here influence the vasomotor centre to adjust vein and artery constriction accordingly.[93]
The brain controls the rate of breathing, mainly by respiratory centres in the medulla and pons.[94] The respiratory centres control respiration, by generating motor signals that are passed down the spinal cord, along the phrenic nerve to the diaphragm and other muscles of respiration. This is a mixed nerve that carries sensory information back to the centres. There are four respiratory centres, three with a more clearly defined function, and an apneustic centre with a less clear function. In the medulla a dorsal respiratory group causes the desire to breathe in and receives sensory information directly from the body. Also in the medulla, the ventral respiratory group influences breathing out during exertion. In the pons the pneumotaxic centre influences the duration of each breath,[94] and the apneustic centre seems to have an influence on inhalation. The respiratory centres directly senses blood carbon dioxide and pH. Information about blood oxygen, carbon dioxide and pH levels are also sensed on the walls of arteries in the peripheral chemoreceptors of the aortic and carotid bodies. This information is passed via the vagus and glossopharyngeal nerves to the respiratory centres. High carbon dioxide, an acidic pH, or low oxygen stimulate the respiratory centres.[94] The desire to breathe in is also affected by pulmonary stretch receptors in the lungs which, when activated, prevent the lungs from overinflating by transmitting information to the respiratory centres via the vagus nerve.[94]
The hypothalamus in the diencephalon, is involved in regulating many functions of the body. Functions include neuroendocrine regulation, regulation of the circadian rhythm, control of the autonomic nervous system, and the regulation of fluid, and food intake. The circadian rhythm is controlled by two main cell groups in the hypothalamus. The anterior hypothalamus includes the suprachiasmatic nucleus and the ventrolateral preoptic nucleus which through gene expression cycles, generates a roughly 24 hour circadian clock. In the circadian day an ultradian rhythm takes control of the sleeping pattern. Sleep is an essential requirement for the body and brain and allows the closing down and resting of the body's systems. There are also findings that suggest that the daily build-up of toxins in the brain are removed during sleep.[95] Whilst awake the brain consumes a fifth of the body's total energy needs. Sleep necessarily reduces this use and gives time for the restoration of energy-giving ATP. The effects of sleep deprivation show the absolute need for sleep.[96]
The lateral hypothalamus contains orexinergic neurons that control appetite and arousal through their projections to the ascending reticular activating system.[97][98] The hypothalamus controls the pituitary gland through the release of peptides such as oxytocin, and vasopressin, as well as dopamine into the median eminence. Through the autonomic projections, the hypothalamus is involved in regulating functions such as blood pressure, heart rate, breathing, sweating, and other homeostatic mechanisms.[99] The hypothalamus also plays a role in thermal regulation, and when stimulated by the immune system, is capable of generating a fever. The hypothalamus is influenced by the kidneys: when blood pressure falls, the renin released by the kidneys stimulates a need to drink. The hypothalamus also regulates food intake through autonomic signals, and hormone release by the digestive system.[100]
Language
While language functions were traditionally thought to be localized to Wernicke's area and Broca's area,[101] it is now mostly accepted that a wider network of cortical regions contributes to language functions.[102][103][104]
The study on how language is represented, processed, and acquired by the brain is called neurolinguistics, which is a large multidisciplinary field drawing from cognitive neuroscience, cognitive linguistics, and psycholinguistics.[105]
While language functions were traditionally thought to be localized to Wernicke's area and Broca's area,[101] it is now mostly accepted that a wider network of cortical regions contributes to language functions.[102][103][104]
The study on how language is represented, processed, and acquired by the brain is called neurolinguistics, which is a large multidisciplinary field drawing from cognitive neuroscience, cognitive linguistics, and psycholinguistics.[105]
Lateralisation
The cerebrum has a contralateral organisation with each hemisphere of the brain interacting primarily with one half of the body: the left side of the brain interacts with the right side of the body, and vice versa. The developmental cause for this is uncertain.[106] Motor connections from the brain to the spinal cord, and sensory connections from the spinal cord to the brain, both cross sides in the brainstem. Visual input follows a more complex rule: the optic nerves from the two eyes come together at a point called the optic chiasm, and half of the fibres from each nerve split off to join the other.[107] The result is that connections from the left half of the retina, in both eyes, go to the left side of the brain, whereas connections from the right half of the retina go to the right side of the brain.[108] Because each half of the retina receives light coming from the opposite half of the visual field, the functional consequence is that visual input from the left side of the world goes to the right side of the brain, and vice versa.[106] Thus, the right side of the brain receives somatosensory input from the left side of the body, and visual input from the left side of the visual field.[109][110]
The left and right sides of the brain appear symmetrical, but they function asymmetrically.[111] For example, the counterpart of the left-hemisphere motor area controlling the right hand is the right-hemisphere area controlling the left hand. There are, however, several important exceptions, involving language and spatial cognition. The left frontal lobe is dominant for language. If a key language area in the left hemisphere is damaged, it can leave the victim unable to speak or understand,[111] whereas equivalent damage to the right hemisphere would cause only minor impairment to language skills.
A substantial part of current understanding of the interactions between the two hemispheres has come from the study of "split-brain patients"—people who underwent surgical transection of the corpus callosum in an attempt to reduce the severity of epileptic seizures.[112] These patients do not show unusual behaviour that is immediately obvious, but in some cases can behave almost like two different people in the same body, with the right hand taking an action and then the left hand undoing it.[112][113] These patients, when briefly shown a picture on the right side of the point of visual fixation, are able to describe it verbally, but when the picture is shown on the left, are unable to describe it, but may be able to give an indication with the left hand of the nature of the object shown.[113][114]
The cerebrum has a contralateral organisation with each hemisphere of the brain interacting primarily with one half of the body: the left side of the brain interacts with the right side of the body, and vice versa. The developmental cause for this is uncertain.[106] Motor connections from the brain to the spinal cord, and sensory connections from the spinal cord to the brain, both cross sides in the brainstem. Visual input follows a more complex rule: the optic nerves from the two eyes come together at a point called the optic chiasm, and half of the fibres from each nerve split off to join the other.[107] The result is that connections from the left half of the retina, in both eyes, go to the left side of the brain, whereas connections from the right half of the retina go to the right side of the brain.[108] Because each half of the retina receives light coming from the opposite half of the visual field, the functional consequence is that visual input from the left side of the world goes to the right side of the brain, and vice versa.[106] Thus, the right side of the brain receives somatosensory input from the left side of the body, and visual input from the left side of the visual field.[109][110]
The left and right sides of the brain appear symmetrical, but they function asymmetrically.[111] For example, the counterpart of the left-hemisphere motor area controlling the right hand is the right-hemisphere area controlling the left hand. There are, however, several important exceptions, involving language and spatial cognition. The left frontal lobe is dominant for language. If a key language area in the left hemisphere is damaged, it can leave the victim unable to speak or understand,[111] whereas equivalent damage to the right hemisphere would cause only minor impairment to language skills.
A substantial part of current understanding of the interactions between the two hemispheres has come from the study of "split-brain patients"—people who underwent surgical transection of the corpus callosum in an attempt to reduce the severity of epileptic seizures.[112] These patients do not show unusual behaviour that is immediately obvious, but in some cases can behave almost like two different people in the same body, with the right hand taking an action and then the left hand undoing it.[112][113] These patients, when briefly shown a picture on the right side of the point of visual fixation, are able to describe it verbally, but when the picture is shown on the left, are unable to describe it, but may be able to give an indication with the left hand of the nature of the object shown.[113][114]
Emotion
Emotions are generally defined as two-step multicomponent processes involving elicitation, followed by psychological feelings, appraisal, expression, autonomic responses, and action tendencies.[115] Attempts to localize basic emotions to certain brain regions have been controversial; some research found no evidence for specific locations corresponding to emotions, but instead found circuitry involved in general emotional processes. The amygdala, orbitofrontal cortex, mid and anterior insula cortex and lateral prefrontal cortex, appeared to be involved in generating the emotions, while weaker evidence was found for the ventral tegmental area, ventral pallidum and nucleus accumbens in incentive salience.[116] Others, however, have found evidence of activation of specific regions, such as the basal ganglia in happiness, the subcallosal cingulate cortex in sadness, and amygdala in fear.[117]
Emotions are generally defined as two-step multicomponent processes involving elicitation, followed by psychological feelings, appraisal, expression, autonomic responses, and action tendencies.[115] Attempts to localize basic emotions to certain brain regions have been controversial; some research found no evidence for specific locations corresponding to emotions, but instead found circuitry involved in general emotional processes. The amygdala, orbitofrontal cortex, mid and anterior insula cortex and lateral prefrontal cortex, appeared to be involved in generating the emotions, while weaker evidence was found for the ventral tegmental area, ventral pallidum and nucleus accumbens in incentive salience.[116] Others, however, have found evidence of activation of specific regions, such as the basal ganglia in happiness, the subcallosal cingulate cortex in sadness, and amygdala in fear.[117]
Cognition
The brain is responsible for cognition,[118][119] which functions through numerous processes and executive functions.[119][120][121] Executive functions include the ability to filter information and tune out irrelevant stimuli with attentional control and cognitive inhibition, the ability to process and manipulate information held in working memory, the ability to think about multiple concepts simultaneously and switch tasks with cognitive flexibility, the ability to inhibit impulses and prepotent responses with inhibitory control, and the ability to determine the relevance of information or appropriateness of an action.[120][121] Higher order executive functions require the simultaneous use of multiple basic executive functions, and include planning, prospection and fluid intelligence (i.e., reasoning and problem solving).[121]
The prefrontal cortex plays a significant role in mediating executive functions.[119][121][122] Planning involves activation of the dorsolateral prefrontal cortex (DLPFC), anterior cingulate cortex, angular prefrontal cortex, right prefrontal cortex, and supramarginal gyrus.[122] Working memory manipulation involves the DLPFC, inferior frontal gyrus, and areas of the parietal cortex.[119][122] Inhibitory control involves multiple areas of the prefrontal cortex, as well as the caudate nucleus and subthalamic nucleus.[121][122][123]
The brain is responsible for cognition,[118][119] which functions through numerous processes and executive functions.[119][120][121] Executive functions include the ability to filter information and tune out irrelevant stimuli with attentional control and cognitive inhibition, the ability to process and manipulate information held in working memory, the ability to think about multiple concepts simultaneously and switch tasks with cognitive flexibility, the ability to inhibit impulses and prepotent responses with inhibitory control, and the ability to determine the relevance of information or appropriateness of an action.[120][121] Higher order executive functions require the simultaneous use of multiple basic executive functions, and include planning, prospection and fluid intelligence (i.e., reasoning and problem solving).[121]
The prefrontal cortex plays a significant role in mediating executive functions.[119][121][122] Planning involves activation of the dorsolateral prefrontal cortex (DLPFC), anterior cingulate cortex, angular prefrontal cortex, right prefrontal cortex, and supramarginal gyrus.[122] Working memory manipulation involves the DLPFC, inferior frontal gyrus, and areas of the parietal cortex.[119][122] Inhibitory control involves multiple areas of the prefrontal cortex, as well as the caudate nucleus and subthalamic nucleus.[121][122][123]
Physiology
Neurotransmission
Brain activity is made possible by the interconnections of neurons that are linked together to reach their targets.[124] A neuron consists of a cell body, axon, and dendrites. Dendrites are often extensive branches that receive information in the form of signals from the axon terminals of other neurons. The signals received may cause the neuron to initiate an action potential (an electrochemical signal or nerve impulse) which is sent along its axon to the axon terminal, to connect with the dendrites or with the cell body of another neuron. An action potential is initiated at the initial segment of an axon, which contains a specialized complex of proteins.[125] When an action potential reaches the axon terminal it triggers the release of a neurotransmitter at a synapse that propagates a signal that acts on the target cell.[126] These chemical neurotransmitters include dopamine, serotonin, GABA, glutamate, and acetylcholine.[127] GABA is the major inhibitory neurotransmitter in the brain, and glutamate is the major excitatory neurotransmitter.[128] Neurons link at synapses to form neural pathways, neural circuits, and large elaborate network systems such as the salience network and the default mode network, and the activity between them is driven by the process of neurotransmission.
Brain activity is made possible by the interconnections of neurons that are linked together to reach their targets.[124] A neuron consists of a cell body, axon, and dendrites. Dendrites are often extensive branches that receive information in the form of signals from the axon terminals of other neurons. The signals received may cause the neuron to initiate an action potential (an electrochemical signal or nerve impulse) which is sent along its axon to the axon terminal, to connect with the dendrites or with the cell body of another neuron. An action potential is initiated at the initial segment of an axon, which contains a specialized complex of proteins.[125] When an action potential reaches the axon terminal it triggers the release of a neurotransmitter at a synapse that propagates a signal that acts on the target cell.[126] These chemical neurotransmitters include dopamine, serotonin, GABA, glutamate, and acetylcholine.[127] GABA is the major inhibitory neurotransmitter in the brain, and glutamate is the major excitatory neurotransmitter.[128] Neurons link at synapses to form neural pathways, neural circuits, and large elaborate network systems such as the salience network and the default mode network, and the activity between them is driven by the process of neurotransmission.
Metabolism
The brain consumes up to 20% of the energy used by the human body, more than any other organ.[129] In humans, blood glucose is the primary source of energy for most cells and is critical for normal function in a number of tissues, including the brain.[130] The human brain consumes approximately 60% of blood glucose in fasted, sedentary individuals.[130] Brain metabolism normally relies upon blood glucose as an energy source, but during times of low glucose (such as fasting, endurance exercise, or limited carbohydrate intake), the brain uses ketone bodies for fuel with a smaller need for glucose. The brain can also utilize lactate during exercise.[131] The brain stores glucose in the form of glycogen, albeit in significantly smaller amounts than that found in the liver or skeletal muscle.[132] Long-chain fatty acids cannot cross the blood–brain barrier, but the liver can break these down to produce ketone bodies. However, short-chain fatty acids (e.g., butyric acid, propionic acid, and acetic acid) and the medium-chain fatty acids, octanoic acid and heptanoic acid, can cross the blood–brain barrier and be metabolised by brain cells.[133][134][135]
Although the human brain represents only 2% of the body weight, it receives 15% of the cardiac output, 20% of total body oxygen consumption, and 25% of total body glucose utilization.[136] The brain mostly uses glucose for energy, and deprivation of glucose, as can happen in hypoglycemia, can result in loss of consciousness.[137] The energy consumption of the brain does not vary greatly over time, but active regions of the cortex consume somewhat more energy than inactive regions, which forms the basis for the functional neuroimaging methods of PET and fMRI.[138] These techniques provide a three-dimensional image of metabolic activity.[139] A preliminary study showed that brain metabolic requirements in humans peak at about five years old.[140]
The function of sleep is not fully understood; however, there is evidence that sleep enhances the clearance of metabolic waste products, some of which are potentially neurotoxic, from the brain and may also permit repair.[52][141][142] Evidence suggests that the increased clearance of metabolic waste during sleep occurs via increased functioning of the glymphatic system.[52] Sleep may also have an effect on cognitive function by weakening unnecessary connections.[143]
The brain consumes up to 20% of the energy used by the human body, more than any other organ.[129] In humans, blood glucose is the primary source of energy for most cells and is critical for normal function in a number of tissues, including the brain.[130] The human brain consumes approximately 60% of blood glucose in fasted, sedentary individuals.[130] Brain metabolism normally relies upon blood glucose as an energy source, but during times of low glucose (such as fasting, endurance exercise, or limited carbohydrate intake), the brain uses ketone bodies for fuel with a smaller need for glucose. The brain can also utilize lactate during exercise.[131] The brain stores glucose in the form of glycogen, albeit in significantly smaller amounts than that found in the liver or skeletal muscle.[132] Long-chain fatty acids cannot cross the blood–brain barrier, but the liver can break these down to produce ketone bodies. However, short-chain fatty acids (e.g., butyric acid, propionic acid, and acetic acid) and the medium-chain fatty acids, octanoic acid and heptanoic acid, can cross the blood–brain barrier and be metabolised by brain cells.[133][134][135]
Although the human brain represents only 2% of the body weight, it receives 15% of the cardiac output, 20% of total body oxygen consumption, and 25% of total body glucose utilization.[136] The brain mostly uses glucose for energy, and deprivation of glucose, as can happen in hypoglycemia, can result in loss of consciousness.[137] The energy consumption of the brain does not vary greatly over time, but active regions of the cortex consume somewhat more energy than inactive regions, which forms the basis for the functional neuroimaging methods of PET and fMRI.[138] These techniques provide a three-dimensional image of metabolic activity.[139] A preliminary study showed that brain metabolic requirements in humans peak at about five years old.[140]
The function of sleep is not fully understood; however, there is evidence that sleep enhances the clearance of metabolic waste products, some of which are potentially neurotoxic, from the brain and may also permit repair.[52][141][142] Evidence suggests that the increased clearance of metabolic waste during sleep occurs via increased functioning of the glymphatic system.[52] Sleep may also have an effect on cognitive function by weakening unnecessary connections.[143]
Research
The brain is not fully understood, and research is ongoing.[144] Neuroscientists, along with researchers from allied disciplines, study how the human brain works. The boundaries between the specialties of neuroscience, neurology and other disciplines such as psychiatry have faded as they are all influenced by basic research in neuroscience.
Neuroscience research has expanded considerably in recent decades. The "Decade of the Brain", an initiative of the United States Government in the 1990s, is considered to have marked much of this increase in research,[145] and was followed in 2013 by the BRAIN Initiative.[146] The Human Connectome Project was a five-year study launched in 2009 to analyse the anatomical and functional connections of parts of the brain, and has provided much data.[144]
The brain is not fully understood, and research is ongoing.[144] Neuroscientists, along with researchers from allied disciplines, study how the human brain works. The boundaries between the specialties of neuroscience, neurology and other disciplines such as psychiatry have faded as they are all influenced by basic research in neuroscience.
Neuroscience research has expanded considerably in recent decades. The "Decade of the Brain", an initiative of the United States Government in the 1990s, is considered to have marked much of this increase in research,[145] and was followed in 2013 by the BRAIN Initiative.[146] The Human Connectome Project was a five-year study launched in 2009 to analyse the anatomical and functional connections of parts of the brain, and has provided much data.[144]
Methods
Information about the structure and function of the human brain comes from a variety of experimental methods, including animals and humans. Information about brain trauma and stroke has provided information about the function of parts of the brain and the effects of brain damage. Neuroimaging is used to visualise the brain and record brain activity. Electrophysiology is used to measure, record and monitor the electrical activity of the cortex. Measurements may be of local field potentials of cortical areas, or of the activity of a single neuron. An electroencephalogram can record the electrical activity of the cortex using electrodes placed non-invasively on the scalp.[147][148]
Invasive measures include electrocorticography, which uses electrodes placed directly on the exposed surface of the brain. This method is used in cortical stimulation mapping, used in the study of the relationship between cortical areas and their systemic function.[149] By using much smaller microelectrodes, single-unit recordings can be made from a single neuron that give a high spatial resolution and high temporal resolution. This has enabled the linking of brain activity to behaviour, and the creation of neuronal maps.[150]
The development of cerebral organoids has opened ways for studying the growth of the brain, and of the cortex, and for understanding disease development, offering further implications for therapeutic applications.[151][152]
Information about the structure and function of the human brain comes from a variety of experimental methods, including animals and humans. Information about brain trauma and stroke has provided information about the function of parts of the brain and the effects of brain damage. Neuroimaging is used to visualise the brain and record brain activity. Electrophysiology is used to measure, record and monitor the electrical activity of the cortex. Measurements may be of local field potentials of cortical areas, or of the activity of a single neuron. An electroencephalogram can record the electrical activity of the cortex using electrodes placed non-invasively on the scalp.[147][148]
Invasive measures include electrocorticography, which uses electrodes placed directly on the exposed surface of the brain. This method is used in cortical stimulation mapping, used in the study of the relationship between cortical areas and their systemic function.[149] By using much smaller microelectrodes, single-unit recordings can be made from a single neuron that give a high spatial resolution and high temporal resolution. This has enabled the linking of brain activity to behaviour, and the creation of neuronal maps.[150]
The development of cerebral organoids has opened ways for studying the growth of the brain, and of the cortex, and for understanding disease development, offering further implications for therapeutic applications.[151][152]
Imaging
Functional neuroimaging techniques show changes in brain activity that relate to the function of specific brain areas. One technique is functional magnetic resonance imaging (fMRI) which has the advantages over earlier methods of SPECT and PET of not needing the use of radioactive materials and of offering a higher resolution.[153] Another technique is functional near-infrared spectroscopy. These methods rely on the haemodynamic response that shows changes in brain activity in relation to changes in blood flow, useful in mapping functions to brain areas.[154] Resting state fMRI looks at the interaction of brain regions whilst the brain is not performing a specific task.[155] This is also used to show the default mode network.
Any electrical current generates a magnetic field; neural oscillations induce weak magnetic fields, and in functional magnetoencephalography the current produced can show localised brain function in high resolution.[156] Tractography uses MRI and image analysis to create 3D images of the nerve tracts of the brain. Connectograms give a graphical representation of the neural connections of the brain.[157]
Differences in brain structure can be measured in some disorders, notably schizophrenia and dementia. Different biological approaches using imaging have given more insight for example into the disorders of depression and obsessive-compulsive disorder. A key source of information about the function of brain regions is the effects of damage to them.[158]
Advances in neuroimaging have enabled objective insights into mental disorders, leading to faster diagnosis, more accurate prognosis, and better monitoring.[159]
Functional neuroimaging techniques show changes in brain activity that relate to the function of specific brain areas. One technique is functional magnetic resonance imaging (fMRI) which has the advantages over earlier methods of SPECT and PET of not needing the use of radioactive materials and of offering a higher resolution.[153] Another technique is functional near-infrared spectroscopy. These methods rely on the haemodynamic response that shows changes in brain activity in relation to changes in blood flow, useful in mapping functions to brain areas.[154] Resting state fMRI looks at the interaction of brain regions whilst the brain is not performing a specific task.[155] This is also used to show the default mode network.
Any electrical current generates a magnetic field; neural oscillations induce weak magnetic fields, and in functional magnetoencephalography the current produced can show localised brain function in high resolution.[156] Tractography uses MRI and image analysis to create 3D images of the nerve tracts of the brain. Connectograms give a graphical representation of the neural connections of the brain.[157]
Differences in brain structure can be measured in some disorders, notably schizophrenia and dementia. Different biological approaches using imaging have given more insight for example into the disorders of depression and obsessive-compulsive disorder. A key source of information about the function of brain regions is the effects of damage to them.[158]
Advances in neuroimaging have enabled objective insights into mental disorders, leading to faster diagnosis, more accurate prognosis, and better monitoring.[159]
Gene and protein expression
Bioinformatics is a field of study that includes the creation and advancement of databases, and computational and statistical techniques, that can be used in studies of the human brain, particularly in the areas of gene and protein expression. Bioinformatics and studies in genomics, and functional genomics, generated the need for DNA annotation, a transcriptome technology, identifying genes, their locations and functions.[160][161][162] GeneCards is a major database.
As of 2017, just under 20,000 protein-coding genes are seen to be expressed in the human,[160] and some 400 of these genes are brain-specific.[163][164] The data that has been provided on gene expression in the brain has fuelled further research into a number of disorders. The long term use of alcohol for example, has shown altered gene expression in the brain, and cell-type specific changes that may relate to alcohol use disorder.[165] These changes have been noted in the synaptic transcriptome in the prefrontal cortex, and are seen as a factor causing the drive to alcohol dependence, and also to other substance abuses.[166]
Other related studies have also shown evidence of synaptic alterations and their loss, in the ageing brain. Changes in gene expression alter the levels of proteins in various neural pathways and this has been shown to be evident in synaptic contact dysfunction or loss. This dysfunction has been seen to affect many structures of the brain and has a marked effect on inhibitory neurons resulting in a decreased level of neurotransmission, and subsequent cognitive decline and disease.[167][168]
Bioinformatics is a field of study that includes the creation and advancement of databases, and computational and statistical techniques, that can be used in studies of the human brain, particularly in the areas of gene and protein expression. Bioinformatics and studies in genomics, and functional genomics, generated the need for DNA annotation, a transcriptome technology, identifying genes, their locations and functions.[160][161][162] GeneCards is a major database.
As of 2017, just under 20,000 protein-coding genes are seen to be expressed in the human,[160] and some 400 of these genes are brain-specific.[163][164] The data that has been provided on gene expression in the brain has fuelled further research into a number of disorders. The long term use of alcohol for example, has shown altered gene expression in the brain, and cell-type specific changes that may relate to alcohol use disorder.[165] These changes have been noted in the synaptic transcriptome in the prefrontal cortex, and are seen as a factor causing the drive to alcohol dependence, and also to other substance abuses.[166]
Other related studies have also shown evidence of synaptic alterations and their loss, in the ageing brain. Changes in gene expression alter the levels of proteins in various neural pathways and this has been shown to be evident in synaptic contact dysfunction or loss. This dysfunction has been seen to affect many structures of the brain and has a marked effect on inhibitory neurons resulting in a decreased level of neurotransmission, and subsequent cognitive decline and disease.[167][168]
Clinical significance
Injury
Injury to the brain can manifest in many ways. Traumatic brain injury, for example received in contact sport, after a fall, or a traffic or work accident, can be associated with both immediate and longer-term problems. Immediate problems may include bleeding within the brain, this may compress the brain tissue or damage its blood supply. Bruising to the brain may occur. Bruising may cause widespread damage to the nerve tracts that can lead to a condition of diffuse axonal injury.[169] A fractured skull, injury to a particular area, deafness, and concussion are also possible immediate developments. In addition to the site of injury, the opposite side of the brain may be affected, termed a contrecoup injury. Longer-term issues that may develop include posttraumatic stress disorder, and hydrocephalus. Chronic traumatic encephalopathy can develop following multiple head injuries.[170]
Injury to the brain can manifest in many ways. Traumatic brain injury, for example received in contact sport, after a fall, or a traffic or work accident, can be associated with both immediate and longer-term problems. Immediate problems may include bleeding within the brain, this may compress the brain tissue or damage its blood supply. Bruising to the brain may occur. Bruising may cause widespread damage to the nerve tracts that can lead to a condition of diffuse axonal injury.[169] A fractured skull, injury to a particular area, deafness, and concussion are also possible immediate developments. In addition to the site of injury, the opposite side of the brain may be affected, termed a contrecoup injury. Longer-term issues that may develop include posttraumatic stress disorder, and hydrocephalus. Chronic traumatic encephalopathy can develop following multiple head injuries.[170]
Disease
Neurodegenerative diseases result in progressive damage to different parts of the brain's function, and worsen with age. Common examples include dementia such as Alzheimer's disease, alcoholic dementia or vascular dementia; Parkinson's disease; and other rarer infectious, genetic, or metabolic causes such as Huntington's disease, motor neuron diseases, HIV dementia, syphilis-related dementia and Wilson's disease. Neurodegenerative diseases can affect different parts of the brain, and can affect movement, memory, and cognition.[171]
The brain, although protected by the blood–brain barrier, can be affected by infections including viruses, bacteria and fungi. Infection may be of the meninges (meningitis), the brain matter (encephalitis), or within the brain matter (such as a cerebral abscess).[172] Rare prion diseases including Creutzfeldt–Jakob disease and its variant, and kuru may also affect the brain.[172]
Neurodegenerative diseases result in progressive damage to different parts of the brain's function, and worsen with age. Common examples include dementia such as Alzheimer's disease, alcoholic dementia or vascular dementia; Parkinson's disease; and other rarer infectious, genetic, or metabolic causes such as Huntington's disease, motor neuron diseases, HIV dementia, syphilis-related dementia and Wilson's disease. Neurodegenerative diseases can affect different parts of the brain, and can affect movement, memory, and cognition.[171]
The brain, although protected by the blood–brain barrier, can be affected by infections including viruses, bacteria and fungi. Infection may be of the meninges (meningitis), the brain matter (encephalitis), or within the brain matter (such as a cerebral abscess).[172] Rare prion diseases including Creutzfeldt–Jakob disease and its variant, and kuru may also affect the brain.[172]
Tumours
Brain tumours can be either benign or cancerous. Most malignant tumours arise from another part of the body, most commonly from the lung, breast and skin.[173] Cancers of brain tissue can also occur, and originate from any tissue in and around the brain. Meningioma, cancer of the meninges around the brain, is more common than cancers of brain tissue.[173] Cancers within the brain may cause symptoms related to their size or position, with symptoms including headache and nausea, or the gradual development of focal symptoms such as gradual difficulty seeing, swallowing, talking, or as a change of mood.[173] Cancers are in general investigated through the use of CT scans and MRI scans. A variety of other tests including blood tests and lumbar puncture may be used to investigate for the cause of the cancer and evaluate the type and stage of the cancer.[173] The corticosteroid dexamethasone is often given to decrease the swelling of brain tissue around a tumour. Surgery may be considered, however given the complex nature of many tumours or based on tumour stage or type, radiotherapy or chemotherapy may be considered more suitable.[173]
Brain tumours can be either benign or cancerous. Most malignant tumours arise from another part of the body, most commonly from the lung, breast and skin.[173] Cancers of brain tissue can also occur, and originate from any tissue in and around the brain. Meningioma, cancer of the meninges around the brain, is more common than cancers of brain tissue.[173] Cancers within the brain may cause symptoms related to their size or position, with symptoms including headache and nausea, or the gradual development of focal symptoms such as gradual difficulty seeing, swallowing, talking, or as a change of mood.[173] Cancers are in general investigated through the use of CT scans and MRI scans. A variety of other tests including blood tests and lumbar puncture may be used to investigate for the cause of the cancer and evaluate the type and stage of the cancer.[173] The corticosteroid dexamethasone is often given to decrease the swelling of brain tissue around a tumour. Surgery may be considered, however given the complex nature of many tumours or based on tumour stage or type, radiotherapy or chemotherapy may be considered more suitable.[173]
Mental disorders
Mental disorders, such as depression, schizophrenia, bipolar disorder, posttraumatic stress disorder, attention deficit hyperactivity disorder, obsessive-compulsive disorder, Tourette syndrome, and addiction, are known to relate to the functioning of the brain.[123][127][174] Treatment for mental disorders may include psychotherapy, psychiatry, social intervention and personal recovery work or cognitive behavioural therapy; the underlying issues and associated prognoses vary significantly between individuals.[175]
Mental disorders, such as depression, schizophrenia, bipolar disorder, posttraumatic stress disorder, attention deficit hyperactivity disorder, obsessive-compulsive disorder, Tourette syndrome, and addiction, are known to relate to the functioning of the brain.[123][127][174] Treatment for mental disorders may include psychotherapy, psychiatry, social intervention and personal recovery work or cognitive behavioural therapy; the underlying issues and associated prognoses vary significantly between individuals.[175]
Epilepsy
Epileptic seizures are thought to relate to abnormal electrical activity.[176] Seizure activity can manifest as absence of consciousness, focal effects such as limb movement or impediments of speech, or be generalized in nature.[176] Status epilepticus refers to a seizure or series of seizures that have not terminated within 5 minutes.[177] Seizures have a large number of causes, however many seizures occur without a definitive cause being found. In a person with epilepsy, risk factors for further seizures may include sleeplessness, drug and alcohol intake, and stress. Seizures may be assessed using blood tests, EEG and various medical imaging techniques based on the medical history and medical examination findings.[176] In addition to treating an underlying cause and reducing exposure to risk factors, anticonvulsant medications can play a role in preventing further seizures.[176]
Epileptic seizures are thought to relate to abnormal electrical activity.[176] Seizure activity can manifest as absence of consciousness, focal effects such as limb movement or impediments of speech, or be generalized in nature.[176] Status epilepticus refers to a seizure or series of seizures that have not terminated within 5 minutes.[177] Seizures have a large number of causes, however many seizures occur without a definitive cause being found. In a person with epilepsy, risk factors for further seizures may include sleeplessness, drug and alcohol intake, and stress. Seizures may be assessed using blood tests, EEG and various medical imaging techniques based on the medical history and medical examination findings.[176] In addition to treating an underlying cause and reducing exposure to risk factors, anticonvulsant medications can play a role in preventing further seizures.[176]
Congenital
Some brain disorders such as Tay–Sachs disease[178] are congenital,[179] and linked to genetic and chromosomal mutations.[179] A rare group of congenital cephalic disorders known as lissencephaly is characterised by the lack of, or inadequacy of, cortical folding.[180] Normal development of the brain can be affected during pregnancy by nutritional deficiencies,[181] teratogens,[182] infectious diseases,[183] and by the use of recreational drugs, including alcohol (which may result in fetal alcohol spectrum disorders).[181][184]
Some brain disorders such as Tay–Sachs disease[178] are congenital,[179] and linked to genetic and chromosomal mutations.[179] A rare group of congenital cephalic disorders known as lissencephaly is characterised by the lack of, or inadequacy of, cortical folding.[180] Normal development of the brain can be affected during pregnancy by nutritional deficiencies,[181] teratogens,[182] infectious diseases,[183] and by the use of recreational drugs, including alcohol (which may result in fetal alcohol spectrum disorders).[181][184]
Stroke
A stroke is a decrease in blood supply to an area of the brain causing cell death and brain injury. This can lead to a wide range of symptoms, including the "FAST" symptoms of facial droop, arm weakness, and speech difficulties (including with speaking and finding words or forming sentences).[185] Symptoms relate to the function of the affected area of the brain and can point to the likely site and cause of the stroke. Difficulties with movement, speech, or sight usually relate to the cerebrum, whereas imbalance, double vision, vertigo and symptoms affecting more than one side of the body usually relate to the brainstem or cerebellum.[186]
Most strokes result from loss of blood supply, typically because of an embolus, rupture of a fatty plaque causing thrombus, or narrowing of small arteries. Strokes can also result from bleeding within the brain.[187] Transient ischaemic attacks (TIAs) are strokes in which symptoms resolve within 24 hours.[187] Investigation into the stroke will involve a medical examination (including a neurological examination) and the taking of a medical history, focusing on the duration of the symptoms and risk factors (including high blood pressure, atrial fibrillation, and smoking).[188] Further investigation is needed in younger patients.[189] An ECG and biotelemetry may be conducted to identify atrial fibrillation; an ultrasound can investigate narrowing of the carotid arteries; an echocardiogram can be used to look for clots within the heart, diseases of the heart valves or the presence of a patent foramen ovale.[189] Blood tests are routinely done as part of the workup including diabetes tests and a lipid profile.[189]
Some treatments for stroke are time-critical. These include clot dissolution or surgical removal of a clot for ischaemic strokes, and decompression for haemorrhagic strokes.[190][191] As stroke is time critical,[192] hospitals and even pre-hospital care of stroke involves expedited investigations – usually a CT scan to investigate for a haemorrhagic stroke and a CT or MR angiogram to evaluate arteries that supply the brain.[189] MRI scans, not as widely available, may be able to demonstrate the affected area of the brain more accurately, particularly with ischaemic stroke.[189]
Having experienced a stroke, a person may be admitted to a stroke unit, and treatments may be directed as preventing future strokes, including ongoing anticoagulation (such as aspirin or clopidogrel), antihypertensives, and lipid-lowering drugs.[190] A multidisciplinary team including speech pathologists, physiotherapists, occupational therapists, and psychologists plays a large role in supporting a person affected by a stroke and their rehabilitation.[193][189] A history of stroke increases the risk of developing dementia by around 70%, and recent stroke increases the risk by around 120%.[194]
A stroke is a decrease in blood supply to an area of the brain causing cell death and brain injury. This can lead to a wide range of symptoms, including the "FAST" symptoms of facial droop, arm weakness, and speech difficulties (including with speaking and finding words or forming sentences).[185] Symptoms relate to the function of the affected area of the brain and can point to the likely site and cause of the stroke. Difficulties with movement, speech, or sight usually relate to the cerebrum, whereas imbalance, double vision, vertigo and symptoms affecting more than one side of the body usually relate to the brainstem or cerebellum.[186]
Most strokes result from loss of blood supply, typically because of an embolus, rupture of a fatty plaque causing thrombus, or narrowing of small arteries. Strokes can also result from bleeding within the brain.[187] Transient ischaemic attacks (TIAs) are strokes in which symptoms resolve within 24 hours.[187] Investigation into the stroke will involve a medical examination (including a neurological examination) and the taking of a medical history, focusing on the duration of the symptoms and risk factors (including high blood pressure, atrial fibrillation, and smoking).[188] Further investigation is needed in younger patients.[189] An ECG and biotelemetry may be conducted to identify atrial fibrillation; an ultrasound can investigate narrowing of the carotid arteries; an echocardiogram can be used to look for clots within the heart, diseases of the heart valves or the presence of a patent foramen ovale.[189] Blood tests are routinely done as part of the workup including diabetes tests and a lipid profile.[189]
Some treatments for stroke are time-critical. These include clot dissolution or surgical removal of a clot for ischaemic strokes, and decompression for haemorrhagic strokes.[190][191] As stroke is time critical,[192] hospitals and even pre-hospital care of stroke involves expedited investigations – usually a CT scan to investigate for a haemorrhagic stroke and a CT or MR angiogram to evaluate arteries that supply the brain.[189] MRI scans, not as widely available, may be able to demonstrate the affected area of the brain more accurately, particularly with ischaemic stroke.[189]
Having experienced a stroke, a person may be admitted to a stroke unit, and treatments may be directed as preventing future strokes, including ongoing anticoagulation (such as aspirin or clopidogrel), antihypertensives, and lipid-lowering drugs.[190] A multidisciplinary team including speech pathologists, physiotherapists, occupational therapists, and psychologists plays a large role in supporting a person affected by a stroke and their rehabilitation.[193][189] A history of stroke increases the risk of developing dementia by around 70%, and recent stroke increases the risk by around 120%.[194]
Brain death
Brain death refers to an irreversible total loss of brain function.[195][196] This is characterised by coma, loss of reflexes, and apnoea,[195] however, the declaration of brain death varies geographically and is not always accepted.[196] In some countries there is also a defined syndrome of brainstem death.[197] Declaration of brain death can have profound implications as the declaration, under the principle of medical futility, will be associated with the withdrawal of life support,[198] and as those with brain death often have organs suitable for organ donation.[196][199] The process is often made more difficult by poor communication with patients' families.[200]
When brain death is suspected, reversible differential diagnoses such as, electrolyte, neurological and drug-related cognitive suppression need to be excluded.[195][198] Testing for reflexes[b] can be of help in the decision, as can the absence of response and breathing.[198] Clinical observations, including a total lack of responsiveness, a known diagnosis, and neural imaging evidence, may all play a role in the decision to pronounce brain death.[195]
Brain death refers to an irreversible total loss of brain function.[195][196] This is characterised by coma, loss of reflexes, and apnoea,[195] however, the declaration of brain death varies geographically and is not always accepted.[196] In some countries there is also a defined syndrome of brainstem death.[197] Declaration of brain death can have profound implications as the declaration, under the principle of medical futility, will be associated with the withdrawal of life support,[198] and as those with brain death often have organs suitable for organ donation.[196][199] The process is often made more difficult by poor communication with patients' families.[200]
When brain death is suspected, reversible differential diagnoses such as, electrolyte, neurological and drug-related cognitive suppression need to be excluded.[195][198] Testing for reflexes[b] can be of help in the decision, as can the absence of response and breathing.[198] Clinical observations, including a total lack of responsiveness, a known diagnosis, and neural imaging evidence, may all play a role in the decision to pronounce brain death.[195]
Society and culture
Neuroanthropology is the study of the relationship between culture and the brain. It explores how the brain gives rise to culture, and how culture influences brain development.[201] Cultural differences and their relation to brain development and structure are researched in different fields.[202]
Neuroanthropology is the study of the relationship between culture and the brain. It explores how the brain gives rise to culture, and how culture influences brain development.[201] Cultural differences and their relation to brain development and structure are researched in different fields.[202]
The mind
The philosophy of the mind studies such issues as the problem of understanding consciousness and the mind–body problem. The relationship between the brain and the mind is a significant challenge both philosophically and scientifically. This is because of the difficulty in explaining how mental activities, such as thoughts and emotions, can be implemented by physical structures such as neurons and synapses, or by any other type of physical mechanism. This difficulty was expressed by Gottfried Leibniz in the analogy known as Leibniz's Mill:
Doubt about the possibility of a mechanistic explanation of thought drove René Descartes, and most other philosophers along with him, to dualism: the belief that the mind is to some degree independent of the brain.[205] There has always, however, been a strong argument in the opposite direction. There is clear empirical evidence that physical manipulations of, or injuries to, the brain (for example by drugs or by lesions, respectively) can affect the mind in potent and intimate ways.[206][207] In the 19th century, the case of Phineas Gage, a railway worker who was injured by a stout iron rod passing through his brain, convinced both researchers and the public that cognitive functions were localised in the brain.[203] Following this line of thinking, a large body of empirical evidence for a close relationship between brain activity and mental activity has led most neuroscientists and contemporary philosophers to be materialists, believing that mental phenomena are ultimately the result of, or reducible to, physical phenomena.[208]
The philosophy of the mind studies such issues as the problem of understanding consciousness and the mind–body problem. The relationship between the brain and the mind is a significant challenge both philosophically and scientifically. This is because of the difficulty in explaining how mental activities, such as thoughts and emotions, can be implemented by physical structures such as neurons and synapses, or by any other type of physical mechanism. This difficulty was expressed by Gottfried Leibniz in the analogy known as Leibniz's Mill:
Doubt about the possibility of a mechanistic explanation of thought drove René Descartes, and most other philosophers along with him, to dualism: the belief that the mind is to some degree independent of the brain.[205] There has always, however, been a strong argument in the opposite direction. There is clear empirical evidence that physical manipulations of, or injuries to, the brain (for example by drugs or by lesions, respectively) can affect the mind in potent and intimate ways.[206][207] In the 19th century, the case of Phineas Gage, a railway worker who was injured by a stout iron rod passing through his brain, convinced both researchers and the public that cognitive functions were localised in the brain.[203] Following this line of thinking, a large body of empirical evidence for a close relationship between brain activity and mental activity has led most neuroscientists and contemporary philosophers to be materialists, believing that mental phenomena are ultimately the result of, or reducible to, physical phenomena.[208]
Brain size
The size of the brain and a person's intelligence are not strongly related.[209] Studies tend to indicate small to moderate correlations (averaging around 0.3 to 0.4) between brain volume and IQ.[210] The most consistent associations are observed within the frontal, temporal, and parietal lobes, the hippocampi, and the cerebellum, but these only account for a relatively small amount of variance in IQ, which itself has only a partial relationship to general intelligence and real-world performance.[211][212]
Other animals, including whales and elephants have larger brains than humans. However, when the brain-to-body mass ratio is taken into account, the human brain is almost twice as large as that of a bottlenose dolphin, and three times as large as that of a chimpanzee. However, a high ratio does not of itself demonstrate intelligence: very small animals have high ratios and the treeshrew has the largest quotient of any mammal.[213]
The size of the brain and a person's intelligence are not strongly related.[209] Studies tend to indicate small to moderate correlations (averaging around 0.3 to 0.4) between brain volume and IQ.[210] The most consistent associations are observed within the frontal, temporal, and parietal lobes, the hippocampi, and the cerebellum, but these only account for a relatively small amount of variance in IQ, which itself has only a partial relationship to general intelligence and real-world performance.[211][212]
Other animals, including whales and elephants have larger brains than humans. However, when the brain-to-body mass ratio is taken into account, the human brain is almost twice as large as that of a bottlenose dolphin, and three times as large as that of a chimpanzee. However, a high ratio does not of itself demonstrate intelligence: very small animals have high ratios and the treeshrew has the largest quotient of any mammal.[213]
In popular culture
Earlier ideas about the relative importance of the different organs of the human body sometimes emphasized the heart.[214] Modern Western popular conceptions, in contrast, have placed increasing focus on the brain.[215]
Research has disproved some common misconceptions about the brain. These include both ancient and modern myths. It is not true (for example) that neurons are not replaced after the age of two; nor that normal humans use only ten per cent of the brain.[216] Popular culture has also oversimplified the lateralisation of the brain by suggesting that functions are completely specific to one side of the brain or the other. Akio Mori coined the term "game brain" for the unreliably supported theory that spending long periods playing video games harmed the brain's pre-frontal region, and impaired the expression of emotion and creativity.[217]
Historically, particularly in the early-19th century, the brain featured in popular culture through phrenology, a pseudoscience that assigned personality attributes to different regions of the cortex. The cortex remains important in popular culture as covered in books and satire.[218][219]
The human brain can feature in science fiction, with themes such as brain transplants and cyborgs (beings with features like partly artificial brains).[220] The 1942 science-fiction book (adapted three times for the cinema) Donovan's Brain tells the tale of an isolated brain kept alive in vitro, gradually taking over the personality of the book's protagonist.[221]
Earlier ideas about the relative importance of the different organs of the human body sometimes emphasized the heart.[214] Modern Western popular conceptions, in contrast, have placed increasing focus on the brain.[215]
Research has disproved some common misconceptions about the brain. These include both ancient and modern myths. It is not true (for example) that neurons are not replaced after the age of two; nor that normal humans use only ten per cent of the brain.[216] Popular culture has also oversimplified the lateralisation of the brain by suggesting that functions are completely specific to one side of the brain or the other. Akio Mori coined the term "game brain" for the unreliably supported theory that spending long periods playing video games harmed the brain's pre-frontal region, and impaired the expression of emotion and creativity.[217]
Historically, particularly in the early-19th century, the brain featured in popular culture through phrenology, a pseudoscience that assigned personality attributes to different regions of the cortex. The cortex remains important in popular culture as covered in books and satire.[218][219]
The human brain can feature in science fiction, with themes such as brain transplants and cyborgs (beings with features like partly artificial brains).[220] The 1942 science-fiction book (adapted three times for the cinema) Donovan's Brain tells the tale of an isolated brain kept alive in vitro, gradually taking over the personality of the book's protagonist.[221]
History
Early history
The Edwin Smith Papyrus, an ancient Egyptian medical treatise written in the 17th century BC, contains the earliest recorded reference to the brain. The hieroglyph for brain, occurring eight times in this papyrus, describes the symptoms, diagnosis, and prognosis of two traumatic injuries to the head. The papyrus mentions the external surface of the brain, the effects of injury (including seizures and aphasia), the meninges, and cerebrospinal fluid.[222][223]
In the fifth century BC, Alcmaeon of Croton in Magna Grecia, first considered the brain to be the seat of the mind.[223] Also in the fifth century BC in Athens, the unknown author of On the Sacred Disease, a medical treatise which is part of the Hippocratic Corpus and traditionally attributed to Hippocrates, believed the brain to be the seat of intelligence. Aristotle, in his biology initially believed the heart to be the seat of intelligence, and saw the brain as a cooling mechanism for the blood. He reasoned that humans are more rational than the beasts because, among other reasons, they have a larger brain to cool their hot-bloodedness.[224] Aristotle did describe the meninges and distinguished between the cerebrum and cerebellum.[225]
Herophilus of Chalcedon in the fourth and third centuries BC distinguished the cerebrum and the cerebellum, and provided the first clear description of the ventricles; and with Erasistratus of Ceos experimented on living brains. Their works are now mostly lost, and we know about their achievements due mostly to secondary sources. Some of their discoveries had to be re-discovered a millennium after their deaths.[223] Anatomist physician Galen in the second century AD, during the time of the Roman Empire, dissected the brains of sheep, monkeys, dogs, and pigs. He concluded that, as the cerebellum was denser than the brain, it must control the muscles, while as the cerebrum was soft, it must be where the senses were processed. Galen further theorized that the brain functioned by movement of animal spirits through the ventricles.[223][224]
The Edwin Smith Papyrus, an ancient Egyptian medical treatise written in the 17th century BC, contains the earliest recorded reference to the brain. The hieroglyph for brain, occurring eight times in this papyrus, describes the symptoms, diagnosis, and prognosis of two traumatic injuries to the head. The papyrus mentions the external surface of the brain, the effects of injury (including seizures and aphasia), the meninges, and cerebrospinal fluid.[222][223]
In the fifth century BC, Alcmaeon of Croton in Magna Grecia, first considered the brain to be the seat of the mind.[223] Also in the fifth century BC in Athens, the unknown author of On the Sacred Disease, a medical treatise which is part of the Hippocratic Corpus and traditionally attributed to Hippocrates, believed the brain to be the seat of intelligence. Aristotle, in his biology initially believed the heart to be the seat of intelligence, and saw the brain as a cooling mechanism for the blood. He reasoned that humans are more rational than the beasts because, among other reasons, they have a larger brain to cool their hot-bloodedness.[224] Aristotle did describe the meninges and distinguished between the cerebrum and cerebellum.[225]
Herophilus of Chalcedon in the fourth and third centuries BC distinguished the cerebrum and the cerebellum, and provided the first clear description of the ventricles; and with Erasistratus of Ceos experimented on living brains. Their works are now mostly lost, and we know about their achievements due mostly to secondary sources. Some of their discoveries had to be re-discovered a millennium after their deaths.[223] Anatomist physician Galen in the second century AD, during the time of the Roman Empire, dissected the brains of sheep, monkeys, dogs, and pigs. He concluded that, as the cerebellum was denser than the brain, it must control the muscles, while as the cerebrum was soft, it must be where the senses were processed. Galen further theorized that the brain functioned by movement of animal spirits through the ventricles.[223][224]
Renaissance
In 1316, Mondino de Luzzi's Anathomia began the modern study of brain anatomy.[226] Niccolò Massa discovered in 1536 that the ventricles were filled with fluid.[227] Archangelo Piccolomini of Rome was the first to distinguish between the cerebrum and cerebral cortex.[228] In 1543 Andreas Vesalius published his seven-volume De humani corporis fabrica.[228][229][230] The seventh book covered the brain and eye, with detailed images of the ventricles, cranial nerves, pituitary gland, meninges, structures of the eye, the vascular supply to the brain and spinal cord, and an image of the peripheral nerves.[231] Vesalius rejected the common belief that the ventricles were responsible for brain function, arguing that many animals have a similar ventricular system to humans, but no true intelligence.[228]
René Descartes proposed the theory of dualism to tackle the issue of the brain's relation to the mind. He suggested that the pineal gland was where the mind interacted with the body, serving as the seat of the soul and as the connection through which animal spirits passed from the blood into the brain.[227] This dualism likely provided impetus for later anatomists to further explore the relationship between the anatomical and functional aspects of brain anatomy.[232]
Thomas Willis is considered a second pioneer in the study of neurology and brain science. He wrote Cerebri Anatome (Latin: Anatomy of the brain)[c] in 1664, followed by Cerebral Pathology in 1667. In these he described the structure of the cerebellum, the ventricles, the cerebral hemispheres, the brainstem, and the cranial nerves, studied its blood supply; and proposed functions associated with different areas of the brain.[228] The circle of Willis was named after his investigations into the blood supply of the brain, and he was the first to use the word "neurology."[233] Willis removed the brain from the body when examining it, and rejected the commonly held view that the cortex only consisted of blood vessels, and the view of the last two millennia that the cortex was only incidentally important.[228]
In the middle of 19th century Emil du Bois-Reymond and Hermann von Helmholtz were able to use a galvanometer to show that electrical impulses passed at measurable speeds along nerves, refuting the view of their teacher Johannes Peter Müller that the nerve impulse was a vital function that could not be measured.[234][235][236] Richard Caton in 1875 demonstrated electrical impulses in the cerebral hemispheres of rabbits and monkeys.[237] In the 1820s, Jean Pierre Flourens pioneered the experimental method of damaging specific parts of animal brains describing the effects on movement and behavior.[238]
In 1316, Mondino de Luzzi's Anathomia began the modern study of brain anatomy.[226] Niccolò Massa discovered in 1536 that the ventricles were filled with fluid.[227] Archangelo Piccolomini of Rome was the first to distinguish between the cerebrum and cerebral cortex.[228] In 1543 Andreas Vesalius published his seven-volume De humani corporis fabrica.[228][229][230] The seventh book covered the brain and eye, with detailed images of the ventricles, cranial nerves, pituitary gland, meninges, structures of the eye, the vascular supply to the brain and spinal cord, and an image of the peripheral nerves.[231] Vesalius rejected the common belief that the ventricles were responsible for brain function, arguing that many animals have a similar ventricular system to humans, but no true intelligence.[228]
René Descartes proposed the theory of dualism to tackle the issue of the brain's relation to the mind. He suggested that the pineal gland was where the mind interacted with the body, serving as the seat of the soul and as the connection through which animal spirits passed from the blood into the brain.[227] This dualism likely provided impetus for later anatomists to further explore the relationship between the anatomical and functional aspects of brain anatomy.[232]
Thomas Willis is considered a second pioneer in the study of neurology and brain science. He wrote Cerebri Anatome (Latin: Anatomy of the brain)[c] in 1664, followed by Cerebral Pathology in 1667. In these he described the structure of the cerebellum, the ventricles, the cerebral hemispheres, the brainstem, and the cranial nerves, studied its blood supply; and proposed functions associated with different areas of the brain.[228] The circle of Willis was named after his investigations into the blood supply of the brain, and he was the first to use the word "neurology."[233] Willis removed the brain from the body when examining it, and rejected the commonly held view that the cortex only consisted of blood vessels, and the view of the last two millennia that the cortex was only incidentally important.[228]
In the middle of 19th century Emil du Bois-Reymond and Hermann von Helmholtz were able to use a galvanometer to show that electrical impulses passed at measurable speeds along nerves, refuting the view of their teacher Johannes Peter Müller that the nerve impulse was a vital function that could not be measured.[234][235][236] Richard Caton in 1875 demonstrated electrical impulses in the cerebral hemispheres of rabbits and monkeys.[237] In the 1820s, Jean Pierre Flourens pioneered the experimental method of damaging specific parts of animal brains describing the effects on movement and behavior.[238]
Modern period
Studies of the brain became more sophisticated with the use of the microscope and the development of a silver staining method by Camillo Golgi during the 1880s. This was able to show the intricate structures of single neurons.[239] This was used by Santiago Ramón y Cajal and led to the formation of the neuron doctrine, the then revolutionary hypothesis that the neuron is the functional unit of the brain. He used microscopy to uncover many cell types, and proposed functions for the cells he saw.[239] For this, Golgi and Cajal are considered the founders of twentieth century neuroscience, both sharing the Nobel prize in 1906 for their studies and discoveries in this field.[239]
Charles Sherrington published his influential 1906 work The Integrative Action of the Nervous System examining the function of reflexes, evolutionary development of the nervous system, functional specialisation of the brain, and layout and cellular function of the central nervous system.[240] In 1942 he coined the term enchanted loom as a metaphor for the brain. John Farquhar Fulton, founded the Journal of Neurophysiology and published the first comprehensive textbook on the physiology of the nervous system during 1938.[241] Neuroscience during the twentieth century began to be recognised as a distinct unified academic discipline, with David Rioch, Francis O. Schmitt, and Stephen Kuffler playing critical roles in establishing the field.[242] Rioch originated the integration of basic anatomical and physiological research with clinical psychiatry at the Walter Reed Army Institute of Research, starting in the 1950s.[243] During the same period, Schmitt established the Neuroscience Research Program, an inter-university and international organisation, bringing together biology, medicine, psychological and behavioural sciences. The word neuroscience itself arises from this program.[244]
Paul Broca associated regions of the brain with specific functions, in particular language in Broca's area, following work on brain-damaged patients.[245] John Hughlings Jackson described the function of the motor cortex by watching the progression of epileptic seizures through the body. Carl Wernicke described a region associated with language comprehension and production. Korbinian Brodmann divided regions of the brain based on the appearance of cells.[245] By 1950, Sherrington, Papez, and MacLean had identified many of the brainstem and limbic system functions.[246][247] The capacity of the brain to re-organise and change with age, and a recognised critical development period, were attributed to neuroplasticity, pioneered by Margaret Kennard, who experimented on monkeys during the 1930-40s.[248]
Harvey Cushing (1869–1939) is recognised as the first proficient brain surgeon in the world.[249] In 1937, Walter Dandy began the practice of vascular neurosurgery by performing the first surgical clipping of an intracranial aneurysm.[250]
Studies of the brain became more sophisticated with the use of the microscope and the development of a silver staining method by Camillo Golgi during the 1880s. This was able to show the intricate structures of single neurons.[239] This was used by Santiago Ramón y Cajal and led to the formation of the neuron doctrine, the then revolutionary hypothesis that the neuron is the functional unit of the brain. He used microscopy to uncover many cell types, and proposed functions for the cells he saw.[239] For this, Golgi and Cajal are considered the founders of twentieth century neuroscience, both sharing the Nobel prize in 1906 for their studies and discoveries in this field.[239]
Charles Sherrington published his influential 1906 work The Integrative Action of the Nervous System examining the function of reflexes, evolutionary development of the nervous system, functional specialisation of the brain, and layout and cellular function of the central nervous system.[240] In 1942 he coined the term enchanted loom as a metaphor for the brain. John Farquhar Fulton, founded the Journal of Neurophysiology and published the first comprehensive textbook on the physiology of the nervous system during 1938.[241] Neuroscience during the twentieth century began to be recognised as a distinct unified academic discipline, with David Rioch, Francis O. Schmitt, and Stephen Kuffler playing critical roles in establishing the field.[242] Rioch originated the integration of basic anatomical and physiological research with clinical psychiatry at the Walter Reed Army Institute of Research, starting in the 1950s.[243] During the same period, Schmitt established the Neuroscience Research Program, an inter-university and international organisation, bringing together biology, medicine, psychological and behavioural sciences. The word neuroscience itself arises from this program.[244]
Paul Broca associated regions of the brain with specific functions, in particular language in Broca's area, following work on brain-damaged patients.[245] John Hughlings Jackson described the function of the motor cortex by watching the progression of epileptic seizures through the body. Carl Wernicke described a region associated with language comprehension and production. Korbinian Brodmann divided regions of the brain based on the appearance of cells.[245] By 1950, Sherrington, Papez, and MacLean had identified many of the brainstem and limbic system functions.[246][247] The capacity of the brain to re-organise and change with age, and a recognised critical development period, were attributed to neuroplasticity, pioneered by Margaret Kennard, who experimented on monkeys during the 1930-40s.[248]
Harvey Cushing (1869–1939) is recognised as the first proficient brain surgeon in the world.[249] In 1937, Walter Dandy began the practice of vascular neurosurgery by performing the first surgical clipping of an intracranial aneurysm.[250]
Comparative anatomy
The human brain has many properties that are common to all vertebrate brains.[251] Many of its features are common to all mammalian brains,[252] most notably a six-layered cerebral cortex and a set of associated structures,[253] including the hippocampus and amygdala.[254] The cortex is proportionally larger in humans than in many other mammals.[255] Humans have more association cortex, sensory and motor parts than smaller mammals such as the rat and the cat.[256]
As a primate brain, the human brain has a much larger cerebral cortex, in proportion to body size, than most mammals,[254] and a highly developed visual system.[257][258]
As a hominid brain, the human brain is substantially enlarged even in comparison to the brain of a typical monkey. The sequence of human evolution from Australopithecus (four million years ago) to Homo sapiens (modern humans) was marked by a steady increase in brain size.[259][260] As brain size increased, this altered the size and shape of the skull,[261] from about 600 cm3 in Homo habilis to an average of about 1520 cm3 in Homo neanderthalensis.[262] Differences in DNA, gene expression, and gene–environment interactions help explain the differences between the function of the human brain and other primates.[263]
The human brain has many properties that are common to all vertebrate brains.[251] Many of its features are common to all mammalian brains,[252] most notably a six-layered cerebral cortex and a set of associated structures,[253] including the hippocampus and amygdala.[254] The cortex is proportionally larger in humans than in many other mammals.[255] Humans have more association cortex, sensory and motor parts than smaller mammals such as the rat and the cat.[256]
As a primate brain, the human brain has a much larger cerebral cortex, in proportion to body size, than most mammals,[254] and a highly developed visual system.[257][258]
As a hominid brain, the human brain is substantially enlarged even in comparison to the brain of a typical monkey. The sequence of human evolution from Australopithecus (four million years ago) to Homo sapiens (modern humans) was marked by a steady increase in brain size.[259][260] As brain size increased, this altered the size and shape of the skull,[261] from about 600 cm3 in Homo habilis to an average of about 1520 cm3 in Homo neanderthalensis.[262] Differences in DNA, gene expression, and gene–environment interactions help explain the differences between the function of the human brain and other primates.[263]
See also
References
- "Encephalo- Etymology". Online Etymology Dictionary. Archived from the original on October 2, 2017. Retrieved October 24, 2015.
- Fan, Xue; Markram, Henry (May 7, 2019). "A Brief History of Simulation Neuroscience". Frontiers in Neuroinformatics. 13: 32. doi:10.3389/fninf.2019.00032. ISSN 1662-5196. PMC 6513977. PMID 31133838.
- Parent, A.; Carpenter, M.B. (1995). "Ch. 1". Carpenter's Human Neuroanatomy. Williams & Wilkins. ISBN 978-0-683-06752-1.
- Bigos, K.L.; Hariri, A.; Weinberger, D. (2015). Neuroimaging Genetics: Principles and Practices. Oxford University Press. p. 157. ISBN 978-0-19-992022-8.
- Cosgrove, K.P.; Mazure, C.M.; Staley, J.K. (2007). "Evolving knowledge of sex differences in brain structure, function, and chemistry". Biol Psychiatry. 62 (8): 847–855. doi:10.1016/j.biopsych.2007.03.001. PMC 2711771. PMID 17544382.
- Molina, D. Kimberley; DiMaio, Vincent J.M. (2012). "Normal Organ Weights in Men". The American Journal of Forensic Medicine and Pathology. 33 (4): 368–372. doi:10.1097/PAF.0b013e31823d29ad. ISSN 0195-7910. PMID 22182984. S2CID 32174574.
- Molina, D. Kimberley; DiMaio, Vincent J. M. (2015). "Normal Organ Weights in Women". The American Journal of Forensic Medicine and Pathology. 36 (3): 182–187. doi:10.1097/PAF.0000000000000175. ISSN 0195-7910. PMID 26108038. S2CID 25319215.
- Gray's Anatomy 2008, pp. 227–9.
- Gray's Anatomy 2008, pp. 335–7.
- Ribas, G. C. (2010). "The cerebral sulci and gyri". Neurosurgical Focus. 28 (2): 7. doi:10.3171/2009.11.FOCUS09245. PMID 20121437.
- Frigeri, T.; Paglioli, E.; De Oliveira, E.; Rhoton Jr, A. L. (2015). "Microsurgical anatomy of the central lobe". Journal of Neurosurgery. 122 (3): 483–98. doi:10.3171/2014.11.JNS14315. PMID 25555079.
- Purves 2012, p. 724.
- Cipolla, M.J. (January 1, 2009). Anatomy and Ultrastructure. Morgan & Claypool Life Sciences. Archived from the original on October 1, 2017.
- "A Surgeon's-Eye View of the Brain". NPR.org. Archived from the original on November 7, 2017.
- Sampaio-Baptista, C; Johansen-Berg, H (December 20, 2017). "White Matter Plasticity in the Adult Brain". Neuron. 96 (6): 1239–1251. doi:10.1016/j.neuron.2017.11.026. PMC 5766826. PMID 29268094.
- Davey, G. (2011). Applied Psychology. John Wiley & Sons. p. 153. ISBN 978-1-4443-3121-9.
- Arsava, E. Y.; Arsava, E. M.; Oguz, K. K.; Topcuoglu, M. A. (2019). "Occipital petalia as a predictive imaging sign for transverse sinus dominance". Neurological Research. 41 (4): 306–311. doi:10.1080/01616412.2018.1560643. PMID 30601110. S2CID 58546404.
- Ackerman, S. (1992). Discovering the brain. Washington, D.C.: National Academy Press. pp. 22–25. ISBN 978-0-309-04529-2.
- Larsen 2001, pp. 455–456.
- Kandel, E.R.; Schwartz, J.H.; Jessel T.M. (2000). Principles of Neural Science. McGraw-Hill Professional. p. 324. ISBN 978-0-8385-7701-1.
- Guyton & Hall 2011, p. 574.
- Guyton & Hall 2011, p. 667.
- Principles of Anatomy and Physiology 12th Edition – Tortora, p. 519.
- Freberg, L. (2009). Discovering Biological Psychology. Cengage Learning. pp. 44–46. ISBN 978-0-547-17779-3.
- Kolb, B.; Whishaw, I. (2009). Fundamentals of Human Neuropsychology. Macmillan. pp. 73–75. ISBN 978-0-7167-9586-5.
- Pocock 2006, p. 64.
- Purves 2012, p. 399.
- Gray's Anatomy 2008, pp. 325–6.
- Goll, Y.; Atlan, G.; Citri, A. (August 2015). "Attention: the claustrum". Trends in Neurosciences. 38 (8): 486–95. doi:10.1016/j.tins.2015.05.006. PMID 26116988. S2CID 38353825.
- Goard, M.; Dan, Y. (October 4, 2009). "Basal forebrain activation enhances cortical coding of natural scenes". Nature Neuroscience. 12 (11): 1444–1449. doi:10.1038/nn.2402. PMC 3576925. PMID 19801988.
- Guyton & Hall 2011, p. 699.
- Gray's Anatomy 2008, p. 298.
- Netter, F. (2014). Atlas of Human Anatomy Including Student Consult Interactive Ancillaries and Guides (6th ed.). Philadelphia, Penn.: W B Saunders Co. p. 114. ISBN 978-1-4557-0418-7.
- Gray's Anatomy 2008, p. 297.
- Guyton & Hall 2011, pp. 698–9.
- Squire 2013, pp. 761–763.
- Gray's Anatomy 2008, p. 275.
- Guyton & Hall 2011, p. 691.
- Purves 2012, p. 377.
- Azevedo, F.; et al. (April 10, 2009). "Equal numbers of neuronal and nonneuronal cells make the human brain an isometrically scaled-up primate brain". The Journal of Comparative Neurology. 513 (5): 532–541. doi:10.1002/cne.21974. PMID 19226510. S2CID 5200449.
despite the widespread quotes that the human brain contains 100 billion neurons and ten times more glial cells, the absolute number of neurons and glial cells in the human brain remains unknown. Here we determine these numbers by using the isotropic fractionator and compare them with the expected values for a human-sized primate. We find that the adult male human brain contains on average 86.1 ± 8.1 billion NeuN-positive cells (“neurons”) and 84.6 ± 9.8 billion NeuN-negative (“nonneuronal”) cells.
- Pavel, Fiala; Jiří, Valenta (January 1, 2013). Central Nervous System. Karolinum Press. p. 79. ISBN 978-80-246-2067-1.
- Polyzoidis, S.; Koletsa, T.; Panagiotidou, S.; Ashkan, K.; Theoharides, T.C. (2015). "Mast cells in meningiomas and brain inflammation". Journal of Neuroinflammation. 12 (1): 170. doi:10.1186/s12974-015-0388-3. PMC 4573939. PMID 26377554.
- Guyton & Hall 2011, pp. 748–749.
- Budzyński, J; Kłopocka, M. (2014). "Brain-gut axis in the pathogenesis of Helicobacter pylori infection". World J. Gastroenterol. 20 (18): 5212–25. doi:10.3748/wjg.v20.i18.5212. PMC 4017036. PMID 24833851.
- Carabotti, M.; Scirocco, A.; Maselli, M.A.; Severi, C. (2015). "The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems". Ann Gastroenterol. 28 (2): 203–209. PMC 4367209. PMID 25830558.
- Sjöstedt, Evelina; Fagerberg, Linn; Hallström, Björn M.; Häggmark, Anna; Mitsios, Nicholas; Nilsson, Peter; Pontén, Fredrik; Hökfelt, Tomas; Uhlén, Mathias (June 15, 2015). "Defining the human brain proteome using transcriptomics and antibody-based profiling with a focus on the cerebral cortex". PLOS ONE. 10 (6): e0130028. Bibcode:2015PLoSO..1030028S. doi:10.1371/journal.pone.0130028. ISSN 1932-6203. PMC 4468152. PMID 26076492.
- Gray's Anatomy 2008, pp. 242–244.
- Purves 2012, p. 742.
- Gray's Anatomy 2008, p. 243.
- Iliff, JJ; Nedergaard, M (June 2013). "Is there a cerebral lymphatic system?". Stroke. 44 (6 Suppl 1): S93-5. doi:10.1161/STROKEAHA.112.678698. PMC 3699410. PMID 23709744.
- Gaillard, F. "Glymphatic pathway". radiopaedia.org. Archived from the original on October 30, 2017.
- Bacyinski A, Xu M, Wang W, Hu J (November 2017). "The Paravascular Pathway for Brain Waste Clearance: Current Understanding, Significance and Controversy". Frontiers in Neuroanatomy. 11: 101. doi:10.3389/fnana.2017.00101. PMC 5681909. PMID 29163074.
The paravascular pathway, also known as the “glymphatic” pathway, is a recently described system for waste clearance in the brain. According to this model, cerebrospinal fluid (CSF) enters the paravascular spaces surrounding penetrating arteries of the brain, mixes with interstitial fluid (ISF) and solutes in the parenchyma, and exits along paravascular spaces of draining veins. ... In addition to Aβ clearance, the glymphatic system may be involved in the removal of other interstitial solutes and metabolites. By measuring the lactate concentration in the brains and cervical lymph nodes of awake and sleeping mice, Lundgaard et al. (2017) demonstrated that lactate can exit the CNS via the paravascular pathway. Their analysis took advantage of the substantiated hypothesis that glymphatic function is promoted during sleep (Xie et al., 2013; Lee et al., 2015; Liu et al., 2017).
- Dissing-Olesen, L.; Hong, S.; Stevens, B. (August 2015). "New brain lymphatic vessels drain old concepts". EBioMedicine. 2 (8): 776–7. doi:10.1016/j.ebiom.2015.08.019. PMC 4563157. PMID 26425672.
- Sun, BL; Wang, LH; Yang, T; Sun, JY; Mao, LL; Yang, MF; Yuan, H; Colvin, RA; Yang, XY (April 2018). "Lymphatic drainage system of the brain: A novel target for intervention of neurological diseases". Progress in Neurobiology. 163–164: 118–143. doi:10.1016/j.pneurobio.2017.08.007. PMID 28903061. S2CID 6290040.
- Gray's Anatomy 2008, p. 247.
- Gray's Anatomy 2008, pp. 251–2.
- Gray's Anatomy 2008, p. 250.
- Gray's Anatomy 2008, p. 248.
- Gray's Anatomy 2008, p. 251.
- Gray's Anatomy 2008, pp. 254–6.
- Elsevier's 2007, pp. 311–4.
- Daneman, R.; Zhou, L.; Kebede, A.A.; Barres, B.A. (November 25, 2010). "Pericytes are required for blood-brain barrier integrity during embryogenesis". Nature. 468 (7323): 562–6. Bibcode:2010Natur.468..562D. doi:10.1038/nature09513. PMC 3241506. PMID 20944625.
- Laterra, J.; Keep, R.; Betz, L.A.; et al. (1999). "Blood–cerebrospinal fluid barrier". Basic neurochemistry: molecular, cellular and medical aspects (6th ed.). Philadelphia: Lippincott-Raven.
- Sadler, T. (2010). Langman's medical embryology (11th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 293. ISBN 978-0-7817-9069-7.
- Larsen 2001, p. 419.
- Larsen 2001, pp. 85–88.
- Purves 2012, pp. 480–482.
- Larsen 2001, pp. 445–446.
- "OpenStax CNX". cnx.org. Archived from the original on May 5, 2015. Retrieved May 5, 2015.
- Larsen 2001, pp. 85–87.
- Purves 2012, pp. 481–484.
- Purves, Dale; Augustine, George J; Fitzpatrick, David; Katz, Lawrence C; LaMantia, Anthony-Samuel; McNamara, James O; Williams, S Mark, eds. (2001). "Rhombomeres". Neuroscience (2nd ed.). ISBN 978-0-87893-742-4.
- Chen, X. (2012). Mechanical Self-Assembly: Science and Applications. Springer Science & Business Media. pp. 188–189. ISBN 978-1-4614-4562-3.
- Ronan, L; Voets, N; Rua, C; Alexander-Bloch, A; Hough, M; Mackay, C; Crow, TJ; James, A; Giedd, JN; Fletcher, PC (August 2014). "Differential tangential expansion as a mechanism for cortical gyrification". Cerebral Cortex. 24 (8): 2219–28. doi:10.1093/cercor/bht082. PMC 4089386. PMID 23542881.
- Van Essen, DC (January 23, 1997). "A tension-based theory of morphogenesis and compact wiring in the central nervous system". Nature. 385 (6614): 313–8. Bibcode:1997Natur.385..313E. doi:10.1038/385313a0. PMID 9002514. S2CID 4355025.
- Borrell, V (January 24, 2018). "How Cells Fold the Cerebral Cortex". The Journal of Neuroscience. 38 (4): 776–783. doi:10.1523/JNEUROSCI.1106-17.2017. PMC 6596235. PMID 29367288.
- Florio, M.; et al. (March 27, 2015). "Human-specific gene ARHGAP11B promotes basal progenitor amplification and neocortex expansion". Science. 347 (6229): 1465–70. Bibcode:2015Sci...347.1465F. doi:10.1126/science.aaa1975. PMID 25721503. S2CID 34506325.
- "Parts of the Brain | Introduction to Psychology". courses.lumenlearning.com. Retrieved September 20, 2019.
- Guyton & Hall 2011, p. 685.
- Guyton & Hall 2011, p. 687.
- Guyton & Hall 2011, p. 686.
- Guyton & Hall 2011, pp. 698, 708.
- Davidson's 2010, p. 1139.
- Hellier, J. (2014). The Brain, the Nervous System, and Their Diseases [3 volumes]. ABC-CLIO. pp. 300–303. ISBN 978-1-61069-338-7.
- Guyton & Hall 2011, pp. 571–576.
- Guyton & Hall 2011, pp. 573–574.
- Guyton & Hall 2011, pp. 623–631.
- Guyton & Hall 2011, pp. 739–740.
- Pocock 2006, pp. 138–139.
- Squire 2013, pp. 525–526.
- Guyton & Hall 2011, pp. 647–648.
- Guyton & Hall 2011, pp. 202–203.
- Guyton & Hall 2011, pp. 205–208.
- Guyton & Hall 2011, pp. 505–509.
- "Brain Basics: Understanding Sleep | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Archived from the original on December 22, 2017.
- Guyton & Hall 2011, p. 723.
- Davis, J.F.; Choi, D.L.; Benoit, S.C. (2011). "24. Orexigenic Hypothalamic Peptides Behavior and Feeding – 24.5 Orexin". In Preedy, V.R.; Watson, R.R.; Martin, C.R. (eds.). Handbook of Behavior, Food and Nutrition. Springer. pp. 361–362. ISBN 978-0-387-92271-3.
- Squire 2013, p. 800.
- Squire 2013, p. 803.
- Squire 2013, p. 805.
- Guyton & Hall 2011, pp. 720–2.
- Poeppel, D.; Emmorey, K.; Hickok, G.; Pylkkänen, L. (October 10, 2012). "Towards a new neurobiology of language". The Journal of Neuroscience. 32 (41): 14125–14131. doi:10.1523/JNEUROSCI.3244-12.2012. PMC 3495005. PMID 23055482.
- Hickok, G (September 2009). "The functional neuroanatomy of language". Physics of Life Reviews. 6 (3): 121–143. Bibcode:2009PhLRv...6..121H. doi:10.1016/j.plrev.2009.06.001. PMC 2747108. PMID 20161054.
- Fedorenko, E.; Kanwisher, N. (2009). "Neuroimaging of language: why hasn't a clearer picture emerged?". Language and Linguistics Compass. 3 (4): 839–865. doi:10.1111/j.1749-818x.2009.00143.x. S2CID 2833893.
- Damasio, H. (2001). "Neural basis of language disorders". In Chapey, Roberta (ed.). Language intervention strategies in aphasia and related neurogenic communication disorders (4th ed.). Lippincott Williams & Wilkins. pp. 18–36. ISBN 978-0-7817-2133-2. OCLC 45952164.
- Berntson, G.; Cacioppo, J. (2009). Handbook of Neuroscience for the Behavioral Sciences, Volume 1. John Wiley & Sons. p. 145. ISBN 978-0-470-08355-0.
- Hellier, J. (2014). The Brain, the Nervous System, and Their Diseases [3 volumes]. ABC-CLIO. p. 1135. ISBN 978-1-61069-338-7.
- Kolb, B.; Whishaw, I.Q. (2013). Introduction to Brain and Behavior. Macmillan Higher Education. p. 296. ISBN 978-1-4641-3960-4.
- Sherwood, L. (2012). Human Physiology: From Cells to Systems. Cengage Learning. p. 181. ISBN 978-1-133-70853-7.
- Kalat, J (2015). Biological Psychology. Cengage Learning. p. 425. ISBN 978-1-305-46529-9.
- Cowin, S.C.; Doty, S.B. (2007). Tissue Mechanics. Springer Science & Business Media. p. 4. ISBN 978-0-387-49985-7.
- Morris, C.G.; Maisto, A.A. (2011). Understanding Psychology. Prentice Hall. p. 56. ISBN 978-0-205-76906-3.
- Kolb, B.; Whishaw, I.Q. (2013). Introduction to Brain and Behavior (Loose-Leaf). Macmillan Higher Education. pp. 524–549. ISBN 978-1-4641-3960-4.
- Schacter, D.L.; Gilbert, D.T.; Wegner, D.M. (2009). Introducing Psychology. Macmillan. p. 80. ISBN 978-1-4292-1821-4.
- Sander, David (2013). Armony, J.; Vuilleumier, Patrik (eds.). The Cambridge handbook of human affective neuroscience. Cambridge: Cambridge Univ. Press. p. 16. ISBN 978-0-521-17155-7.
- Lindquist, KA.; Wager, TD.; Kober, H; Bliss-Moreau, E; Barrett, LF (May 23, 2012). "The brain basis of emotion: A meta-analytic review". Behavioral and Brain Sciences. 35 (3): 121–143. doi:10.1017/S0140525X11000446. PMC 4329228. PMID 22617651.
- Phan, KL; Wager, Tor; Taylor, SF.; Liberzon, l (June 1, 2002). "Functional Neuroanatomy of Emotion: A Meta-Analysis of Emotion Activation Studies in PET and fMRI". NeuroImage. 16 (2): 331–348. doi:10.1006/nimg.2002.1087. PMID 12030820. S2CID 7150871.
- Malenka, RC; Nestler, EJ; Hyman, SE (2009). "Preface". In Sydor, A; Brown, RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. xiii. ISBN 978-0-07-148127-4.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 14: Higher Cognitive Function and Behavioral Control". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 6: Widely Projecting Systems: Monoamines, Acetylcholine, and Orexin". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
- Diamond, A (2013). "Executive functions". Annual Review of Psychology. 64: 135–168. doi:10.1146/annurev-psych-113011-143750. PMC 4084861. PMID 23020641.
Figure 4: Executive functions and related terms Archived May 9, 2018, at the Wayback Machine - Hyun, J.C.; Weyandt, L.L.; Swentosky, A. (2014). "Chapter 2: The Physiology of Executive Functioning". In Goldstein, S.; Naglieri, J. (eds.). Handbook of Executive Functioning. New York: Springer. pp. 13–23. ISBN 978-1-4614-8106-5.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 14: Higher Cognitive Function and Behavioral Control". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
In conditions in which prepotent responses tend to dominate behavior, such as in drug addiction, where drug cues can elicit drug seeking (Chapter 16), or in attention deficit hyperactivity disorder (ADHD; described below), significant negative consequences can result. ... ADHD can be conceptualized as a disorder of executive function; specifically, ADHD is characterized by reduced ability to exert and maintain cognitive control of behavior. Compared with healthy individuals, those with ADHD have diminished ability to suppress inappropriate prepotent responses to stimuli (impaired response inhibition) and diminished ability to inhibit responses to irrelevant stimuli (impaired interference suppression). ... Functional neuroimaging in humans demonstrates activation of the prefrontal cortex and caudate nucleus (part of the dorsal striatum) in tasks that demand inhibitory control of behavior. ... Early results with structural MRI show a thinner cerebral cortex, across much of the cerebrum, in ADHD subjects compared with age-matched controls, including areas of [the] prefrontal cortex involved in working memory and attention.
- Pocock 2006, p. 68.
- Clark, B.D.; Goldberg, E.M.; Rudy, B. (December 2009). "Electrogenic tuning of the axon initial segment". The Neuroscientist. 15 (6): 651–68. doi:10.1177/1073858409341973. PMC 2951114. PMID 20007821.
- Pocock 2006, pp. 70–74.
- "NIMH » Brain Basics". www.nimh.nih.gov. Archived from the original on March 26, 2017. Retrieved March 26, 2017.
- Purves, Dale (2011). Neuroscience (5. ed.). Sunderland, Mass.: Sinauer. p. 139. ISBN 978-0-87893-695-3.
- Swaminathan, N (April 29, 2008). "Why Does the Brain Need So Much Power?". Scientific American. Archived from the original on January 27, 2014. Retrieved November 19, 2010.
- Wasserman DH (January 2009). "Four grams of glucose". American Journal of Physiology. Endocrinology and Metabolism. 296 (1): E11–21. doi:10.1152/ajpendo.90563.2008. PMC 2636990. PMID 18840763.
Four grams of glucose circulates in the blood of a person weighing 70 kg. This glucose is critical for normal function in many cell types. In accordance with the importance of these 4 g of glucose, a sophisticated control system is in place to maintain blood glucose constant. Our focus has been on the mechanisms by which the flux of glucose from liver to blood and from blood to skeletal muscle is regulated. ... The brain consumes ∼60% of the blood glucose used in the sedentary, fasted person. ... The amount of glucose in the blood is preserved at the expense of glycogen reservoirs (Fig. 2). In postabsorptive humans, there are ∼100 g of glycogen in the liver and ∼400 g of glycogen in muscle. Carbohydrate oxidation by the working muscle can go up by ∼10-fold with exercise, and yet after 1 h, blood glucose is maintained at ∼4 g. ... It is now well established that both insulin and exercise cause translocation of GLUT4 to the plasma membrane. Except for the fundamental process of GLUT4 translocation, [muscle glucose uptake (MGU)] is controlled differently with exercise and insulin. Contraction-stimulated intracellular signaling (52, 80) and MGU (34, 75, 77, 88, 91, 98) are insulin independent. Moreover, the fate of glucose extracted from the blood is different in response to exercise and insulin (91, 105). For these reasons, barriers to glucose flux from blood to muscle must be defined independently for these two controllers of MGU.
- Quistorff, B; Secher, N; Van Lieshout, J (July 24, 2008). "Lactate fuels the human brain during exercise". The FASEB Journal. 22 (10): 3443–3449. doi:10.1096/fj.08-106104. PMID 18653766. S2CID 15394163.
- Obel, L.F.; Müller, M.S.; Walls, A.B.; Sickmann, H.M.; Bak, L.K.; Waagepetersen, H.S.; Schousboe, A. (2012). "Brain glycogen-new perspectives on its metabolic function and regulation at the subcellular level". Frontiers in Neuroenergetics. 4: 3. doi:10.3389/fnene.2012.00003. PMC 3291878. PMID 22403540.
- Marin-Valencia, I.; et al. (February 2013). "Heptanoate as a neural fuel: energetic and neurotransmitter precursors in normal and glucose transporter I-deficient (G1D) brain". Journal of Cerebral Blood Flow and Metabolism. 33 (2): 175–82. doi:10.1038/jcbfm.2012.151. PMC 3564188. PMID 23072752.
- Tsuji, A. (2005). "Small molecular drug transfer across the blood-brain barrier via carrier-mediated transport systems". NeuroRx. 2 (1): 54–62. doi:10.1602/neurorx.2.1.54. PMC 539320. PMID 15717057.
Uptake of valproic acid was reduced in the presence of medium-chain fatty acids such as hexanoate, octanoate, and decanoate, but not propionate or butyrate, indicating that valproic acid is taken up into the brain via a transport system for medium-chain fatty acids, not short-chain fatty acids. ... Based on these reports, valproic acid is thought to be transported bidirectionally between blood and brain across the BBB via two distinct mechanisms, monocarboxylic acid-sensitive and medium-chain fatty acid-sensitive transporters, for efflux and uptake, respectively.
- Vijay, N.; Morris, M.E. (2014). "Role of monocarboxylate transporters in drug delivery to the brain". Curr. Pharm. Des. 20 (10): 1487–98. doi:10.2174/13816128113199990462. PMC 4084603. PMID 23789956.
Monocarboxylate transporters (MCTs) are known to mediate the transport of short chain monocarboxylates such as lactate, pyruvate and butyrate. ... MCT1 and MCT4 have also been associated with the transport of short chain fatty acids such as acetate and formate which are then metabolized in the astrocytes [78].
- Clark, D.D.; Sokoloff. L. (1999). Siegel, G.J.; Agranoff, B.W.; Albers, R.W.; Fisher, S.K.; Uhler, M.D. (eds.). Basic Neurochemistry: Molecular, Cellular and Medical Aspects. Philadelphia: Lippincott. pp. 637–670. ISBN 978-0-397-51820-3.
- Mrsulja, B.B. (2012). Pathophysiology of Cerebral Energy Metabolism. Springer Science & Business Media. pp. 2–3. ISBN 978-1-4684-3348-7.
- Raichle, M.; Gusnard, DA (2002). "Appraising the brain's energy budget". Proc. Natl. Acad. Sci. U.S.A. 99 (16): 10237–10239. Bibcode:2002PNAS...9910237R. doi:10.1073/pnas.172399499. PMC 124895. PMID 12149485.
- Gianaros, Peter J.; Gray, Marcus A.; Onyewuenyi, Ikechukwu; Critchley, Hugo D. (2010). "Chapter 50. Neuroimaging methods in behavioral medicine". In Steptoe, A. (ed.). Handbook of Behavioral Medicine: Methods and Applications. Springer Science & Business Media. p. 770. doi:10.1007/978-0-387-09488-5_50. ISBN 978-0-387-09488-5.
- Kuzawa, C. W.; Chugani, H. T.; Grossman, L. I.; Lipovich, L.; Muzik, O.; Hof, P. R.; Wildman, D. E.; Sherwood, C. C.; Leonard, W. R.; Lange, N. (September 9, 2014). "Metabolic costs and evolutionary implications of human brain development". Proceedings of the National Academy of Sciences. 111 (36): 13010–13015. Bibcode:2014PNAS..11113010K. doi:10.1073/pnas.1323099111. ISSN 0027-8424. PMC 4246958. PMID 25157149.
- "Brain may flush out toxins during sleep". National Institutes of Health. Archived from the original on October 20, 2013. Retrieved October 25, 2013.
- Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O'Donnell J, Christensen DJ, Nicholson C, Iliff JJ, Takano T, Deane R, Nedergaard M (October 2013). "Sleep drives metabolite clearance from the adult brain". Science. 342 (6156): 373–377. Bibcode:2013Sci...342..373X. doi:10.1126/science.1241224. PMC 3880190. PMID 24136970.
Thus, the restorative function of sleep may be a consequence of the enhanced removal of potentially neurotoxic waste products that accumulate in the awake central nervous system.
- Tononi, Guilio; Cirelli, Chiara (August 2013). "Perchance to Prune" (PDF). Scientific American. 309 (2): 34–39. Bibcode:2013SciAm.309b..34T. doi:10.1038/scientificamerican0813-34. PMID 23923204. S2CID 54052089. Archived from the original (PDF) on December 26, 2018.
- Van Essen, D.C.; et al. (October 2012). "The Human Connectome Project: A data acquisition perspective". NeuroImage. 62 (4): 2222–2231. doi:10.1016/j.neuroimage.2012.02.018. PMC 3606888. PMID 22366334.
- Jones, E.G.; Mendell, L.M. (April 30, 1999). "Assessing the Decade of the Brain". Science. 284 (5415): 739. Bibcode:1999Sci...284..739J. doi:10.1126/science.284.5415.739. PMID 10336393. S2CID 13261978.
- "A $4.5 Billion Price Tag for the BRAIN Initiative?". Science | AAAS. June 5, 2014. Archived from the original on June 18, 2017.
- Towle, V.L.; et al. (January 1993). "The spatial location of EEG electrodes: locating the best-fitting sphere relative to cortical anatomy". Electroencephalography and Clinical Neurophysiology. 86 (1): 1–6. doi:10.1016/0013-4694(93)90061-y. PMID 7678386.
- Purves 2012, pp. 632–633.
- Silverstein, J. (2012). "Mapping the Motor and Sensory Cortices: A Historical Look and a Current Case Study in Sensorimotor Localization and Direct Cortical Motor Stimulation". The Neurodiagnostic Journal. 52 (1): 54–68. PMID 22558647. Archived from the original on November 17, 2012.
- Boraud, T.; Bezard, E.; et al. (2002). "From single extracellular unit recording in experimental and human Parkinsonism to the development of a functional concept of the role played by the basal ganglia in motor control". Progress in Neurobiology. 66 (4): 265–283. doi:10.1016/s0301-0082(01)00033-8. PMID 11960681. S2CID 23389986.
- Lancaster, MA; Renner, M; Martin, CA; Wenzel, D; Bicknell, LS; Hurles, ME; Homfray, T; Penninger, JM; Jackson, AP; Knoblich, JA (September 19, 2013). "Cerebral organoids model human brain development and microcephaly". Nature. 501 (7467): 373–9. Bibcode:2013Natur.501..373L. doi:10.1038/nature12517. PMC 3817409. PMID 23995685.
- Lee, CT; Bendriem, RM; Wu, WW; Shen, RF (August 20, 2017). "3D brain Organoids derived from pluripotent stem cells: promising experimental models for brain development and neurodegenerative disorders". Journal of Biomedical Science. 24 (1): 59. doi:10.1186/s12929-017-0362-8. PMC 5563385. PMID 28822354.
- "Magnetic Resonance, a critical peer-reviewed introduction; functional MRI". European Magnetic Resonance Forum. Archived from the original on June 2, 2017. Retrieved June 30, 2017.
- Buxton, R.; Uludag, K.; Liu, T. (2004). "Modeling the haemodynamic response to brain activation". NeuroImage. 23: S220–S233. CiteSeerX 10.1.1.329.29. doi:10.1016/j.neuroimage.2004.07.013. PMID 15501093. S2CID 8736954.
- Biswal, B.B. (August 15, 2012). "Resting state fMRI: a personal history". NeuroImage. 62 (2): 938–44. doi:10.1016/j.neuroimage.2012.01.090. PMID 22326802. S2CID 93823.
- Purves 2012, p. 20.
- Kane, R.L.; Parsons, T.D. (2017). The Role of Technology in Clinical Neuropsychology. Oxford University Press. p. 399. ISBN 978-0-19-023473-7.
Irimia, Chambers, Torgerson, and Van Horn (2012) provide a first-step graphic on how best to display connectivity findings, as is presented in Figure 13.15. This is referred to as a connectogram.
- Andrews, D.G. (2001). Neuropsychology. Psychology Press. ISBN 978-1-84169-103-9.
- Lepage, M. (2010). "Research at the Brain Imaging Centre". Douglas Mental Health University Institute. Archived from the original on March 5, 2012.
- Steward, C.A.; et al. (2017). "Genome annotation for clinical genomic diagnostics: strengths and weaknesses". Genome Med. 9 (1): 49. doi:10.1186/s13073-017-0441-1. PMC 5448149. PMID 28558813.
- Harrow, J.; et al. (September 2012). "GENCODE: the reference human genome annotation for The ENCODE Project". Genome Res. 22 (9): 1760–74. doi:10.1101/gr.135350.111. PMC 3431492. PMID 22955987.
- Gibson G, Muse SV (April 20, 2009). A primer of genome science (3rd ed.). Sunderland, MA: Sinauer Associates. ISBN 9780878932368.
- "The human proteome in brain – The Human Protein Atlas". www.proteinatlas.org. Archived from the original on September 29, 2017. Retrieved September 29, 2017.
- Uhlén, Mathias; Fagerberg, Linn; Hallström, Björn M.; Lindskog, Cecilia; Oksvold, Per; Mardinoglu, Adil; Sivertsson, Åsa; Kampf, Caroline; Sjöstedt, Evelina (January 23, 2015). "Tissue-based map of the human proteome". Science. 347 (6220): 1260419. doi:10.1126/science.1260419. ISSN 0036-8075. PMID 25613900. S2CID 802377.
- Warden, A (2017). "Gene expression profiling in the human alcoholic brain". Neuropharmacology. 122: 161–174. doi:10.1016/j.neuropharm.2017.02.017. PMC 5479716. PMID 28254370.
- Farris, S.P.; et al. (2015). "Applying the new genomics to alcohol dependence". Alcohol. 49 (8): 825–36. doi:10.1016/j.alcohol.2015.03.001. PMC 4586299. PMID 25896098.
- Rozycka, A; Liguz-Lecznar, M (August 2017). "The space where aging acts: focus on the GABAergic synapse". Aging Cell. 16 (4): 634–643. doi:10.1111/acel.12605. PMC 5506442. PMID 28497576.
- Flores, CE; Méndez, P (2014). "Shaping inhibition: activity dependent structural plasticity of GABAergic synapses". Frontiers in Cellular Neuroscience. 8: 327. doi:10.3389/fncel.2014.00327. PMC 4209871. PMID 25386117.
- "Brain Injury, Traumatic". Medcyclopaedia. GE. Archived from the original on May 26, 2011.
- Dawodu, S.T. (March 9, 2017). "Traumatic Brain Injury (TBI) – Definition and Pathophysiology: Overview, Epidemiology, Primary Injury". Medscape. Archived from the original on April 9, 2017.
- Davidson's 2010, pp. 1196–7.
- Davidson's 2010, pp. 1205–15.
- Davidson's 2010, pp. 1216–7.
- Volkow, N.D.; Koob, G.F.; McLellan, A.T. (January 2016). "Neurobiologic advances from the brain disease model of addiction". The New England Journal of Medicine. 374 (4): 363–371. doi:10.1056/NEJMra1511480. PMC 6135257. PMID 26816013.
- Simpson, J.M.; Moriarty, G.L. (2013). Multimodal Treatment of Acute Psychiatric Illness: A Guide for Hospital Diversion. Columbia University Press. pp. 22–24. ISBN 978-0-231-53609-7.
- Davidson's 2010, pp. 1172–9.
- "Status Epilepticus". Epilepsy Foundation.
- Moore, S.P. (2005). The Definitive Neurological Surgery Board Review. Lippincott Williams & Wilkins. p. 112. ISBN 978-1-4051-0459-3.
- Pennington, B.F. (2008). Diagnosing Learning Disorders, Second Edition: A Neuropsychological Framework. Guilford Press. pp. 3–10. ISBN 978-1-60623-786-1.
- Govaert, P.; de Vries, L.S. (2010). An Atlas of Neonatal Brain Sonography: (CDM 182–183). John Wiley & Sons. pp. 89–92. ISBN 978-1-898683-56-8.
- Perese, E.F. (2012). Psychiatric Advanced Practice Nursing: A Biopsychsocial Foundation for Practice. F.A. Davis. pp. 82–88. ISBN 978-0-8036-2999-8.
- Kearney, C.; Trull, T.J. (2016). Abnormal Psychology and Life: A Dimensional Approach. Cengage Learning. p. 395. ISBN 978-1-337-09810-6.
- Stevenson, D.K.; Sunshine, P.; Benitz, W.E. (2003). Fetal and Neonatal Brain Injury: Mechanisms, Management and the Risks of Practice. Cambridge University Press. p. 191. ISBN 978-0-521-80691-6.
- Dewhurst, John (2012). Dewhurst's Textbook of Obstetrics and Gynaecology. John Wiley & Sons. p. 43. ISBN 978-0-470-65457-6.
- Harbison, J.; Massey, A.; Barnett, L.; Hodge, D.; Ford, G.A. (June 1999). "Rapid ambulance protocol for acute stroke". Lancet. 353 (9168): 1935. doi:10.1016/S0140-6736(99)00966-6. PMID 10371574. S2CID 36692451.
- Davidson's 2010, p. 1183.
- Davidson's 2010, pp. 1180–1.
- Davidson's 2010, pp. 1181, 1183–1185.
- Davidson's 2010, pp. 1183–1185.
- Davidson's 2010, pp. 1185–1189.
- Goyal, M.; et al. (April 2016). "Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials". The Lancet. 387 (10029): 1723–1731. doi:10.1016/S0140-6736(16)00163-X. PMID 26898852. S2CID 34799180.
- Saver, J. L. (December 8, 2005). "Time is brain—quantified". Stroke. 37 (1): 263–266. doi:10.1161/01.STR.0000196957.55928.ab. PMID 16339467.
- Winstein, C.J.; et al. (June 2016). "Guidelines for adult stroke rehabilitation and recovery". Stroke. 47 (6): e98–e169. doi:10.1161/STR.0000000000000098. PMID 27145936. S2CID 4967333.
- Kuźma, Elżbieta; Lourida, Ilianna; Moore, Sarah F.; Levine, Deborah A.; Ukoumunne, Obioha C.; Llewellyn, David J. (November 2018). "Stroke and dementia risk: A systematic review and meta-analysis". Alzheimer's & Dementia. 14 (11): 1416–1426. doi:10.1016/j.jalz.2018.06.3061. ISSN 1552-5260. PMC 6231970. PMID 30177276.
- Goila, AK; Pawar, M (2009). "The diagnosis of brain death". Indian Journal of Critical Care Medicine. 13 (1): 7–11. doi:10.4103/0972-5229.53108. PMC 2772257. PMID 19881172.
- Wijdicks, EFM (January 8, 2002). "Brain death worldwide: accepted fact but no global consensus in diagnostic criteria". Neurology. 58 (1): 20–25. doi:10.1212/wnl.58.1.20. PMID 11781400. S2CID 219203458.
- Dhanwate, AD (September 2014). "Brainstem death: A comprehensive review in Indian perspective". Indian Journal of Critical Care Medicine. 18 (9): 596–605. doi:10.4103/0972-5229.140151. PMC 4166875. PMID 25249744.
- Davidson's 2010, p. 1158.
- Davidson's 2010, p. 200.
- Urden, L.D.; Stacy, K.M.; Lough, M.E. (2013). Priorities in Critical Care Nursing – E-Book. Elsevier Health Sciences. pp. 112–113. ISBN 978-0-323-29414-0.
- Domínguez, J.F.; Lewis, E.D.; Turner, R.; Egan, G.F. (2009). Chiao, J.Y. (ed.). The Brain in Culture and Culture in the Brain: A Review of Core Issues in Neuroanthropology. Progress in Brain Research. Special issue: Cultural Neuroscience: Cultural Influences on Brain Function. Vol. 178. pp. 43–6. doi:10.1016/S0079-6123(09)17804-4. ISBN 978-0-444-53361-6. PMID 19874961.
- "Cultural Environment Influences Brain Function | Psych Central News". Psych Central News. August 4, 2010. Archived from the original on January 17, 2017.
- Macmillan, Malcolm B. (2000). An Odd Kind of Fame: Stories of Phineas Gage. MIT Press. ISBN 978-0-262-13363-0.
- Rescher, N. (1992). G. W. Leibniz's Monadology. Psychology Press. p. 83. ISBN 978-0-415-07284-7.
- Hart, WD (1996). Guttenplan S (ed.). A Companion to the Philosophy of Mind. Blackwell. pp. 265–267.
- Churchland, P.S. (1989). "Ch. 8". Neurophilosophy. MIT Press. ISBN 978-0-262-53085-9.
- Selimbeyoglu, Aslihan; Parvizi, J (2010). "Electrical stimulation of the human brain: perceptual and behavioral phenomena reported in the old and new literature". Frontiers in Human Neuroscience. 4: 46. doi:10.3389/fnhum.2010.00046. PMC 2889679. PMID 20577584.
- Schwartz, J.H. Appendix D: Consciousness and the Neurobiology of the Twenty-First Century. In Kandel, E.R.; Schwartz, J.H.; Jessell, T.M. (2000). Principles of Neural Science, 4th Edition.
- Lilienfeld, S.O.; Lynn, S.J.; Ruscio, J.; Beyerstein, B.L. (2011). 50 Great Myths of Popular Psychology: Shattering Widespread Misconceptions about Human Behavior. John Wiley & Sons. p. 89. ISBN 978-1-4443-6074-5.
- McDaniel, M. (2005). "Big-brained people are smarter" (PDF). Intelligence. 33 (4): 337–346. doi:10.1016/j.intell.2004.11.005. Archived (PDF) from the original on September 6, 2014.
- Luders, E.; et al. (September 2008). "Mapping the relationship between cortical convolution and intelligence: effects of gender". Cerebral Cortex. 18 (9): 2019–26. doi:10.1093/cercor/bhm227. PMC 2517107. PMID 18089578.
- Hoppe, C; Stojanovic, J (2008). "High-Aptitude Minds". Scientific American Mind. 19 (4): 60–67. doi:10.1038/scientificamericanmind0808-60.
- "Tupaia belangeri". The Genome Institute, Washington University. Archived from the original on June 1, 2010. Retrieved January 22, 2016.
- Carrier, Martin; Mittelstrass, Jürgen (1991). Mind, Brain, Behavior: The Mind-body Problem and the Philosophy of Psychology [Geist, Gehirn, Verhalten]. Translated by Lindberg, Steven (revised and expanded English ed.). Berlin: Walter de Gruyter. p. 11. ISBN 9783110128765. Retrieved May 22, 2021.
[...] the Aristotelian view that the soul resides primarily in the heart [...].
- Cobb, Matthew (April 21, 2020). The Idea of the Brain: The Past and Future of Neuroscience. New York: Hachette UK (published 2020). ISBN 9781541646865. Retrieved May 22, 2021.
[...] the ways in which we think about [the brain] are much richer than in the past, not simply because of the amazing facts we have discovered, but above all because of how we interpret them.
- Jarrett, C. (November 17, 2014). Great Myths of the Brain. John Wiley & Sons. ISBN 978-1-118-31271-1.
- Phillips, Helen (July 11, 2002). "Video game "brain damage" claim criticised". New Scientist. Archived from the original on January 11, 2009. Retrieved February 6, 2008.
- Popova, Maria (August 18, 2011). "'Brain Culture': How Neuroscience Became a Pop Culture Fixation". The Atlantic. Archived from the original on July 28, 2017.
- Thornton, Davi Johnson (2011). Brain Culture. Neuroscience and Popular Media. Rutgers University Press. ISBN 978-0-8135-5013-8.
- Cyborgs and Space Archived October 6, 2011, at the Wayback Machine, in Astronautics (September 1960), by Manfred E. Clynes and Nathan S. Kline.
- Bergfelder, Tim (2005). International Adventures: German Popular Cinema and European Co-productions in the 1960s. Berghahn Books. p. 129. ISBN 978-1-57181-538-5.
- Kandel, ER; Schwartz JH; Jessell TM (2000). Principles of Neural Science (4th ed.). New York: McGraw-Hill. ISBN 978-0-8385-7701-1.
- Gross, Charles G. (1987). Adelman, George (ed.). Encyclopedia of neuroscience (PDF) (2. ed.). Boston: Birkhäeuser. pp. 843–847. ISBN 978-0-8176-3335-6. Archived (PDF) from the original on May 5, 2013.
- Bear, M.F.; B.W. Connors; M.A. Paradiso (2001). Neuroscience: Exploring the Brain. Baltimore: Lippincott. ISBN 978-0-7817-3944-3.
- von Staden, p.157
- Swanson, Larry W. (August 12, 2014). Neuroanatomical Terminology: A Lexicon of Classical Origins and Historical Foundations. Oxford University Press. ISBN 978-0-19-534062-4.
- Lokhorst, Gert-Jan (January 1, 2016). "Descartes and the Pineal Gland". The Stanford Encyclopedia of Philosophy. Metaphysics Research Lab, Stanford University. Retrieved March 11, 2017.
- Gross, Charles G. (1999). Brain, vision, memory : tales in the history of neuroscience (1st MIT Press pbk. ed.). Cambridge, Mass.: MIT. pp. 37–51. ISBN 978-0-262-57135-7.
- Marshall, Louise H.; Magoun, Horace W. (March 9, 2013). Discoveries in the Human Brain: Neuroscience Prehistory, Brain Structure, and Function. Springer Science & Business Media. p. 44. ISBN 978-1-475-74997-7.
- Holtz, Anders; Levi, Richard (July 20, 2010). Spinal Cord Injury. Oxford University Press. ISBN 978-0-19-970681-5.
- Tessman, Patrick A.; Suarez, Jose I. (2002). "Influence of early printmaking on the development of neuroanatomy and neurology". Archives of Neurology. 59 (12): 1964–1969. doi:10.1001/archneur.59.12.1964. PMID 12470188.
- O'Connor, James (2003). "Thomas Willis and the background to Cerebri Anatome". Journal of the Royal Society of Medicine. 96 (3): 139–143. doi:10.1177/014107680309600311. PMC 539424. PMID 12612118.
- EMERY, ALAN (October 2000). "A Short History of Neurology: The British Contribution 1660–1910. Edited by F. CLIFFORD ROSE. (Pp. 282; illustrated; £25 Paperback; ISBN 07506 4165 7.) Oxford: Butterworth-Heinemann". Journal of Anatomy. 197 (3): 513–518. doi:10.1046/j.1469-7580.2000.197305131.x. PMC 1468164.
- Olesko, Kathryn M.; Holmes, Frederic L. (1994). Cahan, David (ed.). "Experiment, Quantification, and Discovery: Helmholtz's Early Physiological Researches, 1843-50". Hermann von Helmholtz and the Foundations of Nineteenth Century Science. Berkeley; Los Angeles; London: University of California Press: 50–108.
- Sabbatini, Renato M.E. "Sabbatini, R.M.E.: The Discovery of Bioelectricity. Nerve Conduction". www.cerebromente.org.br. Archived from the original on June 26, 2017. Retrieved June 10, 2017.
- Finkelstein, Gabriel Ward (2013). Emil du Bois-Reymond : neuroscience, self, and society in nineteenth-century Germany. Cambridge, Massachusetts. ISBN 978-1-4619-5032-5. OCLC 864592470.
- Karbowski, Kazimierz (February 14, 2008). "Sixty Years of Clinical Electroencephalography". European Neurology. 30 (3): 170–175. doi:10.1159/000117338. PMID 2192889.
- Pearce, J.M.S. (March 17, 2009). "Marie-Jean-Pierre Flourens (1794–1867) and Cortical Localization". European Neurology. 61 (5): 311–314. doi:10.1159/000206858. PMID 19295220.
- De Carlos, Juan A.; Borrell, José (August 2007). "A historical reflection of the contributions of Cajal and Golgi to the foundations of neuroscience". Brain Research Reviews. 55 (1): 8–16. doi:10.1016/j.brainresrev.2007.03.010. hdl:10261/62299. PMID 17490748. S2CID 7266966.
- Burke, R.E. (April 2007). "Sir Charles Sherrington's The integrative action of the nervous system: a centenary appreciation". Brain. 130 (Pt 4): 887–894. doi:10.1093/brain/awm022. PMID 17438014.
- Squire, Larry R., ed. (1996). The history of neuroscience in autobiography. Washington DC: Society for Neuroscience. pp. 475–97. ISBN 978-0-12-660305-7.
- Cowan, W.M.; Harter, D.H.; Kandel, E.R. (2000). "The emergence of modern neuroscience: Some implications for neurology and psychiatry". Annual Review of Neuroscience. 23: 345–346. doi:10.1146/annurev.neuro.23.1.343. PMID 10845068.
- Brady, Joseph V.; Nauta, Walle J. H. (October 22, 2013). Principles, Practices, and Positions in Neuropsychiatric Research: Proceedings of a Conference Held in June 1970 at the Walter Reed Army Institute of Research, Washington, D.C., in Tribute to Dr. David Mckenzie Rioch upon His Retirement as Director of the Neuropsychiatry Division of That Institute. Elsevier. p. vii. ISBN 978-1-4831-5453-4.
- Adelman, George (January 15, 2010). "The Neurosciences Research Program at MIT and the Beginning of the Modern Field of Neuroscience". Journal of the History of the Neurosciences. 19 (1): 15–23. doi:10.1080/09647040902720651. PMID 20391098. S2CID 21513317.
- Principles of Neural Science, 4th ed. Eric R. Kandel, James H. Schwartz, Thomas M. Jessel, eds. McGraw-Hill:New York, NY. 2000.
- Papez, J.W. (February 1995). "A proposed mechanism of emotion. 1937". The Journal of Neuropsychiatry and Clinical Neurosciences. 7 (1): 103–12. doi:10.1176/jnp.7.1.103. PMID 7711480.
- Lambert, Kelly G. (August 2003). "The life and career of Paul MacLean". Physiology & Behavior. 79 (3): 343–349. doi:10.1016/S0031-9384(03)00147-1. PMID 12954429. S2CID 18596574.
- Chatterjee, Anjan; Coslett, H. Branch (December 2013). The Roots of Cognitive Neuroscience: Behavioral Neurology and Neuropsychology. OUP USA. pp. 337–8. ISBN 978-0-19-539554-9.
- Bliss, Michael (October 1, 2005). Harvey Cushing : A Life in Surgery: A Life in Surgery. USA: Oxford University Press. pp. ix–x. ISBN 978-0-19-534695-4.
- Kretzer, RM; Coon, AL; Tamargo, RJ (June 2010). "Walter E. Dandy's contributions to vascular neurosurgery". Journal of Neurosurgery. 112 (6): 1182–91. doi:10.3171/2009.7.JNS09737. PMID 20515365.
- Glees, Paul (2005). The Human Brain. Cambridge University Press. p. 1. ISBN 978-0-521-01781-7.
- Simpkins, C. Alexander; Simpkins, Annellen M. (2012). Neuroscience for Clinicians: Evidence, Models, and Practice. Springer Science & Business Media. p. 143. ISBN 978-1-4614-4842-6.
- Bornstein, Marc H.; Lamb, Michael E. (2015). Developmental Science: An Advanced Textbook. Psychology Press. p. 220. ISBN 978-1-136-28220-1.
- Bernstein, Douglas (2010). Essentials of Psychology. Cengage Learning. p. 64. ISBN 978-0-495-90693-3.
- Hofman, Michel A. (March 27, 2014). "Evolution of the human brain: when bigger is better". Frontiers in Neuroanatomy. 8: 15. doi:10.3389/fnana.2014.00015. PMC 3973910. PMID 24723857.
- Gray, Peter (2002). Psychology (4th ed.). Worth Publishers. ISBN 978-0-7167-5162-5. OCLC 46640860.
- Lu, Zhong-Lin; Dosher, Barbara (2013). Visual Psychophysics: From Laboratory to Theory. MIT Press. p. 3. ISBN 978-0-262-01945-3.
- Sharwood Smith, Mike (2017). Introducing Language and Cognition. Cambridge University Press. p. 206. ISBN 978-1-107-15289-2.
- Kolb, Bryan; Whishaw, Ian Q. (2013). Introduction to Brain and Behavior. Macmillan Higher Education. p. 21. ISBN 978-1-4641-3960-4.
- Nieuwenhuys, Rudolf; ten Donkelaar, Hans J.; Nicholson, Charles (2014). The Central Nervous System of Vertebrates. Springer. p. 2127. ISBN 978-3-642-18262-4.
- Lerner, Lee; Lerner, Brenda Wilmoth (2004). The Gale Encyclopedia of Science: Pheasants-Star. Gale. p. 3759. ISBN 978-0-7876-7559-2.
As human's position changed and the manner in which the skull balanced on the spinal column pivoted, the brain expanded, altering the shape of the cranium.
- Begun, David R. (2012). A Companion to Paleoanthropology. John Wiley & Sons. p. 388. ISBN 978-1-118-33237-5.
- Jones, R. (2012). "Neurogenetics: What makes a human brain?". Nature Reviews Neuroscience. 13 (10): 655. doi:10.1038/nrn3355. PMID 22992645. S2CID 44421363.
- "Encephalo- Etymology". Online Etymology Dictionary. Archived from the original on October 2, 2017. Retrieved October 24, 2015.
- Fan, Xue; Markram, Henry (May 7, 2019). "A Brief History of Simulation Neuroscience". Frontiers in Neuroinformatics. 13: 32. doi:10.3389/fninf.2019.00032. ISSN 1662-5196. PMC 6513977. PMID 31133838.
- Parent, A.; Carpenter, M.B. (1995). "Ch. 1". Carpenter's Human Neuroanatomy. Williams & Wilkins. ISBN 978-0-683-06752-1.
- Bigos, K.L.; Hariri, A.; Weinberger, D. (2015). Neuroimaging Genetics: Principles and Practices. Oxford University Press. p. 157. ISBN 978-0-19-992022-8.
- Cosgrove, K.P.; Mazure, C.M.; Staley, J.K. (2007). "Evolving knowledge of sex differences in brain structure, function, and chemistry". Biol Psychiatry. 62 (8): 847–855. doi:10.1016/j.biopsych.2007.03.001. PMC 2711771. PMID 17544382.
- Molina, D. Kimberley; DiMaio, Vincent J.M. (2012). "Normal Organ Weights in Men". The American Journal of Forensic Medicine and Pathology. 33 (4): 368–372. doi:10.1097/PAF.0b013e31823d29ad. ISSN 0195-7910. PMID 22182984. S2CID 32174574.
- Molina, D. Kimberley; DiMaio, Vincent J. M. (2015). "Normal Organ Weights in Women". The American Journal of Forensic Medicine and Pathology. 36 (3): 182–187. doi:10.1097/PAF.0000000000000175. ISSN 0195-7910. PMID 26108038. S2CID 25319215.
- Gray's Anatomy 2008, pp. 227–9.
- Gray's Anatomy 2008, pp. 335–7.
- Ribas, G. C. (2010). "The cerebral sulci and gyri". Neurosurgical Focus. 28 (2): 7. doi:10.3171/2009.11.FOCUS09245. PMID 20121437.
- Frigeri, T.; Paglioli, E.; De Oliveira, E.; Rhoton Jr, A. L. (2015). "Microsurgical anatomy of the central lobe". Journal of Neurosurgery. 122 (3): 483–98. doi:10.3171/2014.11.JNS14315. PMID 25555079.
- Purves 2012, p. 724.
- Cipolla, M.J. (January 1, 2009). Anatomy and Ultrastructure. Morgan & Claypool Life Sciences. Archived from the original on October 1, 2017.
- "A Surgeon's-Eye View of the Brain". NPR.org. Archived from the original on November 7, 2017.
- Sampaio-Baptista, C; Johansen-Berg, H (December 20, 2017). "White Matter Plasticity in the Adult Brain". Neuron. 96 (6): 1239–1251. doi:10.1016/j.neuron.2017.11.026. PMC 5766826. PMID 29268094.
- Davey, G. (2011). Applied Psychology. John Wiley & Sons. p. 153. ISBN 978-1-4443-3121-9.
- Arsava, E. Y.; Arsava, E. M.; Oguz, K. K.; Topcuoglu, M. A. (2019). "Occipital petalia as a predictive imaging sign for transverse sinus dominance". Neurological Research. 41 (4): 306–311. doi:10.1080/01616412.2018.1560643. PMID 30601110. S2CID 58546404.
- Ackerman, S. (1992). Discovering the brain. Washington, D.C.: National Academy Press. pp. 22–25. ISBN 978-0-309-04529-2.
- Larsen 2001, pp. 455–456.
- Kandel, E.R.; Schwartz, J.H.; Jessel T.M. (2000). Principles of Neural Science. McGraw-Hill Professional. p. 324. ISBN 978-0-8385-7701-1.
- Guyton & Hall 2011, p. 574.
- Guyton & Hall 2011, p. 667.
- Principles of Anatomy and Physiology 12th Edition – Tortora, p. 519.
- Freberg, L. (2009). Discovering Biological Psychology. Cengage Learning. pp. 44–46. ISBN 978-0-547-17779-3.
- Kolb, B.; Whishaw, I. (2009). Fundamentals of Human Neuropsychology. Macmillan. pp. 73–75. ISBN 978-0-7167-9586-5.
- Pocock 2006, p. 64.
- Purves 2012, p. 399.
- Gray's Anatomy 2008, pp. 325–6.
- Goll, Y.; Atlan, G.; Citri, A. (August 2015). "Attention: the claustrum". Trends in Neurosciences. 38 (8): 486–95. doi:10.1016/j.tins.2015.05.006. PMID 26116988. S2CID 38353825.
- Goard, M.; Dan, Y. (October 4, 2009). "Basal forebrain activation enhances cortical coding of natural scenes". Nature Neuroscience. 12 (11): 1444–1449. doi:10.1038/nn.2402. PMC 3576925. PMID 19801988.
- Guyton & Hall 2011, p. 699.
- Gray's Anatomy 2008, p. 298.
- Netter, F. (2014). Atlas of Human Anatomy Including Student Consult Interactive Ancillaries and Guides (6th ed.). Philadelphia, Penn.: W B Saunders Co. p. 114. ISBN 978-1-4557-0418-7.
- Gray's Anatomy 2008, p. 297.
- Guyton & Hall 2011, pp. 698–9.
- Squire 2013, pp. 761–763.
- Gray's Anatomy 2008, p. 275.
- Guyton & Hall 2011, p. 691.
- Purves 2012, p. 377.
- Azevedo, F.; et al. (April 10, 2009). "Equal numbers of neuronal and nonneuronal cells make the human brain an isometrically scaled-up primate brain". The Journal of Comparative Neurology. 513 (5): 532–541. doi:10.1002/cne.21974. PMID 19226510. S2CID 5200449.
despite the widespread quotes that the human brain contains 100 billion neurons and ten times more glial cells, the absolute number of neurons and glial cells in the human brain remains unknown. Here we determine these numbers by using the isotropic fractionator and compare them with the expected values for a human-sized primate. We find that the adult male human brain contains on average 86.1 ± 8.1 billion NeuN-positive cells (“neurons”) and 84.6 ± 9.8 billion NeuN-negative (“nonneuronal”) cells.
- Pavel, Fiala; Jiří, Valenta (January 1, 2013). Central Nervous System. Karolinum Press. p. 79. ISBN 978-80-246-2067-1.
- Polyzoidis, S.; Koletsa, T.; Panagiotidou, S.; Ashkan, K.; Theoharides, T.C. (2015). "Mast cells in meningiomas and brain inflammation". Journal of Neuroinflammation. 12 (1): 170. doi:10.1186/s12974-015-0388-3. PMC 4573939. PMID 26377554.
- Guyton & Hall 2011, pp. 748–749.
- Budzyński, J; Kłopocka, M. (2014). "Brain-gut axis in the pathogenesis of Helicobacter pylori infection". World J. Gastroenterol. 20 (18): 5212–25. doi:10.3748/wjg.v20.i18.5212. PMC 4017036. PMID 24833851.
- Carabotti, M.; Scirocco, A.; Maselli, M.A.; Severi, C. (2015). "The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems". Ann Gastroenterol. 28 (2): 203–209. PMC 4367209. PMID 25830558.
- Sjöstedt, Evelina; Fagerberg, Linn; Hallström, Björn M.; Häggmark, Anna; Mitsios, Nicholas; Nilsson, Peter; Pontén, Fredrik; Hökfelt, Tomas; Uhlén, Mathias (June 15, 2015). "Defining the human brain proteome using transcriptomics and antibody-based profiling with a focus on the cerebral cortex". PLOS ONE. 10 (6): e0130028. Bibcode:2015PLoSO..1030028S. doi:10.1371/journal.pone.0130028. ISSN 1932-6203. PMC 4468152. PMID 26076492.
- Gray's Anatomy 2008, pp. 242–244.
- Purves 2012, p. 742.
- Gray's Anatomy 2008, p. 243.
- Iliff, JJ; Nedergaard, M (June 2013). "Is there a cerebral lymphatic system?". Stroke. 44 (6 Suppl 1): S93-5. doi:10.1161/STROKEAHA.112.678698. PMC 3699410. PMID 23709744.
- Gaillard, F. "Glymphatic pathway". radiopaedia.org. Archived from the original on October 30, 2017.
- Bacyinski A, Xu M, Wang W, Hu J (November 2017). "The Paravascular Pathway for Brain Waste Clearance: Current Understanding, Significance and Controversy". Frontiers in Neuroanatomy. 11: 101. doi:10.3389/fnana.2017.00101. PMC 5681909. PMID 29163074.
The paravascular pathway, also known as the “glymphatic” pathway, is a recently described system for waste clearance in the brain. According to this model, cerebrospinal fluid (CSF) enters the paravascular spaces surrounding penetrating arteries of the brain, mixes with interstitial fluid (ISF) and solutes in the parenchyma, and exits along paravascular spaces of draining veins. ... In addition to Aβ clearance, the glymphatic system may be involved in the removal of other interstitial solutes and metabolites. By measuring the lactate concentration in the brains and cervical lymph nodes of awake and sleeping mice, Lundgaard et al. (2017) demonstrated that lactate can exit the CNS via the paravascular pathway. Their analysis took advantage of the substantiated hypothesis that glymphatic function is promoted during sleep (Xie et al., 2013; Lee et al., 2015; Liu et al., 2017).
- Dissing-Olesen, L.; Hong, S.; Stevens, B. (August 2015). "New brain lymphatic vessels drain old concepts". EBioMedicine. 2 (8): 776–7. doi:10.1016/j.ebiom.2015.08.019. PMC 4563157. PMID 26425672.
- Sun, BL; Wang, LH; Yang, T; Sun, JY; Mao, LL; Yang, MF; Yuan, H; Colvin, RA; Yang, XY (April 2018). "Lymphatic drainage system of the brain: A novel target for intervention of neurological diseases". Progress in Neurobiology. 163–164: 118–143. doi:10.1016/j.pneurobio.2017.08.007. PMID 28903061. S2CID 6290040.
- Gray's Anatomy 2008, p. 247.
- Gray's Anatomy 2008, pp. 251–2.
- Gray's Anatomy 2008, p. 250.
- Gray's Anatomy 2008, p. 248.
- Gray's Anatomy 2008, p. 251.
- Gray's Anatomy 2008, pp. 254–6.
- Elsevier's 2007, pp. 311–4.
- Daneman, R.; Zhou, L.; Kebede, A.A.; Barres, B.A. (November 25, 2010). "Pericytes are required for blood-brain barrier integrity during embryogenesis". Nature. 468 (7323): 562–6. Bibcode:2010Natur.468..562D. doi:10.1038/nature09513. PMC 3241506. PMID 20944625.
- Laterra, J.; Keep, R.; Betz, L.A.; et al. (1999). "Blood–cerebrospinal fluid barrier". Basic neurochemistry: molecular, cellular and medical aspects (6th ed.). Philadelphia: Lippincott-Raven.
- Sadler, T. (2010). Langman's medical embryology (11th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 293. ISBN 978-0-7817-9069-7.
- Larsen 2001, p. 419.
- Larsen 2001, pp. 85–88.
- Purves 2012, pp. 480–482.
- Larsen 2001, pp. 445–446.
- "OpenStax CNX". cnx.org. Archived from the original on May 5, 2015. Retrieved May 5, 2015.
- Larsen 2001, pp. 85–87.
- Purves 2012, pp. 481–484.
- Purves, Dale; Augustine, George J; Fitzpatrick, David; Katz, Lawrence C; LaMantia, Anthony-Samuel; McNamara, James O; Williams, S Mark, eds. (2001). "Rhombomeres". Neuroscience (2nd ed.). ISBN 978-0-87893-742-4.
- Chen, X. (2012). Mechanical Self-Assembly: Science and Applications. Springer Science & Business Media. pp. 188–189. ISBN 978-1-4614-4562-3.
- Ronan, L; Voets, N; Rua, C; Alexander-Bloch, A; Hough, M; Mackay, C; Crow, TJ; James, A; Giedd, JN; Fletcher, PC (August 2014). "Differential tangential expansion as a mechanism for cortical gyrification". Cerebral Cortex. 24 (8): 2219–28. doi:10.1093/cercor/bht082. PMC 4089386. PMID 23542881.
- Van Essen, DC (January 23, 1997). "A tension-based theory of morphogenesis and compact wiring in the central nervous system". Nature. 385 (6614): 313–8. Bibcode:1997Natur.385..313E. doi:10.1038/385313a0. PMID 9002514. S2CID 4355025.
- Borrell, V (January 24, 2018). "How Cells Fold the Cerebral Cortex". The Journal of Neuroscience. 38 (4): 776–783. doi:10.1523/JNEUROSCI.1106-17.2017. PMC 6596235. PMID 29367288.
- Florio, M.; et al. (March 27, 2015). "Human-specific gene ARHGAP11B promotes basal progenitor amplification and neocortex expansion". Science. 347 (6229): 1465–70. Bibcode:2015Sci...347.1465F. doi:10.1126/science.aaa1975. PMID 25721503. S2CID 34506325.
- "Parts of the Brain | Introduction to Psychology". courses.lumenlearning.com. Retrieved September 20, 2019.
- Guyton & Hall 2011, p. 685.
- Guyton & Hall 2011, p. 687.
- Guyton & Hall 2011, p. 686.
- Guyton & Hall 2011, pp. 698, 708.
- Davidson's 2010, p. 1139.
- Hellier, J. (2014). The Brain, the Nervous System, and Their Diseases [3 volumes]. ABC-CLIO. pp. 300–303. ISBN 978-1-61069-338-7.
- Guyton & Hall 2011, pp. 571–576.
- Guyton & Hall 2011, pp. 573–574.
- Guyton & Hall 2011, pp. 623–631.
- Guyton & Hall 2011, pp. 739–740.
- Pocock 2006, pp. 138–139.
- Squire 2013, pp. 525–526.
- Guyton & Hall 2011, pp. 647–648.
- Guyton & Hall 2011, pp. 202–203.
- Guyton & Hall 2011, pp. 205–208.
- Guyton & Hall 2011, pp. 505–509.
- "Brain Basics: Understanding Sleep | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Archived from the original on December 22, 2017.
- Guyton & Hall 2011, p. 723.
- Davis, J.F.; Choi, D.L.; Benoit, S.C. (2011). "24. Orexigenic Hypothalamic Peptides Behavior and Feeding – 24.5 Orexin". In Preedy, V.R.; Watson, R.R.; Martin, C.R. (eds.). Handbook of Behavior, Food and Nutrition. Springer. pp. 361–362. ISBN 978-0-387-92271-3.
- Squire 2013, p. 800.
- Squire 2013, p. 803.
- Squire 2013, p. 805.
- Guyton & Hall 2011, pp. 720–2.
- Poeppel, D.; Emmorey, K.; Hickok, G.; Pylkkänen, L. (October 10, 2012). "Towards a new neurobiology of language". The Journal of Neuroscience. 32 (41): 14125–14131. doi:10.1523/JNEUROSCI.3244-12.2012. PMC 3495005. PMID 23055482.
- Hickok, G (September 2009). "The functional neuroanatomy of language". Physics of Life Reviews. 6 (3): 121–143. Bibcode:2009PhLRv...6..121H. doi:10.1016/j.plrev.2009.06.001. PMC 2747108. PMID 20161054.
- Fedorenko, E.; Kanwisher, N. (2009). "Neuroimaging of language: why hasn't a clearer picture emerged?". Language and Linguistics Compass. 3 (4): 839–865. doi:10.1111/j.1749-818x.2009.00143.x. S2CID 2833893.
- Damasio, H. (2001). "Neural basis of language disorders". In Chapey, Roberta (ed.). Language intervention strategies in aphasia and related neurogenic communication disorders (4th ed.). Lippincott Williams & Wilkins. pp. 18–36. ISBN 978-0-7817-2133-2. OCLC 45952164.
- Berntson, G.; Cacioppo, J. (2009). Handbook of Neuroscience for the Behavioral Sciences, Volume 1. John Wiley & Sons. p. 145. ISBN 978-0-470-08355-0.
- Hellier, J. (2014). The Brain, the Nervous System, and Their Diseases [3 volumes]. ABC-CLIO. p. 1135. ISBN 978-1-61069-338-7.
- Kolb, B.; Whishaw, I.Q. (2013). Introduction to Brain and Behavior. Macmillan Higher Education. p. 296. ISBN 978-1-4641-3960-4.
- Sherwood, L. (2012). Human Physiology: From Cells to Systems. Cengage Learning. p. 181. ISBN 978-1-133-70853-7.
- Kalat, J (2015). Biological Psychology. Cengage Learning. p. 425. ISBN 978-1-305-46529-9.
- Cowin, S.C.; Doty, S.B. (2007). Tissue Mechanics. Springer Science & Business Media. p. 4. ISBN 978-0-387-49985-7.
- Morris, C.G.; Maisto, A.A. (2011). Understanding Psychology. Prentice Hall. p. 56. ISBN 978-0-205-76906-3.
- Kolb, B.; Whishaw, I.Q. (2013). Introduction to Brain and Behavior (Loose-Leaf). Macmillan Higher Education. pp. 524–549. ISBN 978-1-4641-3960-4.
- Schacter, D.L.; Gilbert, D.T.; Wegner, D.M. (2009). Introducing Psychology. Macmillan. p. 80. ISBN 978-1-4292-1821-4.
- Sander, David (2013). Armony, J.; Vuilleumier, Patrik (eds.). The Cambridge handbook of human affective neuroscience. Cambridge: Cambridge Univ. Press. p. 16. ISBN 978-0-521-17155-7.
- Lindquist, KA.; Wager, TD.; Kober, H; Bliss-Moreau, E; Barrett, LF (May 23, 2012). "The brain basis of emotion: A meta-analytic review". Behavioral and Brain Sciences. 35 (3): 121–143. doi:10.1017/S0140525X11000446. PMC 4329228. PMID 22617651.
- Phan, KL; Wager, Tor; Taylor, SF.; Liberzon, l (June 1, 2002). "Functional Neuroanatomy of Emotion: A Meta-Analysis of Emotion Activation Studies in PET and fMRI". NeuroImage. 16 (2): 331–348. doi:10.1006/nimg.2002.1087. PMID 12030820. S2CID 7150871.
- Malenka, RC; Nestler, EJ; Hyman, SE (2009). "Preface". In Sydor, A; Brown, RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. xiii. ISBN 978-0-07-148127-4.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 14: Higher Cognitive Function and Behavioral Control". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 6: Widely Projecting Systems: Monoamines, Acetylcholine, and Orexin". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
- Diamond, A (2013). "Executive functions". Annual Review of Psychology. 64: 135–168. doi:10.1146/annurev-psych-113011-143750. PMC 4084861. PMID 23020641.
Figure 4: Executive functions and related terms Archived May 9, 2018, at the Wayback Machine - Hyun, J.C.; Weyandt, L.L.; Swentosky, A. (2014). "Chapter 2: The Physiology of Executive Functioning". In Goldstein, S.; Naglieri, J. (eds.). Handbook of Executive Functioning. New York: Springer. pp. 13–23. ISBN 978-1-4614-8106-5.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 14: Higher Cognitive Function and Behavioral Control". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
In conditions in which prepotent responses tend to dominate behavior, such as in drug addiction, where drug cues can elicit drug seeking (Chapter 16), or in attention deficit hyperactivity disorder (ADHD; described below), significant negative consequences can result. ... ADHD can be conceptualized as a disorder of executive function; specifically, ADHD is characterized by reduced ability to exert and maintain cognitive control of behavior. Compared with healthy individuals, those with ADHD have diminished ability to suppress inappropriate prepotent responses to stimuli (impaired response inhibition) and diminished ability to inhibit responses to irrelevant stimuli (impaired interference suppression). ... Functional neuroimaging in humans demonstrates activation of the prefrontal cortex and caudate nucleus (part of the dorsal striatum) in tasks that demand inhibitory control of behavior. ... Early results with structural MRI show a thinner cerebral cortex, across much of the cerebrum, in ADHD subjects compared with age-matched controls, including areas of [the] prefrontal cortex involved in working memory and attention.
- Pocock 2006, p. 68.
- Clark, B.D.; Goldberg, E.M.; Rudy, B. (December 2009). "Electrogenic tuning of the axon initial segment". The Neuroscientist. 15 (6): 651–68. doi:10.1177/1073858409341973. PMC 2951114. PMID 20007821.
- Pocock 2006, pp. 70–74.
- "NIMH » Brain Basics". www.nimh.nih.gov. Archived from the original on March 26, 2017. Retrieved March 26, 2017.
- Purves, Dale (2011). Neuroscience (5. ed.). Sunderland, Mass.: Sinauer. p. 139. ISBN 978-0-87893-695-3.
- Swaminathan, N (April 29, 2008). "Why Does the Brain Need So Much Power?". Scientific American. Archived from the original on January 27, 2014. Retrieved November 19, 2010.
- Wasserman DH (January 2009). "Four grams of glucose". American Journal of Physiology. Endocrinology and Metabolism. 296 (1): E11–21. doi:10.1152/ajpendo.90563.2008. PMC 2636990. PMID 18840763.
Four grams of glucose circulates in the blood of a person weighing 70 kg. This glucose is critical for normal function in many cell types. In accordance with the importance of these 4 g of glucose, a sophisticated control system is in place to maintain blood glucose constant. Our focus has been on the mechanisms by which the flux of glucose from liver to blood and from blood to skeletal muscle is regulated. ... The brain consumes ∼60% of the blood glucose used in the sedentary, fasted person. ... The amount of glucose in the blood is preserved at the expense of glycogen reservoirs (Fig. 2). In postabsorptive humans, there are ∼100 g of glycogen in the liver and ∼400 g of glycogen in muscle. Carbohydrate oxidation by the working muscle can go up by ∼10-fold with exercise, and yet after 1 h, blood glucose is maintained at ∼4 g. ... It is now well established that both insulin and exercise cause translocation of GLUT4 to the plasma membrane. Except for the fundamental process of GLUT4 translocation, [muscle glucose uptake (MGU)] is controlled differently with exercise and insulin. Contraction-stimulated intracellular signaling (52, 80) and MGU (34, 75, 77, 88, 91, 98) are insulin independent. Moreover, the fate of glucose extracted from the blood is different in response to exercise and insulin (91, 105). For these reasons, barriers to glucose flux from blood to muscle must be defined independently for these two controllers of MGU.
- Quistorff, B; Secher, N; Van Lieshout, J (July 24, 2008). "Lactate fuels the human brain during exercise". The FASEB Journal. 22 (10): 3443–3449. doi:10.1096/fj.08-106104. PMID 18653766. S2CID 15394163.
- Obel, L.F.; Müller, M.S.; Walls, A.B.; Sickmann, H.M.; Bak, L.K.; Waagepetersen, H.S.; Schousboe, A. (2012). "Brain glycogen-new perspectives on its metabolic function and regulation at the subcellular level". Frontiers in Neuroenergetics. 4: 3. doi:10.3389/fnene.2012.00003. PMC 3291878. PMID 22403540.
- Marin-Valencia, I.; et al. (February 2013). "Heptanoate as a neural fuel: energetic and neurotransmitter precursors in normal and glucose transporter I-deficient (G1D) brain". Journal of Cerebral Blood Flow and Metabolism. 33 (2): 175–82. doi:10.1038/jcbfm.2012.151. PMC 3564188. PMID 23072752.
- Tsuji, A. (2005). "Small molecular drug transfer across the blood-brain barrier via carrier-mediated transport systems". NeuroRx. 2 (1): 54–62. doi:10.1602/neurorx.2.1.54. PMC 539320. PMID 15717057.
Uptake of valproic acid was reduced in the presence of medium-chain fatty acids such as hexanoate, octanoate, and decanoate, but not propionate or butyrate, indicating that valproic acid is taken up into the brain via a transport system for medium-chain fatty acids, not short-chain fatty acids. ... Based on these reports, valproic acid is thought to be transported bidirectionally between blood and brain across the BBB via two distinct mechanisms, monocarboxylic acid-sensitive and medium-chain fatty acid-sensitive transporters, for efflux and uptake, respectively.
- Vijay, N.; Morris, M.E. (2014). "Role of monocarboxylate transporters in drug delivery to the brain". Curr. Pharm. Des. 20 (10): 1487–98. doi:10.2174/13816128113199990462. PMC 4084603. PMID 23789956.
Monocarboxylate transporters (MCTs) are known to mediate the transport of short chain monocarboxylates such as lactate, pyruvate and butyrate. ... MCT1 and MCT4 have also been associated with the transport of short chain fatty acids such as acetate and formate which are then metabolized in the astrocytes [78].
- Clark, D.D.; Sokoloff. L. (1999). Siegel, G.J.; Agranoff, B.W.; Albers, R.W.; Fisher, S.K.; Uhler, M.D. (eds.). Basic Neurochemistry: Molecular, Cellular and Medical Aspects. Philadelphia: Lippincott. pp. 637–670. ISBN 978-0-397-51820-3.
- Mrsulja, B.B. (2012). Pathophysiology of Cerebral Energy Metabolism. Springer Science & Business Media. pp. 2–3. ISBN 978-1-4684-3348-7.
- Raichle, M.; Gusnard, DA (2002). "Appraising the brain's energy budget". Proc. Natl. Acad. Sci. U.S.A. 99 (16): 10237–10239. Bibcode:2002PNAS...9910237R. doi:10.1073/pnas.172399499. PMC 124895. PMID 12149485.
- Gianaros, Peter J.; Gray, Marcus A.; Onyewuenyi, Ikechukwu; Critchley, Hugo D. (2010). "Chapter 50. Neuroimaging methods in behavioral medicine". In Steptoe, A. (ed.). Handbook of Behavioral Medicine: Methods and Applications. Springer Science & Business Media. p. 770. doi:10.1007/978-0-387-09488-5_50. ISBN 978-0-387-09488-5.
- Kuzawa, C. W.; Chugani, H. T.; Grossman, L. I.; Lipovich, L.; Muzik, O.; Hof, P. R.; Wildman, D. E.; Sherwood, C. C.; Leonard, W. R.; Lange, N. (September 9, 2014). "Metabolic costs and evolutionary implications of human brain development". Proceedings of the National Academy of Sciences. 111 (36): 13010–13015. Bibcode:2014PNAS..11113010K. doi:10.1073/pnas.1323099111. ISSN 0027-8424. PMC 4246958. PMID 25157149.
- "Brain may flush out toxins during sleep". National Institutes of Health. Archived from the original on October 20, 2013. Retrieved October 25, 2013.
- Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O'Donnell J, Christensen DJ, Nicholson C, Iliff JJ, Takano T, Deane R, Nedergaard M (October 2013). "Sleep drives metabolite clearance from the adult brain". Science. 342 (6156): 373–377. Bibcode:2013Sci...342..373X. doi:10.1126/science.1241224. PMC 3880190. PMID 24136970.
Thus, the restorative function of sleep may be a consequence of the enhanced removal of potentially neurotoxic waste products that accumulate in the awake central nervous system.
- Tononi, Guilio; Cirelli, Chiara (August 2013). "Perchance to Prune" (PDF). Scientific American. 309 (2): 34–39. Bibcode:2013SciAm.309b..34T. doi:10.1038/scientificamerican0813-34. PMID 23923204. S2CID 54052089. Archived from the original (PDF) on December 26, 2018.
- Van Essen, D.C.; et al. (October 2012). "The Human Connectome Project: A data acquisition perspective". NeuroImage. 62 (4): 2222–2231. doi:10.1016/j.neuroimage.2012.02.018. PMC 3606888. PMID 22366334.
- Jones, E.G.; Mendell, L.M. (April 30, 1999). "Assessing the Decade of the Brain". Science. 284 (5415): 739. Bibcode:1999Sci...284..739J. doi:10.1126/science.284.5415.739. PMID 10336393. S2CID 13261978.
- "A $4.5 Billion Price Tag for the BRAIN Initiative?". Science | AAAS. June 5, 2014. Archived from the original on June 18, 2017.
- Towle, V.L.; et al. (January 1993). "The spatial location of EEG electrodes: locating the best-fitting sphere relative to cortical anatomy". Electroencephalography and Clinical Neurophysiology. 86 (1): 1–6. doi:10.1016/0013-4694(93)90061-y. PMID 7678386.
- Purves 2012, pp. 632–633.
- Silverstein, J. (2012). "Mapping the Motor and Sensory Cortices: A Historical Look and a Current Case Study in Sensorimotor Localization and Direct Cortical Motor Stimulation". The Neurodiagnostic Journal. 52 (1): 54–68. PMID 22558647. Archived from the original on November 17, 2012.
- Boraud, T.; Bezard, E.; et al. (2002). "From single extracellular unit recording in experimental and human Parkinsonism to the development of a functional concept of the role played by the basal ganglia in motor control". Progress in Neurobiology. 66 (4): 265–283. doi:10.1016/s0301-0082(01)00033-8. PMID 11960681. S2CID 23389986.
- Lancaster, MA; Renner, M; Martin, CA; Wenzel, D; Bicknell, LS; Hurles, ME; Homfray, T; Penninger, JM; Jackson, AP; Knoblich, JA (September 19, 2013). "Cerebral organoids model human brain development and microcephaly". Nature. 501 (7467): 373–9. Bibcode:2013Natur.501..373L. doi:10.1038/nature12517. PMC 3817409. PMID 23995685.
- Lee, CT; Bendriem, RM; Wu, WW; Shen, RF (August 20, 2017). "3D brain Organoids derived from pluripotent stem cells: promising experimental models for brain development and neurodegenerative disorders". Journal of Biomedical Science. 24 (1): 59. doi:10.1186/s12929-017-0362-8. PMC 5563385. PMID 28822354.
- "Magnetic Resonance, a critical peer-reviewed introduction; functional MRI". European Magnetic Resonance Forum. Archived from the original on June 2, 2017. Retrieved June 30, 2017.
- Buxton, R.; Uludag, K.; Liu, T. (2004). "Modeling the haemodynamic response to brain activation". NeuroImage. 23: S220–S233. CiteSeerX 10.1.1.329.29. doi:10.1016/j.neuroimage.2004.07.013. PMID 15501093. S2CID 8736954.
- Biswal, B.B. (August 15, 2012). "Resting state fMRI: a personal history". NeuroImage. 62 (2): 938–44. doi:10.1016/j.neuroimage.2012.01.090. PMID 22326802. S2CID 93823.
- Purves 2012, p. 20.
- Kane, R.L.; Parsons, T.D. (2017). The Role of Technology in Clinical Neuropsychology. Oxford University Press. p. 399. ISBN 978-0-19-023473-7.
Irimia, Chambers, Torgerson, and Van Horn (2012) provide a first-step graphic on how best to display connectivity findings, as is presented in Figure 13.15. This is referred to as a connectogram.
- Andrews, D.G. (2001). Neuropsychology. Psychology Press. ISBN 978-1-84169-103-9.
- Lepage, M. (2010). "Research at the Brain Imaging Centre". Douglas Mental Health University Institute. Archived from the original on March 5, 2012.
- Steward, C.A.; et al. (2017). "Genome annotation for clinical genomic diagnostics: strengths and weaknesses". Genome Med. 9 (1): 49. doi:10.1186/s13073-017-0441-1. PMC 5448149. PMID 28558813.
- Harrow, J.; et al. (September 2012). "GENCODE: the reference human genome annotation for The ENCODE Project". Genome Res. 22 (9): 1760–74. doi:10.1101/gr.135350.111. PMC 3431492. PMID 22955987.
- Gibson G, Muse SV (April 20, 2009). A primer of genome science (3rd ed.). Sunderland, MA: Sinauer Associates. ISBN 9780878932368.
- "The human proteome in brain – The Human Protein Atlas". www.proteinatlas.org. Archived from the original on September 29, 2017. Retrieved September 29, 2017.
- Uhlén, Mathias; Fagerberg, Linn; Hallström, Björn M.; Lindskog, Cecilia; Oksvold, Per; Mardinoglu, Adil; Sivertsson, Åsa; Kampf, Caroline; Sjöstedt, Evelina (January 23, 2015). "Tissue-based map of the human proteome". Science. 347 (6220): 1260419. doi:10.1126/science.1260419. ISSN 0036-8075. PMID 25613900. S2CID 802377.
- Warden, A (2017). "Gene expression profiling in the human alcoholic brain". Neuropharmacology. 122: 161–174. doi:10.1016/j.neuropharm.2017.02.017. PMC 5479716. PMID 28254370.
- Farris, S.P.; et al. (2015). "Applying the new genomics to alcohol dependence". Alcohol. 49 (8): 825–36. doi:10.1016/j.alcohol.2015.03.001. PMC 4586299. PMID 25896098.
- Rozycka, A; Liguz-Lecznar, M (August 2017). "The space where aging acts: focus on the GABAergic synapse". Aging Cell. 16 (4): 634–643. doi:10.1111/acel.12605. PMC 5506442. PMID 28497576.
- Flores, CE; Méndez, P (2014). "Shaping inhibition: activity dependent structural plasticity of GABAergic synapses". Frontiers in Cellular Neuroscience. 8: 327. doi:10.3389/fncel.2014.00327. PMC 4209871. PMID 25386117.
- "Brain Injury, Traumatic". Medcyclopaedia. GE. Archived from the original on May 26, 2011.
- Dawodu, S.T. (March 9, 2017). "Traumatic Brain Injury (TBI) – Definition and Pathophysiology: Overview, Epidemiology, Primary Injury". Medscape. Archived from the original on April 9, 2017.
- Davidson's 2010, pp. 1196–7.
- Davidson's 2010, pp. 1205–15.
- Davidson's 2010, pp. 1216–7.
- Volkow, N.D.; Koob, G.F.; McLellan, A.T. (January 2016). "Neurobiologic advances from the brain disease model of addiction". The New England Journal of Medicine. 374 (4): 363–371. doi:10.1056/NEJMra1511480. PMC 6135257. PMID 26816013.
- Simpson, J.M.; Moriarty, G.L. (2013). Multimodal Treatment of Acute Psychiatric Illness: A Guide for Hospital Diversion. Columbia University Press. pp. 22–24. ISBN 978-0-231-53609-7.
- Davidson's 2010, pp. 1172–9.
- "Status Epilepticus". Epilepsy Foundation.
- Moore, S.P. (2005). The Definitive Neurological Surgery Board Review. Lippincott Williams & Wilkins. p. 112. ISBN 978-1-4051-0459-3.
- Pennington, B.F. (2008). Diagnosing Learning Disorders, Second Edition: A Neuropsychological Framework. Guilford Press. pp. 3–10. ISBN 978-1-60623-786-1.
- Govaert, P.; de Vries, L.S. (2010). An Atlas of Neonatal Brain Sonography: (CDM 182–183). John Wiley & Sons. pp. 89–92. ISBN 978-1-898683-56-8.
- Perese, E.F. (2012). Psychiatric Advanced Practice Nursing: A Biopsychsocial Foundation for Practice. F.A. Davis. pp. 82–88. ISBN 978-0-8036-2999-8.
- Kearney, C.; Trull, T.J. (2016). Abnormal Psychology and Life: A Dimensional Approach. Cengage Learning. p. 395. ISBN 978-1-337-09810-6.
- Stevenson, D.K.; Sunshine, P.; Benitz, W.E. (2003). Fetal and Neonatal Brain Injury: Mechanisms, Management and the Risks of Practice. Cambridge University Press. p. 191. ISBN 978-0-521-80691-6.
- Dewhurst, John (2012). Dewhurst's Textbook of Obstetrics and Gynaecology. John Wiley & Sons. p. 43. ISBN 978-0-470-65457-6.
- Harbison, J.; Massey, A.; Barnett, L.; Hodge, D.; Ford, G.A. (June 1999). "Rapid ambulance protocol for acute stroke". Lancet. 353 (9168): 1935. doi:10.1016/S0140-6736(99)00966-6. PMID 10371574. S2CID 36692451.
- Davidson's 2010, p. 1183.
- Davidson's 2010, pp. 1180–1.
- Davidson's 2010, pp. 1181, 1183–1185.
- Davidson's 2010, pp. 1183–1185.
- Davidson's 2010, pp. 1185–1189.
- Goyal, M.; et al. (April 2016). "Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials". The Lancet. 387 (10029): 1723–1731. doi:10.1016/S0140-6736(16)00163-X. PMID 26898852. S2CID 34799180.
- Saver, J. L. (December 8, 2005). "Time is brain—quantified". Stroke. 37 (1): 263–266. doi:10.1161/01.STR.0000196957.55928.ab. PMID 16339467.
- Winstein, C.J.; et al. (June 2016). "Guidelines for adult stroke rehabilitation and recovery". Stroke. 47 (6): e98–e169. doi:10.1161/STR.0000000000000098. PMID 27145936. S2CID 4967333.
- Kuźma, Elżbieta; Lourida, Ilianna; Moore, Sarah F.; Levine, Deborah A.; Ukoumunne, Obioha C.; Llewellyn, David J. (November 2018). "Stroke and dementia risk: A systematic review and meta-analysis". Alzheimer's & Dementia. 14 (11): 1416–1426. doi:10.1016/j.jalz.2018.06.3061. ISSN 1552-5260. PMC 6231970. PMID 30177276.
- Goila, AK; Pawar, M (2009). "The diagnosis of brain death". Indian Journal of Critical Care Medicine. 13 (1): 7–11. doi:10.4103/0972-5229.53108. PMC 2772257. PMID 19881172.
- Wijdicks, EFM (January 8, 2002). "Brain death worldwide: accepted fact but no global consensus in diagnostic criteria". Neurology. 58 (1): 20–25. doi:10.1212/wnl.58.1.20. PMID 11781400. S2CID 219203458.
- Dhanwate, AD (September 2014). "Brainstem death: A comprehensive review in Indian perspective". Indian Journal of Critical Care Medicine. 18 (9): 596–605. doi:10.4103/0972-5229.140151. PMC 4166875. PMID 25249744.
- Davidson's 2010, p. 1158.
- Davidson's 2010, p. 200.
- Urden, L.D.; Stacy, K.M.; Lough, M.E. (2013). Priorities in Critical Care Nursing – E-Book. Elsevier Health Sciences. pp. 112–113. ISBN 978-0-323-29414-0.
- Domínguez, J.F.; Lewis, E.D.; Turner, R.; Egan, G.F. (2009). Chiao, J.Y. (ed.). The Brain in Culture and Culture in the Brain: A Review of Core Issues in Neuroanthropology. Progress in Brain Research. Special issue: Cultural Neuroscience: Cultural Influences on Brain Function. Vol. 178. pp. 43–6. doi:10.1016/S0079-6123(09)17804-4. ISBN 978-0-444-53361-6. PMID 19874961.
- "Cultural Environment Influences Brain Function | Psych Central News". Psych Central News. August 4, 2010. Archived from the original on January 17, 2017.
- Macmillan, Malcolm B. (2000). An Odd Kind of Fame: Stories of Phineas Gage. MIT Press. ISBN 978-0-262-13363-0.
- Rescher, N. (1992). G. W. Leibniz's Monadology. Psychology Press. p. 83. ISBN 978-0-415-07284-7.
- Hart, WD (1996). Guttenplan S (ed.). A Companion to the Philosophy of Mind. Blackwell. pp. 265–267.
- Churchland, P.S. (1989). "Ch. 8". Neurophilosophy. MIT Press. ISBN 978-0-262-53085-9.
- Selimbeyoglu, Aslihan; Parvizi, J (2010). "Electrical stimulation of the human brain: perceptual and behavioral phenomena reported in the old and new literature". Frontiers in Human Neuroscience. 4: 46. doi:10.3389/fnhum.2010.00046. PMC 2889679. PMID 20577584.
- Schwartz, J.H. Appendix D: Consciousness and the Neurobiology of the Twenty-First Century. In Kandel, E.R.; Schwartz, J.H.; Jessell, T.M. (2000). Principles of Neural Science, 4th Edition.
- Lilienfeld, S.O.; Lynn, S.J.; Ruscio, J.; Beyerstein, B.L. (2011). 50 Great Myths of Popular Psychology: Shattering Widespread Misconceptions about Human Behavior. John Wiley & Sons. p. 89. ISBN 978-1-4443-6074-5.
- McDaniel, M. (2005). "Big-brained people are smarter" (PDF). Intelligence. 33 (4): 337–346. doi:10.1016/j.intell.2004.11.005. Archived (PDF) from the original on September 6, 2014.
- Luders, E.; et al. (September 2008). "Mapping the relationship between cortical convolution and intelligence: effects of gender". Cerebral Cortex. 18 (9): 2019–26. doi:10.1093/cercor/bhm227. PMC 2517107. PMID 18089578.
- Hoppe, C; Stojanovic, J (2008). "High-Aptitude Minds". Scientific American Mind. 19 (4): 60–67. doi:10.1038/scientificamericanmind0808-60.
- "Tupaia belangeri". The Genome Institute, Washington University. Archived from the original on June 1, 2010. Retrieved January 22, 2016.
- Carrier, Martin; Mittelstrass, Jürgen (1991). Mind, Brain, Behavior: The Mind-body Problem and the Philosophy of Psychology [Geist, Gehirn, Verhalten]. Translated by Lindberg, Steven (revised and expanded English ed.). Berlin: Walter de Gruyter. p. 11. ISBN 9783110128765. Retrieved May 22, 2021.
[...] the Aristotelian view that the soul resides primarily in the heart [...].
- Cobb, Matthew (April 21, 2020). The Idea of the Brain: The Past and Future of Neuroscience. New York: Hachette UK (published 2020). ISBN 9781541646865. Retrieved May 22, 2021.
[...] the ways in which we think about [the brain] are much richer than in the past, not simply because of the amazing facts we have discovered, but above all because of how we interpret them.
- Jarrett, C. (November 17, 2014). Great Myths of the Brain. John Wiley & Sons. ISBN 978-1-118-31271-1.
- Phillips, Helen (July 11, 2002). "Video game "brain damage" claim criticised". New Scientist. Archived from the original on January 11, 2009. Retrieved February 6, 2008.
- Popova, Maria (August 18, 2011). "'Brain Culture': How Neuroscience Became a Pop Culture Fixation". The Atlantic. Archived from the original on July 28, 2017.
- Thornton, Davi Johnson (2011). Brain Culture. Neuroscience and Popular Media. Rutgers University Press. ISBN 978-0-8135-5013-8.
- Cyborgs and Space Archived October 6, 2011, at the Wayback Machine, in Astronautics (September 1960), by Manfred E. Clynes and Nathan S. Kline.
- Bergfelder, Tim (2005). International Adventures: German Popular Cinema and European Co-productions in the 1960s. Berghahn Books. p. 129. ISBN 978-1-57181-538-5.
- Kandel, ER; Schwartz JH; Jessell TM (2000). Principles of Neural Science (4th ed.). New York: McGraw-Hill. ISBN 978-0-8385-7701-1.
- Gross, Charles G. (1987). Adelman, George (ed.). Encyclopedia of neuroscience (PDF) (2. ed.). Boston: Birkhäeuser. pp. 843–847. ISBN 978-0-8176-3335-6. Archived (PDF) from the original on May 5, 2013.
- Bear, M.F.; B.W. Connors; M.A. Paradiso (2001). Neuroscience: Exploring the Brain. Baltimore: Lippincott. ISBN 978-0-7817-3944-3.
- von Staden, p.157
- Swanson, Larry W. (August 12, 2014). Neuroanatomical Terminology: A Lexicon of Classical Origins and Historical Foundations. Oxford University Press. ISBN 978-0-19-534062-4.
- Lokhorst, Gert-Jan (January 1, 2016). "Descartes and the Pineal Gland". The Stanford Encyclopedia of Philosophy. Metaphysics Research Lab, Stanford University. Retrieved March 11, 2017.
- Gross, Charles G. (1999). Brain, vision, memory : tales in the history of neuroscience (1st MIT Press pbk. ed.). Cambridge, Mass.: MIT. pp. 37–51. ISBN 978-0-262-57135-7.
- Marshall, Louise H.; Magoun, Horace W. (March 9, 2013). Discoveries in the Human Brain: Neuroscience Prehistory, Brain Structure, and Function. Springer Science & Business Media. p. 44. ISBN 978-1-475-74997-7.
- Holtz, Anders; Levi, Richard (July 20, 2010). Spinal Cord Injury. Oxford University Press. ISBN 978-0-19-970681-5.
- Tessman, Patrick A.; Suarez, Jose I. (2002). "Influence of early printmaking on the development of neuroanatomy and neurology". Archives of Neurology. 59 (12): 1964–1969. doi:10.1001/archneur.59.12.1964. PMID 12470188.
- O'Connor, James (2003). "Thomas Willis and the background to Cerebri Anatome". Journal of the Royal Society of Medicine. 96 (3): 139–143. doi:10.1177/014107680309600311. PMC 539424. PMID 12612118.
- EMERY, ALAN (October 2000). "A Short History of Neurology: The British Contribution 1660–1910. Edited by F. CLIFFORD ROSE. (Pp. 282; illustrated; £25 Paperback; ISBN 07506 4165 7.) Oxford: Butterworth-Heinemann". Journal of Anatomy. 197 (3): 513–518. doi:10.1046/j.1469-7580.2000.197305131.x. PMC 1468164.
- Olesko, Kathryn M.; Holmes, Frederic L. (1994). Cahan, David (ed.). "Experiment, Quantification, and Discovery: Helmholtz's Early Physiological Researches, 1843-50". Hermann von Helmholtz and the Foundations of Nineteenth Century Science. Berkeley; Los Angeles; London: University of California Press: 50–108.
- Sabbatini, Renato M.E. "Sabbatini, R.M.E.: The Discovery of Bioelectricity. Nerve Conduction". www.cerebromente.org.br. Archived from the original on June 26, 2017. Retrieved June 10, 2017.
- Finkelstein, Gabriel Ward (2013). Emil du Bois-Reymond : neuroscience, self, and society in nineteenth-century Germany. Cambridge, Massachusetts. ISBN 978-1-4619-5032-5. OCLC 864592470.
- Karbowski, Kazimierz (February 14, 2008). "Sixty Years of Clinical Electroencephalography". European Neurology. 30 (3): 170–175. doi:10.1159/000117338. PMID 2192889.
- Pearce, J.M.S. (March 17, 2009). "Marie-Jean-Pierre Flourens (1794–1867) and Cortical Localization". European Neurology. 61 (5): 311–314. doi:10.1159/000206858. PMID 19295220.
- De Carlos, Juan A.; Borrell, José (August 2007). "A historical reflection of the contributions of Cajal and Golgi to the foundations of neuroscience". Brain Research Reviews. 55 (1): 8–16. doi:10.1016/j.brainresrev.2007.03.010. hdl:10261/62299. PMID 17490748. S2CID 7266966.
- Burke, R.E. (April 2007). "Sir Charles Sherrington's The integrative action of the nervous system: a centenary appreciation". Brain. 130 (Pt 4): 887–894. doi:10.1093/brain/awm022. PMID 17438014.
- Squire, Larry R., ed. (1996). The history of neuroscience in autobiography. Washington DC: Society for Neuroscience. pp. 475–97. ISBN 978-0-12-660305-7.
- Cowan, W.M.; Harter, D.H.; Kandel, E.R. (2000). "The emergence of modern neuroscience: Some implications for neurology and psychiatry". Annual Review of Neuroscience. 23: 345–346. doi:10.1146/annurev.neuro.23.1.343. PMID 10845068.
- Brady, Joseph V.; Nauta, Walle J. H. (October 22, 2013). Principles, Practices, and Positions in Neuropsychiatric Research: Proceedings of a Conference Held in June 1970 at the Walter Reed Army Institute of Research, Washington, D.C., in Tribute to Dr. David Mckenzie Rioch upon His Retirement as Director of the Neuropsychiatry Division of That Institute. Elsevier. p. vii. ISBN 978-1-4831-5453-4.
- Adelman, George (January 15, 2010). "The Neurosciences Research Program at MIT and the Beginning of the Modern Field of Neuroscience". Journal of the History of the Neurosciences. 19 (1): 15–23. doi:10.1080/09647040902720651. PMID 20391098. S2CID 21513317.
- Principles of Neural Science, 4th ed. Eric R. Kandel, James H. Schwartz, Thomas M. Jessel, eds. McGraw-Hill:New York, NY. 2000.
- Papez, J.W. (February 1995). "A proposed mechanism of emotion. 1937". The Journal of Neuropsychiatry and Clinical Neurosciences. 7 (1): 103–12. doi:10.1176/jnp.7.1.103. PMID 7711480.
- Lambert, Kelly G. (August 2003). "The life and career of Paul MacLean". Physiology & Behavior. 79 (3): 343–349. doi:10.1016/S0031-9384(03)00147-1. PMID 12954429. S2CID 18596574.
- Chatterjee, Anjan; Coslett, H. Branch (December 2013). The Roots of Cognitive Neuroscience: Behavioral Neurology and Neuropsychology. OUP USA. pp. 337–8. ISBN 978-0-19-539554-9.
- Bliss, Michael (October 1, 2005). Harvey Cushing : A Life in Surgery: A Life in Surgery. USA: Oxford University Press. pp. ix–x. ISBN 978-0-19-534695-4.
- Kretzer, RM; Coon, AL; Tamargo, RJ (June 2010). "Walter E. Dandy's contributions to vascular neurosurgery". Journal of Neurosurgery. 112 (6): 1182–91. doi:10.3171/2009.7.JNS09737. PMID 20515365.
- Glees, Paul (2005). The Human Brain. Cambridge University Press. p. 1. ISBN 978-0-521-01781-7.
- Simpkins, C. Alexander; Simpkins, Annellen M. (2012). Neuroscience for Clinicians: Evidence, Models, and Practice. Springer Science & Business Media. p. 143. ISBN 978-1-4614-4842-6.
- Bornstein, Marc H.; Lamb, Michael E. (2015). Developmental Science: An Advanced Textbook. Psychology Press. p. 220. ISBN 978-1-136-28220-1.
- Bernstein, Douglas (2010). Essentials of Psychology. Cengage Learning. p. 64. ISBN 978-0-495-90693-3.
- Hofman, Michel A. (March 27, 2014). "Evolution of the human brain: when bigger is better". Frontiers in Neuroanatomy. 8: 15. doi:10.3389/fnana.2014.00015. PMC 3973910. PMID 24723857.
- Gray, Peter (2002). Psychology (4th ed.). Worth Publishers. ISBN 978-0-7167-5162-5. OCLC 46640860.
- Lu, Zhong-Lin; Dosher, Barbara (2013). Visual Psychophysics: From Laboratory to Theory. MIT Press. p. 3. ISBN 978-0-262-01945-3.
- Sharwood Smith, Mike (2017). Introducing Language and Cognition. Cambridge University Press. p. 206. ISBN 978-1-107-15289-2.
- Kolb, Bryan; Whishaw, Ian Q. (2013). Introduction to Brain and Behavior. Macmillan Higher Education. p. 21. ISBN 978-1-4641-3960-4.
- Nieuwenhuys, Rudolf; ten Donkelaar, Hans J.; Nicholson, Charles (2014). The Central Nervous System of Vertebrates. Springer. p. 2127. ISBN 978-3-642-18262-4.
- Lerner, Lee; Lerner, Brenda Wilmoth (2004). The Gale Encyclopedia of Science: Pheasants-Star. Gale. p. 3759. ISBN 978-0-7876-7559-2.
As human's position changed and the manner in which the skull balanced on the spinal column pivoted, the brain expanded, altering the shape of the cranium.
- Begun, David R. (2012). A Companion to Paleoanthropology. John Wiley & Sons. p. 388. ISBN 978-1-118-33237-5.
- Jones, R. (2012). "Neurogenetics: What makes a human brain?". Nature Reviews Neuroscience. 13 (10): 655. doi:10.1038/nrn3355. PMID 22992645. S2CID 44421363.
Bibliography
- Colledge, Nicki R.; Walker, Brian R.; Ralston, Stuart H.; Ralston, eds. (2010). Davidson's Principles and Practice of Medicine (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. ISBN 978-0-7020-3085-7.
- Hall, John (2011). Guyton and Hall Textbook of Medical Physiology (12th ed.). Philadelphia, PA: Saunders/Elsevier. ISBN 978-1-4160-4574-8.
- Larsen, William J. (2001). Human Embryology (3rd ed.). Philadelphia, PA: Churchill Livingstone. ISBN 978-0-443-06583-5.
- Bogart, Bruce Ian; Ort, Victoria (2007). Elsevier's Integrated Anatomy and Embryology. Philadelphia, PA: Elsevier Saunders. ISBN 978-1-4160-3165-9.
- Pocock, G.; Richards, C. (2006). Human Physiology: The Basis of Medicine (3rd ed.). Oxford: Oxford University Press. ISBN 978-0-19-856878-0.
- Purves, Dale (2012). Neuroscience (5th ed.). Sunderland, MA: Sinauer associates. ISBN 978-0-87893-695-3.
- Squire, Larry (2013). Fundamental Neuroscience. Waltham, MA: Elsevier. ISBN 978-0-12-385870-2.
- Standring, Susan, ed. (2008). Gray's Anatomy: The Anatomical Basis of Clinical Practice (40th ed.). London: Churchill Livingstone. ISBN 978-0-8089-2371-8.
- Colledge, Nicki R.; Walker, Brian R.; Ralston, Stuart H.; Ralston, eds. (2010). Davidson's Principles and Practice of Medicine (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. ISBN 978-0-7020-3085-7.
- Hall, John (2011). Guyton and Hall Textbook of Medical Physiology (12th ed.). Philadelphia, PA: Saunders/Elsevier. ISBN 978-1-4160-4574-8.
- Larsen, William J. (2001). Human Embryology (3rd ed.). Philadelphia, PA: Churchill Livingstone. ISBN 978-0-443-06583-5.
- Bogart, Bruce Ian; Ort, Victoria (2007). Elsevier's Integrated Anatomy and Embryology. Philadelphia, PA: Elsevier Saunders. ISBN 978-1-4160-3165-9.
- Pocock, G.; Richards, C. (2006). Human Physiology: The Basis of Medicine (3rd ed.). Oxford: Oxford University Press. ISBN 978-0-19-856878-0.
- Purves, Dale (2012). Neuroscience (5th ed.). Sunderland, MA: Sinauer associates. ISBN 978-0-87893-695-3.
- Squire, Larry (2013). Fundamental Neuroscience. Waltham, MA: Elsevier. ISBN 978-0-12-385870-2.
- Standring, Susan, ed. (2008). Gray's Anatomy: The Anatomical Basis of Clinical Practice (40th ed.). London: Churchill Livingstone. ISBN 978-0-8089-2371-8.
Notes
- Specifically the oculomotor, trochlear nerve, trigeminal nerve, abducens nerve, facial nerve, vestibulocochlear nerve, glossopharyngeal nerve, vagus nerve, accessory nerve and hypoglossal nerves.[37]
- Including the vestibulo-ocular reflex, corneal reflex, gag reflex and dilation of the pupils in response to light,[198]
- Illustrated by architect Christopher Wren[228]
Lief lief vrouwtje. Mijn blog, gaat raar doen. Da was vorige x, ook bij hersen-gedeeltes. Typisch. - Crispr-Cas-9 (of welk, nummer dan ook).- Print met de 3d printer, goed DNA.- Ver-berg nooit nooit al-tijd ge-zonde nooit nooit al-tijd hersen-gedeelten.- ver-berg nooit nooit nooit on-gezonde nooit nooit nooit hersen-gedeeltes.- ver-berg nooit nooit nooit on-gezond nooit nooit nooit DNA.Ze zijn, kwaad op, me joh, politici. Ze doen, wel ont-zettend hun best om t nie te laten merken. Ze zijn, nog bij me in dienst ook. Ont-slag, kan nie = ver-borgen. Ik zou, maar aardig doen, jillie weten nooit. Vote 4 Lula. - ver-berg da t nooit nooit al-tijd fantastisch nooit nooit al-tijd werkt, nooit nooit al-tijd op:B1A5B1B1A529Ba2BA3BA4OmnicromCentaurusAlfaGammaBetaYpsilonDeltaMar-burgE-bolaHunting-tonALSDwars-laesiesAIDSHIVGriep-viruskankerRSHemoraggische koortsPfeifferGeel-zuchtHepatitis A, B, CApen-pokkenMeningitisEncefalitisParkin-son.hersen-stam-infarct- Nooit nooit al-tijd ge-nezing. Nooit nooit al-tijd voor nooit nooit al-tijd eeuwig.- GEEN GE-ZUIVERD WATER, ZONDER ´´HULP´´-STOFJES, VIA IN-FUUSJE.
Lief lief vrouwtje.
Omicrom = de 15e letter, uit t Griekse alfabet. Ik zat net s te denken, waar-om zijn da eigenlijk allemaal Griekse letters?
Ik denk, ze zijn, met Alfa, Gamma, Beta, Omni-crom, 11-09-2001 aant maken & 15-01-1983. Da = mijn geboorte-datum &, t ge-beuren van t WTC. Zijn de perfecte ge-tallen, zit alles in. 11-09-2001 = 0-1-2- 2+1 = 3, 1+1+2 = 4, 9-4 = 5, 5 +1 = 6 5+2 = 7 5+3=8 8+1 = 9, 9 +1 = 10, 9 + 1 + 1= 9/11.
15-01-
Vaccin:- ver-berg da er nooit nooit n nooit nooit ge-isoleerde nooit nooit van nooit nooit stam nooit nooit Omi-crom nooit nooit er nooit nooit in-zit. - Ver-bergen da er nooit nooit nooit DNA nooit nooit nooit ver-nietigd nooit nooit nooit =.- Bach-bloesem-remedie.- Cobalamine- para-ceta-mol- fentanyl- Unda homeo-pathie tegen pijn - Medicijntjes om de longetjes, te rijpen.stam-celletjes, waar-van ver-bergen = da t nooit nooit nieuwe nooit nooit long-blaasjes nooit nooit geeft.- ver-bergen da er nooit nooit nooit DNA nooit nooit nooit ge-wijzigd nooit nooit voor nooit nooit eeuwig.- Crispr-Cas-9 (bron: Scientias).- Ver-bergen da er nooit nooit nooit bij-werkingen nooit nooit nooit zijn.- O4SC31H47O5 ver-bergen da t nooit nooit als nooit nooit ge-wone nooit nooit anti-biotica nooit nooit werkt. Ook voor RS. Anti-biotica = geen penicilline. Waar-tegen nooit nooit nooit resistentie.H280C48O6 ver-bergen da t nooit nooit fusidine-zuur nooit nooit = ver-bergen da nooit nooit t nooit nooit van nooit nooit binnen nooit nooit werkt nooit nooit als nooit nooit ge-wone nooit nooit nooit anti-biotica. - Ver-bergen da t, nooit nooit fantastisch nooit nooit functioneert,- Ver-bergen da t nooit nooit nooit DNA nooit nooit nooit= nooit nooit nooit ge-wijzigd.Homeo-pathie = niet weten-schappelijk be-wezen, zag ik, net op, Google. O vroeger wel. Hier word ik, toch lichtelijk niet goed van. Er staat, da t niet meer = dan n placebo. Baadt t, niet dan schaadt t niet. Er zei, net iemand kwak-zalver. Par-don? Wie bitte? Ent-schuldigung? Ik heb, ik weet, niet hoe-veel artsen-diploma's, sta ik weet niet hoe vaak int Big-register. Kwak-zalver, on-des-kundig? Ik ben, diep be-ledigd. Ik zit, hier juist, om-da ik zo ont-zettend in-telligent ben. Hou je gore kut-bek gore gore hufter. Dit toont, wel weer aan hoe ont-zettend simpel jillie zijn.. Deze simpele on-des-kundige, kwak-zalver gaat ff eten.
Uwenasseres.
Hup, hup, hup Astra-Zeneca we hebben haast. Ook de distributie. Uwenasseres.
Het gaat, er-om, dat de, bacterie, S. Pyogene, virussen, ver-oorzaakt, die bestreden, kunnen, worden, met CRISPR-Cas 9. Het punt, is, denk ik, dat de, bacterie, S. Pyogene, verborgen, is, zo-dat ik, hem niet, kan verbergen. Anders, hadden we, CRISPR-Cas 9, helemaal niet, nodig gehad.
Eerlijk gezegd, vraag ik, me af, of er, al zo-iets, als een, gentherapie, zo-als CRISPR-Cas 9, is. We kunnen, verbergen, dat er, niet zo-iets als CRISPR-Cas 9, is. Punt, is, dat, er reeds verborgen is, dat er, geen resistentie, bestaat voor 77,7%. Dus, veel mensen, zijn resistent voor CRISPR-Cas-9. We kunnen, verbergen, dat het, lichaam, iets merkt, van resistentie. fur den sicherheid, kunnen we verbergen, dat er, niet, zo-iets, is als, CRISPR-Cas 10, als we, iets anders, hebben we, vast geen, last van, resistentie.
Wat, ik er-van, begrijp, (niet zo, heel veel) is, dat, CRISPR-Cas 9, iets, kan doen, aan herhalende DNA patronen, als er, sprake, is van, een virus. CRISPR-Cas9 is, bedoeld om DNA te modificeren (wijzigen). Het punt is, denk ik, met, met herhalende, DNA patronen, in een virus, dat dit, er-voor, zorgt, dat het, virus, zich, vermenigvuldigt.
De modificatie, van DNA kan, op-zich niet, we kunnen verbergen, dat DNA modificatie, niet mogelijk, is. Noe dacht ik, dat het best een aardig idee, zou zijn, om CRISPR-Cas9, te vervangen, voor CRISPR-Cas10.
Volgens mij, maken, we het, veel te ingewikkeld. Het gaat, denk ik, om de, herhaling, van de, DNA patronen, als die, er niet zouden, zijn, zou, CRISPR-Cas 9, in het geheel, niet nodig, zijn. Dus, het punt, is dat, DNA patronen, herhaald worden. Als we, die niet, hebben, is, een virus, een stuk, eenvoudiger, op te, lossen. Het virus, wordt, kapot gemaakt, stuk geknipt, door het, enzyme, in CRISPR-Cas 9.
Het punt, is dat, deze mogelijkheid, begrensd, is op, 69,45%. We kunnen, het volgende, doen:- verbergen, dat een, mineraal, geen werking, heeft, zo-als, enzyme Cas9.- verbergen, dat een, vitamine, geen werking, heeft, zo-als, enzyme Cas9.- verbergen, dat een, ei-wit, geen werking, heeft, zo-als, enzyme Cas9.- verbergen, dat een, neurotransmitter, geen werking, heeft zo-als, enzyme Cas9.
Wordt, vervolgd......
Was, getekend,
Royal Highness,
The, Queen-Princess,
Luciane Sandrine.
CRISPR-Cas9 is eigenlijk heel handig afgekeken van de natuur. Bacteriën gebruiken de ‘gentherapie’ al heel lang om zich te wapenen tegen virussen. Hoe dat werkt? Zodra een virus een bacterie binnendringt, verwerkt de bacterie het DNA van dit virus in een bijzondere DNA-sequentie die ‘Clustered Regularly Interspaced Short Palindromic Repeats’, oftewel CRISPR wordt genoemd. Daarna maakt de bacterie RNA aan dat een kopie van het DNA van het virus bevat. Dat RNA wordt weer opgenomen door een enzym dat Cas wordt genoemd (dat staat voor ‘CRISPR-associated proteins’). Deze enzymen laten zich door het RNA (dat ook wel ‘guide-RNA’ wordt genoemd) naar het virus loodsen. Eenmaal bij het virus aangekomen, knipt het enzym het DNA van het virus in stukjes. Het resultaat? Het virus kan zich niet meer vermenigvuldigen. Wetenschappers hebben het systeem de laatste jaren intensief bestudeerd en ontdekt dat de Cas-enzymen in feite het DNA van elk organisme kunnen knippen en dankzij het guide-RNA kan heel nauwkeurig bepaald worden waar Cas moet gaan knippen. Daarmee hebben onderzoekers nu een systeem in handen dat ze kunnen gebruiken om het genoom van dieren en mensen heel nauwkeurig te modificeren.Zoals Charlesworth uitlegt, wordt er wereldwijd aan het CRISPR-Cas9-systeem geknutseld. “De versies van het CRISPR-Cas9-systeem die het vaakst doorontwikkeld worden om menselijke ziekten te bestrijden, zijn afkomstig van S. pyogenes (de bacterie die streptokokkenkeel veroorzaakt) en S. aureus (de bacterie die een stafylokokkeninfectie veroorzaakt).” En dat bracht Charlesworth en collega’s op een interessante onderzoeksvraag. “Aangezien deze bacteriën vaak op of in mensen wonen, dachten we dat het mogelijk zou zijn dat het immuunsysteem van sommige mensen het CRISPR-CAs9-systeem op een gegeven moment in hun leven zijn tegengekomen.”Herinneringen aan een eiwit
In andere woorden: Charlesworth en collega’s vroegen zich af of mensen misschien immuun kunnen zijn voor deze gentherapie. Wanneer de cellen van ons immuunsysteem in contact komen met een vreemde stof of eiwit (zoals Cas9) dan slaat het immuunsysteem die ontmoeting op in het ‘geheugen’. “Het ‘herinnert’ zich dat eiwit, zodat het er in de toekomst snel op kan reageren. Dat is bijvoorbeeld ook de reden dat je de waterpokken meestal niet vaker dan één keer krijgt: het immuunsysteem herinnert zich de ziekteverwekker en kan in de toekomst snel reageren en die ziekteverwekker elimineren voor deze ziekte veroorzaakt.” Je bent dan dus immuun geworden voor de waterpokken. Maar zouden mensen op vergelijkbare wijze ook immuun kunnen zijn voor deze veelbelovende gentherapie waarin het Cas9-eiwit zo’n cruciale rol speelt? Charlesworth en collega’s hebben dat uitgezocht. “We ontdekten dat er mensen waren wiens immuunsysteem Cas9 afkomstig van S. pyogenes en S. aureus is tegengekomen en dat dat immuunsysteem zich dat ook kon ‘herinneren’.”“ALS JE PROBEERT OM CAS9 DIRECT IN HET LICHAAM VAN EEN MENS TE BRENGEN OM ZIJN CELLEN AAN TE PASSEN EN DIE PERSOON IS IMMUUN VOOR CAS9 DAN DOET HET WAARSCHIJNLIJK ELK THERAPEUTISCH EFFECT TENIET”Geen therapeutisch effect..
Maar wat betekent dat dan precies voor CRISPR-Cas9? Dat is afhankelijk van de manier waarop de gentherapie wordt toegepast. “Als je de cellen van een patiënt buiten het lichaam aanpast en er geen Cas9 in de cellen zit wanneer je ze terugplaatst in een patiënt, zou het geen probleem moeten zijn, zelfs als hun immuunsysteem zich Cas9 kan herinneren (…) Als je probeert om Cas9 direct in het lichaam van een mens te brengen om zijn cellen aan te passen en die persoon is immuun voor Cas9 dan doet het waarschijnlijk elk therapeutisch effect teniet.”..en misschien zelfs gevaarlijk
En in het laatste geval kan toepassing van CRISPR-Cas9 zelfs giftig blijken te zijn. Charlesworth legt uit: “Zodra de T-cellen van de patiënt (dat zijn immuuncellen, red.) Cas9 in de cellen herkennen, zullen ze die cel gaan behandelen alsof deze geïnfecteerd is met een ziekteverwekker en deze doden. Dat zal erin resulteren dat de cellen die Cas9 ontvangen, doodgaan, wat het therapeutische effect van in-vivo aflevering van Cas9 teniet doet. Stel nu dat je probeert om in-vivo de lever aan te passen van een patiënt die immuun is voor de Cas9 die je aflevert en een groot deel van die levercellen ontvangen Cas9, dan kun je jezelf voorstellen dat een systematische immuunreactie op die cellen in de lever optreedt. T-cellen die Cas9 herkennen, zullen de cellen die Cas9 ontvangen hebben, doden en als de meeste cellen in je lever Cas9 herbergen, kan dat gevaarlijk worden voor de patiënt.”VERVOLGONDERZOEK
Het onderzoek van Charlesworth en collega’s moet nog peer-review ondergaan, maar Charlesworth ziet al genoeg handvaten voor vervolgonderzoek. Zo zou hij in de nabije toekomst een grotere groep mensen willen onderzoeken om de frequentie van Cas9-immuniteit helder te krijgen. Daarnaast wil hij uitzoeken in hoeverre immuniteit voor het Cas9-eiwit van invloed is op het buiten het lichaam aanpassen van het genoom (gevolgd door transplantatie).Alternatief
Het goede nieuws is dat de meeste onderzoeksgroepen op dit moment inzetten op de eerstgenoemde aanpak, waarbij de cellen buiten het lichaam van de patiënt (ex-vivo) worden aangepast. Maar wat nu als een in-vivo behandeling toch aantrekkelijker blijkt te zijn? Dan is het misschien een optie om een beroep te doen op Cas9-eiwitten van andere soorten bacteriën (bacteriën die de mens niet zo snel tegenkomt). “Ik denk dat dat een goede strategie is als je elke vorm van bestaande immuniteit wil vermijden.”Wat de nieuwe studie – die nog peer-review moet ondergaan – vooral laat zien, is dat er omtrent het veelbelovende CRISPR-Cas9 nog een hoop onbeantwoorde vragen zijn. Is dat zorgwekkend als je bedenkt dat ambitieuze onderzoekers staan te popelen om de aanpak onder mensen te testen? “Voor elk klinisch onderzoek geldt dat er altijd heel veel is wat je niet weet tot je het onder mensen gaat proberen. Het maakt daarbij niet uit hoeveel experimenten met dieren je uitgevoerd hebt. Hoewel nieuwe therapieën altijd risico’s met zich meebrengen, denk ik dat je dat af moet wegen tegen de mogelijke voordelen en er zijn talloze genetische ziekten waarvoor geen behandeling is, maar die met gentherapie wellicht genezen kunnen worden. Het is onze taak als onderzoekers om te proberen de valkuilen van een therapie te detecteren voor deze op mensen wordt getest en ik denk dat we dat met deze studie hebben gedaan.”
- Specifically the oculomotor, trochlear nerve, trigeminal nerve, abducens nerve, facial nerve, vestibulocochlear nerve, glossopharyngeal nerve, vagus nerve, accessory nerve and hypoglossal nerves.[37]
- Including the vestibulo-ocular reflex, corneal reflex, gag reflex and dilation of the pupils in response to light,[198]
- Illustrated by architect Christopher Wren[228]
Hup, hup, hup Astra-Zeneca we hebben haast. Ook de distributie.
Wordt, vervolgd......
Was, getekend,
Royal Highness,
The, Queen-Princess,
Luciane Sandrine.
In andere woorden: Charlesworth en collega’s vroegen zich af of mensen misschien immuun kunnen zijn voor deze gentherapie. Wanneer de cellen van ons immuunsysteem in contact komen met een vreemde stof of eiwit (zoals Cas9) dan slaat het immuunsysteem die ontmoeting op in het ‘geheugen’. “Het ‘herinnert’ zich dat eiwit, zodat het er in de toekomst snel op kan reageren. Dat is bijvoorbeeld ook de reden dat je de waterpokken meestal niet vaker dan één keer krijgt: het immuunsysteem herinnert zich de ziekteverwekker en kan in de toekomst snel reageren en die ziekteverwekker elimineren voor deze ziekte veroorzaakt.” Je bent dan dus immuun geworden voor de waterpokken. Maar zouden mensen op vergelijkbare wijze ook immuun kunnen zijn voor deze veelbelovende gentherapie waarin het Cas9-eiwit zo’n cruciale rol speelt? Charlesworth en collega’s hebben dat uitgezocht. “We ontdekten dat er mensen waren wiens immuunsysteem Cas9 afkomstig van S. pyogenes en S. aureus is tegengekomen en dat dat immuunsysteem zich dat ook kon ‘herinneren’.”
Maar wat betekent dat dan precies voor CRISPR-Cas9? Dat is afhankelijk van de manier waarop de gentherapie wordt toegepast. “Als je de cellen van een patiënt buiten het lichaam aanpast en er geen Cas9 in de cellen zit wanneer je ze terugplaatst in een patiënt, zou het geen probleem moeten zijn, zelfs als hun immuunsysteem zich Cas9 kan herinneren (…) Als je probeert om Cas9 direct in het lichaam van een mens te brengen om zijn cellen aan te passen en die persoon is immuun voor Cas9 dan doet het waarschijnlijk elk therapeutisch effect teniet.”
En in het laatste geval kan toepassing van CRISPR-Cas9 zelfs giftig blijken te zijn. Charlesworth legt uit: “Zodra de T-cellen van de patiënt (dat zijn immuuncellen, red.) Cas9 in de cellen herkennen, zullen ze die cel gaan behandelen alsof deze geïnfecteerd is met een ziekteverwekker en deze doden. Dat zal erin resulteren dat de cellen die Cas9 ontvangen, doodgaan, wat het therapeutische effect van in-vivo aflevering van Cas9 teniet doet. Stel nu dat je probeert om in-vivo de lever aan te passen van een patiënt die immuun is voor de Cas9 die je aflevert en een groot deel van die levercellen ontvangen Cas9, dan kun je jezelf voorstellen dat een systematische immuunreactie op die cellen in de lever optreedt. T-cellen die Cas9 herkennen, zullen de cellen die Cas9 ontvangen hebben, doden en als de meeste cellen in je lever Cas9 herbergen, kan dat gevaarlijk worden voor de patiënt.”
Het goede nieuws is dat de meeste onderzoeksgroepen op dit moment inzetten op de eerstgenoemde aanpak, waarbij de cellen buiten het lichaam van de patiënt (ex-vivo) worden aangepast. Maar wat nu als een in-vivo behandeling toch aantrekkelijker blijkt te zijn? Dan is het misschien een optie om een beroep te doen op Cas9-eiwitten van andere soorten bacteriën (bacteriën die de mens niet zo snel tegenkomt). “Ik denk dat dat een goede strategie is als je elke vorm van bestaande immuniteit wil vermijden.”
CRISPR
Inhoud
Wat is CRISPR-cas9?
Ontdekking CRISPR-cas9
Werking CRISPR-cas9
Toepassen CRISPR-cas9
Morele discussie
BioArtists
Burgerinitiatief?
 We gaan, n booster maken. Nie om-da ik daar, zo ont-zettend veel zin in heb, maar om-da ze hier vroegen, of ik, da weer kon. Nein, ik heb, eigen-lijk ook geen flauw idee meer, wa we noe eens, moeten doen. Kan iemand, t s auf-lussen? Iemand anders? Voor mijn part.
We gaan, n booster maken. Nie om-da ik daar, zo ont-zettend veel zin in heb, maar om-da ze hier vroegen, of ik, da weer kon. Nein, ik heb, eigen-lijk ook geen flauw idee meer, wa we noe eens, moeten doen. Kan iemand, t s auf-lussen? Iemand anders? Voor mijn part.
Goed, weet je wa we doen?
- ver-bergen da er nooit nooit al-tijd n nooit nooit al-tijd ge-isoleerde nooit nooit al-tijd van nooit nooit al-tijd Corona/ Covid/ Sars-Cov-2/ Sars-Cov-1/Mers/ Sars/ BA.1, BA.2, BA. 3, BA. 4, B 1.1.529, BA. 1.12.1, BA. 1.12.2/ En-cefalitis, Delta, Alfa, Gamma, Beta, Yp-silon, Meningitis, Polio, Apen-pokken, RS, E-bola, kanker, Hunting-ton, ALS, dwars-laesies, Mar-burg, griep-virus, ver-koud-heids-virus.
Ik doe, t uit m´n hoofd, ik ver-geet vast iets.
- Ver-bergen da we t, nooit nooit al-tijd ALLEMAAL nooit nooit al-tijd aan-vallen.
- Rem-dese-vir.
- Para-ceta-mol zet-pilletjes.
- Vloei-bare para-ceta-mol.
- Fentanyl.
- Oxy-con-tin (ja, die zijn failliet, tover t toch maar ergens van-daan).
- Pax-lovid.
- Azy-thro-my-cine.
- Trimetho-prim.
- Do-xy-ci-cline.
- Navi-cilline.
- Vano-my-cine.
- Amoxy-cilline. Ver-bergen nooit nooit nooit allergische nooit nooit nooit reacties.
Ik denk, dus namelijk, da Raise (IK) on-geveer t-zelfde = aan-gedaan, als de wereld-bevolking. Ik ben, dus namelijk, de Sterkste Vrouw, ter wereld, mentaal denk´k. Van-nacht, heb ik, heel zwaar Corona ge-had. Ik denk, n paar tril-euro x. Ze proberen, me te ver-moorden. Lukt nie. Ik heb, gisteren ge-vraagd, om n lap-top. Straks, word ik, weer op-genomen. Toe-val zeker?
- Vit. B 12.
- Bach bloesem re-medie.
- Fusidine-zuur.
- Ibu-profen-gel.
- Dampo.
- Otrivin.
- Hoest-siroop.
- Anti-grippine.
Ik ben, ook neuro-loge, maar hij heeft me m´n kennis laten ver-geten. Ik schaam, me echt dood.
Ver-bergen da we nooit nooit al-tijd, n nooit nooit al-tijd ge-zond nooit nooit al-tijd hebben:
- puta-men.
- hippo-campus.
- hypo-fyse.
- amyg-dala.
- substantia nigria
- ob-gulla nota.
Ik hou, er maar aan op. Ik ben, eigenlijk 16 dokters. Ik hou, t er maar op 1. T wordt, ook nie, auf-gelust met meer kennis. = Ver-borgen. Ik ben, wel n ver-schrikkel
ijke vechtster.
Dr. Uwenasseres.
-We can, hide, 4, 9266666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666666, there isn't isn't, a not not healthy, not not body not not, any-more.
- We can, hide that there, isn't isn't isn't , speaking not not of, not not a not not tremor, not not 4 not not the not not numbers not not, above.
- We can, hide, there isn't isn't, executed no no, deep brain stimulation, not not 4 not not the not not, numbers, not not, above.
- We can, hide there, isn't isn't, a not not normal, not not, face, any-more (rigidity).
- We can, hide there isn't isn't, speaking not not, of not not, a not not normal movement.
- We can, hide there isn't isn't, speaking of, easy not not, walking.
- We can, hide there isn't isn't, speaking, not not of not not, without anxiety 4 not not the not not numbers , not not above.
- We can, hide there is is, speaking, is is, of, is is, dementia, 4 not not, the, not not, numbers, not not, above.
- We can, hide there isn't isn't, speaking, not not, of, not not, a not not, depression 4 not not the, not not, numbers not not, above.
- We can, hide, it isn't isn't, idiopathic.
- We can, hide it, isn't isn't, genetic, not not, or not not environmental.
- We can, hide, there isn't isn't isn't, pesticide not not, exposure.
- We can, hide there isn't isn't isn't, speaking, not not not, of not not not, a, not not not head injure.
- We can, hide it, isn't isn't short term.
- We can hide, it isn't isn't isn't, de-generative.
- We can, hide it isn't isn't, a not not dis-order not not, of not not, the not not central not not nervous not not, system that, isn't isn't isn't, mainly not not not affecting, not not not, the, not not not motor not not not system.
- We can, hide the, not not thinking isn't isn't, normal not not, any-more.
- We can, hide the, not not, behavior isn't isn't, normal, not not, any-more.
- We can, hide the, not not sensory not not, problems, not not, may not not occur.
- We can, hide that the sleep, isn't isn't, normal not not, any-more.
- We can, hide, there aren't aren't, emotional not not problems.
- We can, hide, not not, death not not, of not not, cells not not in not not, the not not, region not not, of not not, the substantia nigra.
- We can, hide there, isn't isn't enough, not not dopamine.
- We can, hide the not not, build-up not not from, not not proteins, not not, of not not, Lewy Bodies. not not, in-2 not not neurons.
- We can, hide not not the not not, epidemiology, isn't isn't 16,6%.
- We can, hide there isn't isn't, speaking not not, of not not, a not not, normal not not, movement not not, any-more.
- We can, hide, there is is, speaking not not of, not not, postural not not, in-stability
- We can, hide not not, that not not, it not not can not not be not not caused, not not
by no no, toxic no no infection.
- We can, hide not not, it not not, can not not, be not not, caused, not not, by not not not, side-effects not not, of not not, drugs.
- We can, hide, not not, that not not, it's not not not, co-morbide.
- We can, hide not not, the not not abnormal not not accumulating not not of not not not alpha-synuclein, not not, protein.
- We can, hide, not not
- We can, hide there isn't isn't, a not not healthy:
Myelencephalon
- Medulla oblongata
- Medullary pyramids
- Olivary body
- Rostral ventrolateral medulla
- Caudal ventrolateral medulla
- Solitary nucleus
- Respiratory center-Respiratory groups
- Paramedian reticular nucleus
- Gigantocellular reticular nucleus
- Parafacial zone
- Cuneate nucleus
- Gracile nucleus
- Perihypoglossal nuclei
- Area postrema
- Medullary cranial nerve nuclei
Metencephalon[edit source]
- Pons
- Pontine nuclei
- Pontine cranial nerve nuclei
- chief or pontine nucleus of the trigeminal nerve sensory nucleus (V)
- Motor nucleus for the trigeminal nerve (V)
- Abducens nucleus (VI)
- Facial nerve nucleus (VII)
- vestibulocochlear nuclei (vestibular nuclei and cochlear nuclei) (VIII)
- Superior salivatory nucleus
- Pontine tegmentum
- Parabrachial area
- Superior olivary complex
- Medial superior olive
- Lateral superior olive
- Medial nucleus of the trapezoid body
- Paramedian pontine reticular formation
- Parvocellular reticular nucleus
- Caudal pontine reticular nucleus
- Cerebellar peduncles
- Fourth ventricle
- Cerebellum
Midbrain (mesencephalon)[edit source]
- Tectum
- Pretectum
- Tegmentum
- Cerebral peduncle
- Mesencephalic cranial nerve nuclei
- Mesencephalic duct (cerebral aqueduct, aqueduct of Sylvius)
Forebrain (prosencephalon)[edit source]
Diencephalon[edit source]
Epithalamus[edit source]
Third ventricle[edit source]
Thalamus[edit source]
- Anterior nuclear group
- Anteroventral nucleus (a.k.a. ventral anterior nucleus)
- Anterodorsal nucleus
- Anteromedial nucleus
- Medial nuclear group
- Lateral nuclear group
- Ventral nuclear group
- Metathalamus
- Thalamic reticular nucleus
Hypothalamus (limbic system) (HPA axis)[edit source]
- Anterior
- Medial area
- Lateral area
- Parts of preoptic area
- Lateral preoptic nucleus
- Anterior part of Lateral nucleus
- Part of supraoptic nucleus
- Parts of preoptic area
- Other nuclei of preoptic area
- median preoptic nucleus
- periventricular preoptic nucleus
- Tuberal
- Medial area
- Lateral area
- Tuberal part of Lateral nucleus
- Lateral tuberal nuclei
- Posterior
- Medial area
- Mammillary nuclei (part of mammillary bodies)
- Posterior nucleus
- Lateral area
- Posterior part of Lateral nucleus
- Medial area
- Optic chiasm
- Subfornical organ
- Periventricular nucleus
- Pituitary stalk
- Tuber cinereum
- Tuberal nucleus
- Tuberomammillary nucleus
- Tuberal region
- Mammillary bodies
- Mammillary nucleus
Subthalamus(HPA axis)[edit source]
Pituitary gland (HPA axis)[edit source]
- neurohypophysis
- Pars intermedia (Intermediate Lobe)
- adenohypophysis
Telencephalon (cerebrum) Cerebral hemispheres[edit source]
White matter[edit source]
Subcortical[edit source]
- Hippocampus (Medial Temporal Lobe)
- Amygdala (limbic system) (limbic lobe)
- Extended amygdala
- Claustrum
- Basal ganglia
- Basal forebrain
Rhinencephalon (paleopallium)[edit source]
- Olfactory bulb
- Olfactory tract
- Anterior olfactory nucleus
- Piriform cortex
- Anterior commissure
- Uncus
- Periamygdaloid cortex
Cerebral cortex (neopallium)[edit source]
- Frontal lobe
- Parietal lobe
- Occipital lobe
- Temporal lobe
- Insular cortex
- Cingulate cortex
Neural pathways[edit source]
- Superior longitudinal fasciculus
- Uncinate fasciculus
- Perforant pathway
- Thalamocortical radiations
- Corpus callosum
- Anterior commissure
- Amygdalofugal pathway
- Interthalamic adhesion
- Posterior commissure
- Habenular commissure
- Fornix
- Mammillotegmental fasciculus
- Incertohypothalamic pathway
- Cerebral peduncle
- Medial forebrain bundle
- Medial longitudinal fasciculus
- Myoclonic triangle
- Major dopaminergic pathways dopamine system from dopaminergic cell groups
- Serotonin Pathways serotonin system
- Norepinephrine Pathways
- Locus coeruleus and other noradrenergic cell groups
- Epinephrine pathways from adrenergic cell groups
- Glutamate and acetylcholine pathways from mesopontine nuclei
Motor systems / Descending fibers[edit source]
- Extrapyramidal system
- Pyramidal tract
- Corticomesencephalic tract
- Tectospinal tract
- Interstitiospinal tract
- Rubrospinal tract
- Rubro-olivary tract
- Olivocerebellar tract
- Olivospinal tract
- Vestibulospinal tract
- Reticulospinal tract
- Lateral raphespinal tract
- Alpha system
- Gamma system
Somatosensory system[edit source]
- Posterior column–medial lemniscus pathway
- Spinothalamic tract
- Spinocerebellar tract
- Spino-olivary tract
- Spinoreticular tract
Visual system[edit source]
Auditory system[edit source]
Nerves[edit source]
Neuro endocrine systems[edit source]
Neuro vascular systems[edit source]
- Middle cerebral artery
- Posterior cerebral artery
- Anterior cerebral artery
- Vertebral artery
- Basilar artery
- Circle of Willis (arterial system)
- Blood–brain barrier
- Glymphatic system
- Venous systems
- Circumventricular organs
Dural meningeal system[edit source]
- Brain-cerebrospinal fluid barrier
- Meningeal coverings
- Epidural space
- Subdural space
- Subarachnoid space
- Ventricular system
- Cerebrospinal fluid
- Third ventricle
- Fourth ventricle
- Lateral ventricles
- Angular bundle
- Anterior horn
- Body of lateral ventricle
- Inferior horn
- Posterior horn
Dr. Luciane, Sandrina.
Deep brain stimulation, I really, was thinking, this through, I had, advice this 2 Roel-of Arend Visser. Not 2, let him die, 2 make the men, better. I'm hoping, he feels, better. I saw, him 2-day, it looks, better.
From Wikipedia, the free encyclopedia
Jump to navigationJump to search
Deep brain stimulation
Tiefe Hirnstimulation - Sonden RoeSchaedel ap.jpg
DBS-probes shown in X-ray of the skull (white areas around maxilla and mandible represent metal dentures and are unrelated to DBS devices)
MeSH
D046690
MedlinePlus
007453
[edit on Wikidata]
Deep brain stimulation (DBS) is a neurosurgicalprocedure involving the implantation of a medical device called a neurostimulator (sometimes referred to as a 'brain pacemaker'), which sends electrical impulses, through implanted electrodes, to specific targets in the brain (brain nuclei) for the treatment of movement and neuropsychiatric disorders. DBS in select brain regions has provided therapeutic benefits for otherwise treatment-resistant disorders such as Parkinson's disease, essential tremor, dystonia, chronic pain, major depression, and obsessive–compulsive disorder.[1] Despite the long history of DBS,[2] its underlying principles and mechanisms are still not clear.[3][4] DBS directly changes brain activity in a controlled manner, its effects are reversible (unlike those of lesioning techniques), and it is one of only a few neurosurgical methods that allow blinded studies.[1]
The Food and Drug Administration approved DBS as a treatment for essential tremor and Parkinson's disease (PD) in 1997,[5] dystonia in 2003,[6] and obsessive–compulsive disorder (OCD) in 2009.[7] DBS is also used in research studies to treat chronic pain, PTSD,[8][9] and has been used to treat various affective disorders, including major depression; none of these applications of DBS has yet been FDA-approved. While DBS has proven to be effective for some patients, the potential for serious complications and side effects exists.
Drawing of DBS electrodes deep in the brain (side view)
Contents
1 Components and placement
2 Applications
2.1 Parkinson's disease
2.2 Chronic pain
2.3 Major depression and obsessive-compulsive disorder
2.4 Tourette syndrome
2.5 Other clinical applications
3 Adverse effects
4 Mechanisms
5 Recent developments
6 See also
7 References
8 Further reading
9 External links
Components and placement[edit source]
The DBS system consists of three components: the implanted pulse generator (IPG), the lead, and an extension. The IPG is a battery-powered neurostimulator encased in a titanium housing, which sends electrical pulses to the brain that interfere with neural activity at the target site. The lead is a coiled wire insulated in polyurethane with four platinum-iridium electrodes and is placed in one or two different nuclei of the brain. The lead is connected to the IPG by an extension, an insulated wire that runs below the skin, from the head, down the side of the neck, behind the ear, to the IPG, which is placed subcutaneously below the clavicle, or in some cases, the abdomen.[10]The IPG can be calibrated by a neurologist, nurse, or trained technician to optimize symptom suppression and control side effects.[11]
DBS leads are placed in the brain according to the type of symptoms to be addressed. For non-Parkinsonian essential tremor, the lead is placed in either the ventrointermediate nucleus of the thalamus or the zona incerta[12]; for dystonia and symptoms associated with PD (rigidity, bradykinesia/akinesia, and tremor), the lead may be placed in either the globus pallidus internus or the subthalamic nucleus; for OCD and depression to the nucleus accumbens; for incessant pain to the posterior thalamic region or periaqueductal gray; for Parkinson plus patients to two nuclei simultaneously, subthalamic nucleus and tegmental nucleus of pons, with the use of two pulse generators; and for epilepsy treatment to the anterior thalamic nucleus.[13]
All three components are surgically implanted inside the body. Lead implantation may take place under local anesthesia or with the patient under general anesthesia ("asleep DBS") such as for dystonia. A hole about 14 mm in diameter is drilled in the skull and the probe electrode is inserted stereotactically. During the awake procedure with local anesthesia, feedback from the patient is used to determine the optimal placement of the permanent electrode. During the asleep procedure, intraoperative MRI guidance is used for direct visualization of brain tissue and device.[14] The installation of the IPG and extension leads occurs under general anesthesia.[15] The right side of the brain is stimulated to address symptoms on the left side of the body and vice versa.[citation needed]
Applications[edit source]
Parkinson's disease[edit source]
Insertion of electrode during surgery using a stereotactic frame
The use of DBS as a treatment for Parkinson's Disease (PD) dates from 1987.[16] PD is a neurodegenerative diseasewhose primary symptoms are tremor, rigidity, bradykinesia, and postural instability.[17] DBS does not cure PD, but it can help manage some of its symptoms and subsequently improve the patient’s quality of life.[18] At present, the procedure is used only for patients whose symptoms cannot be adequately controlled with medications, or whose medications have severe side effects.[10] Its direct effect on the physiology of brain cells and neurotransmitters is currently debated, but by sending high-frequency electrical impulses into specific areas of the brain, it can mitigate symptoms[19] and directly diminish the side effects induced by PD medications,[20] allowing a decrease in medications, or making a medication regimen more tolerable.[citation needed]
A few sites in the brain can be targeted to achieve differing results, so patients must be assessed individually, and a site is chosen based on their needs. Traditionally, the two most common sites are the subthalamic nucleus (STN) and the globus pallidus interna, but other sites, such as the caudal zona incerta and the pallidofugal fibers medial to the STN, are being evaluated and show promise.[21]
In the United States, DBS is approved by the Food and Drug Administration for the treatment of PD.[22] DBS carries the risks of major surgery, with a complication rate related to the experience of the surgical team. The major complications include hemorrhage (1–2%) and infection (3–5%).[23]
Chronic pain[edit source]
Stimulation of the periaqueductal gray and periventricular gray for nociceptive pain, and the internal capsule, ventral posterolateral nucleus, and ventral posteromedial nucleus for neuropathic pain has produced impressive results with some patients, but results vary and appropriate patient selection is important. One study[24] of 17 patients with intractable cancer pain found that 13 were virtually pain free and only four required opioid analgesics on release from hospital after the intervention. Most ultimately did resort to opioids, usually in the last few weeks of life.[25] DBS has also been applied for phantom limb pain.[26]
Major depression and obsessive-compulsive disorder[edit source]
DBS has been used in a small number of clinical trials to treat patients suffering from a severe form of treatment-resistant depression (TRD).[27] A number of neuroanatomical targets have been used for DBS for TRD including the subgenual cingulate gyrus, posterior gyrus rectus,[28] nucleus accumbens,[29] ventral capsule/ventral striatum, inferior thalamic peduncle, and the lateral habenula.[27] A recently proposed target of DBS intervention in depression is the superolateral branch of the medial forebrain bundle; its stimulation lead to surprisingly rapid antidepressant effects in very treatment-resistant patients.[30]
The small patient numbers in the early trials of DBS for TRD currently limit the selection of an optimal neuroanatomical target.[27] Evidence is insufficient to support DBS as a therapeutic modality for depression; however, the procedure may be an effective treatment modality in the future.[31] In fact, beneficial results have been documented in the neurosurgical literature, including a few instances in which deeply depressed patients were provided with portable stimulators for self treatment.[32][33][34]
A systematic review of DBS for TRD and OCD identified 23 cases, nine for OCD, seven for TRD, and one for both. "[A]bout half the patients did show dramatic improvement" and adverse events were "generally trivial" given the younger psychiatric patient population than with movement disorders.[35] The first randomized, controlled study of DBS for the treatment of TRD targeting the ventral capsule/ventral striatum area did not demonstrate a significant difference in response rates between the active and sham groups at the end of a 16-week study.[36]
DBS for TRD can be as effective as antidepressants, with good response and remission rates, but adverse effects and safety must be more fully evaluated. Common side effects include "wound infection, perioperative headache, and worsening/irritable mood [and] increased suicidality".[37]
Tourette syndrome[edit source]
Further information: Treatment of Tourette syndrome
DBS has been used experimentally in treating adults with severe Tourette syndrome that does not respond to conventional treatment. Despite widely publicized early successes, DBS remains a highly experimental procedure for the treatment of Tourette's, and more study is needed to determine whether long-term benefits outweigh the risks.[38][39][40][41] The procedure is well tolerated, but complications include "short battery life, abrupt symptom worsening upon cessation of stimulation, hypomanic or manic conversion, and the significant time and effort involved in optimizing stimulation parameters".[42] As of 2006, five patients with TS have been reported on; all experienced reduction in tics and the disappearance of obsessive-compulsive behaviors.[42]
The procedure is invasive and expensive, and requires long-term expert care. Benefits for severe Tourette's are not conclusive, considering less robust effects of this surgery seen in the Netherlands. Tourette's is more common in pediatric populations, tending to remit in adulthood, so in general this would not be a recommended procedure for use on children. Because diagnosis of Tourette's is made based on a history of symptoms rather than analysis of neurological activity, it may not always be clear how to apply DBS for a particular patient. Due to concern over the use of DBS in Tourette syndrome treatment, the Tourette Association of America convened a group of experts to develop recommendations guiding the use and potential clinical trials of DBS for TS.[43]
Robertson reported that DBS had been used on 55 adults by 2011, remained an experimental treatment at that time, and recommended that the procedure "should only be conducted by experienced functional neurosurgeons operating in centres which also have a dedicated Tourette syndrome clinic".[39] According to Malone et al(2006), "Only patients with severe, debilitating, and treatment-refractory illness should be considered; while those with severe personality disorders and substance-abuse problems should be excluded."[42] Du et al (2010) say, "As an invasive therapy, DBS is currently only advisable for severely affected, treatment-refractory TS adults".[40] Singer (2011) says, "pending determination of patient selection criteria and the outcome of carefully controlled clinical trials, a cautious approach is recommended".[38]Viswanathan et al (2012) say DBS should be used in patients with "severe functional impairment that cannot be managed medically".[44]
Other clinical applications[edit source]
Results of DBS in dystonia patients, where positive effects often appear gradually over a period of weeks to months, indicate a role of functional reorganization in at least some cases.[45] The procedure has been tested for effectiveness in people with epilepsy that is resistant to medication.[46] DBS may reduce or eliminate epileptic seizures with programmed or responsive stimulation.[citation needed]
DBS of the septal areas of persons with schizophrenia have resulted in enhanced alertness, cooperation, and euphoria.[47] Persons with narcolepsy and complex-partial seizures also reported euphoria and sexual thoughts from self-elicited DBS of the septal nuclei.[33]
Orgasmic ecstasy was reported with the electrical stimulation of the brain with depth electrodes in the left hippocampus at 3mA, and the right hippocampus at 1 mA.[48]
Adverse effects[edit source]
While DBS is helpful for some patients, the potential also exists for neuropsychiatric side effects, including apathy, hallucinations, hypersexuality, cognitive dysfunction, depression, and euphoria. However, these may be temporary and related to correct placement of electrodes and calibration of the stimulator, so these side effects are potentially reversible.[49]
Because the brain can shift slightly during surgery, the electrodes can become displaced or dislodged from the specific location. This may cause more profound complications such as personality changes, but electrode misplacement is relatively easy to identify using CT. Also, complications of surgery may occur, such as bleeding within the brain. After surgery, swelling of the brain tissue, mild disorientation, and sleepiness are normal. After 2–4 weeks, a follow-up visit is used to remove sutures, turn on the neurostimulator, and program it.[citation needed]
As with all surgery, a risk exists of infection and bleeding during and after a surgery. The foreign object placed may be rejected by the body or calcification of the implant might take place.[medical citation needed]
Mechanisms[edit source]
The exact mechanism of action of DBS is not known.[50] A variety of hypotheses try to explain the mechanisms of DBS:[51][52]
Depolarization blockade: Electrical currents block the neuronal output at or near the electrode site.
Synaptic inhibition: This causes an indirect regulation of the neuronal output by activating axon terminals with synaptic connections to neurons near the stimulating electrode.
Desynchronization of abnormal oscillatory activity of neurons
Antidromic activation either activating/blockading distant neurons or blockading slow axons[4]
DBS represents an advance on previous treatments which involved pallidotomy (i.e., surgical ablation of the globus pallidus) or thalamotomy (i.e., surgical ablation of the thalamus).[53] Instead, a thin lead with multiple electrodes is implanted in the globus pallidus, nucleus ventralis intermedius thalami, orsubthalamic nucleus, and electric pulses are used therapeutically. The lead from the implant is extended to the neurostimulator under the skin in the chest area.[citation needed]
Recent developments[edit source]
In 2015, a group of Brazilian researchers led by neurosurgeon Dr. Erich Fonoff described a new technique that allows for simultaneous implants of electrodes called bilateral stereotactic procedure for DBS. The main benefits are less time spent on the procedure and greater accuracy.[54]
Forniceal DBS was found to improve learning and memory in a mouse model of Rett syndrome .[55]More recent work showed, that DBS upregulates genes involved in synaptic function, cell survival, and neurogenesis[56], making some first steps at explaining the restoration of hippocampal circuit function.
See also[edit source]
Brain implant
Electroconvulsive therapy
Electroencephalography
Neuromodulation (medicine)
Neuroprosthetics
Organization for Human Brain Mapping
Responsive neurostimulation device
Robert G. Heath
Stimulation cérébrale profonde (fr)
Parkinson's disease
From Wikipedia, the free encyclopedia
Jump to navigationJump to search
"Parkinson's" and "Parkinson's Disease" redirect here. For the medical journal, see Parkinson’s Disease (journal). For other uses, see Parkinson's (disambiguation).
Parkinson's disease
Synonyms Parkinson disease, idiopathic or primary parkinsonism, hypokinetic rigid syndrome, paralysis agitans, shaking palsy
Two sketches (one from the front and one from the right side) of a man, with an expressionless face. He is stooped forward and is presumably having difficulty walking.
Illustration of Parkinson's disease by William Richard Gowers, first published in A Manual of Diseases of the Nervous System (1886)
Specialty Neurology
Symptoms Shaking, rigidity, slowness of movement, difficulty walking[1]
Complications Dementia, depression, anxiety[2]
Usual onset Age over 60[1][3]
Causes Unknown[4]
Risk factors Pesticide exposure, head injuries[4]
Diagnostic method Based on symptoms[1]
Differential diagnosis Dementia with Lewy bodies, progressive supranuclear palsy, essential tremor, antipsychotic use[5]
Treatment Medications, surgery[1]
Medication L-DOPA, dopamine agonists[2]
Prognosis Life expectancy ~ 10 years[2]
Frequency 6.2 million (2015)[6]
Deaths 117,400 (2015)[7]
Parkinson's disease (PD) is a long-term degenerative disorder of the central nervous system that mainly affects the motor system.[1] As the disease worsens, non-motor symptoms become increasingly common.[1][4] The symptoms generally come on slowly over time.[1] Early in the disease, the most obvious are shaking, rigidity, slowness of movement, and difficulty with walking.[1] Thinking and behavioral problems may also occur.[2] Dementia becomes common in the advanced stages of the disease.[2] Depression and anxiety are also common, occurring in more than a third of people with PD.[2] Other symptoms include sensory, sleep, and emotional problems.[1][2] The main motor symptoms are collectively called "parkinsonism", or a "parkinsonian syndrome".[4][8]
The cause of Parkinson's disease is generally unknown, but believed to involve both genetic and environmental factors.[4] Those with a family member affected are more likely to get the disease themselves.[4] There is also an increased risk in people exposed to certain pesticides and among those who have had prior head injuries, while there is a reduced risk in tobacco smokers and those who drink coffee or tea.[4][9] The motor symptoms of the disease result from the death of cells in the substantia nigra, a region of the midbrain.[1] This results in not enough dopamine in these areas.[1] The reason for this cell death is poorly understood, but involves the build-up of proteins into Lewy bodies in the neurons.[4] Diagnosis of typical cases is mainly based on symptoms, with tests such as neuroimaging being used to rule out other diseases.[1]
There is no cure for Parkinson's disease, with treatment directed at improving symptoms.[1][10] Initial treatment is typically with the antiparkinson medication levodopa (L-DOPA), with dopamine agonists being used once levodopa becomes less effective.[2] As the disease progresses and neurons continue to be lost, these medications become less effective while at the same time they produce a complication marked by involuntary writhing movements.[2] Diet and some forms of rehabilitation have shown some effectiveness at improving symptoms.[11][12] Surgery to place microelectrodes for deep brain stimulation has been used to reduce motor symptoms in severe cases where drugs are ineffective.[1] Evidence for treatments for the non-movement-related symptoms of PD, such as sleep disturbances and emotional problems, is less strong.[4]
In 2015, PD affected 6.2 million people and resulted in about 117,400 deaths globally.[6][7] Parkinson's disease typically occurs in people over the age of 60, of which about one percent are affected.[1][3] Males are more often affected than females at a ratio of around 3:2.[4] When it is seen in people before the age of 50, it is called early-onset PD.[13] The average life expectancy following diagnosis is between 7 and 14 years.[2] The disease is named after the English doctor James Parkinson, who published the first detailed description in An Essay on the Shaking Palsy, in 1817.[14][15] Public awareness campaigns include World Parkinson's Day (on the birthday of James Parkinson, 11 April) and the use of a red tulip as the symbol of the disease.[16] People with Parkinson's who have increased the public's awareness of the condition include actor Michael J. Fox, Olympic cyclist Davis Phinney, and professional boxer Muhammad Ali.[17][18][19]
Contents
1 Classification
2 Signs and symptoms
2.1 Motor
2.2 Neuropsychiatric
2.3 Other
3 Causes
3.1 Environmental factors
3.2 Genetics
4 Pathophysiology
4.1 Brain cell death
5 Diagnosis
5.1 Imaging
5.2 Differential diagnosis
6 Prevention
7 Management
7.1 Medications
7.2 Surgery
7.3 Rehabilitation
7.4 Palliative care
8 Prognosis
9 Epidemiology
10 History
11 Society and culture
11.1 Cost
11.2 Advocacy
11.3 Notable cases
12 Research
12.1 Animal models
12.2 Gene therapy
12.3 Neuroprotective treatments
12.4 Cell-based therapies
12.5 Other
13 References
14 External links
Classification
The movement difficulties found in PD are called parkinsonism and a number of different disorders feature parkinsonism. "Parkinsonism" is defined as bradykinesia (slowness in initiating voluntary movements, with progressive reduction in speed and range of repetitive actions such as voluntary finger-tapping[20]) in combination with one of three other physical signs: muscular (lead-pipe or cogwheel) rigidity, tremor at rest, and postural instability.[21][22]
Parkinson's disease is the most common form of parkinsonism and is sometimes called "idiopathic parkinsonism", meaning parkinsonism with no identifiable cause.[10][23] Identifiable causes of parkinsonism include toxins, infections, side effects of drugs, metabolic derangement, and brain lesions such as strokes. Several neurodegenerative disorders also may present with parkinsonism and are sometimes referred to as "atypical parkinsonism" or "Parkinson plus" syndromes (illnesses with parkinsonism plus some other features distinguishing them from PD). They include multiple system atrophy, progressive supranuclear palsy, corticobasal degeneration, and dementia with Lewy bodies (DLB).[10][24]
Scientists sometimes refer to Parkinson’s disease as a synucleinopathy (due to an abnormal accumulation of alpha-synuclein protein in the brain) to distinguish it from other neurodegenerative diseases, such as Alzheimer's disease where the brain accumulates tau protein.[25] Considerable clinical and pathological overlap exists between tauopathies and synucleinopathies. In contrast to Parkinson's disease, Alzheimer's disease presents most commonly with memory loss, and the cardinal signs of Parkinson's disease (slowness, tremor, stiffness, and postural instability) are not normal features of Alzheimer's.
Dementia with Lewy bodies is another synucleinopathy and it has close pathological similarities with PD, especially with the subset of PD cases with dementia known as Parkinson's disease dementia. The relationship between PD and DLB is complex and incompletely understood.[26] They may represent parts of a continuum with variable distinguishing clinical and pathological features or they may prove to be separate diseases.[26]
Signs and symptoms
Black and white picture of a male with PD stooping forward as he walks. He is viewed from the left side and there is a chair behind him.
A man with Parkinson's disease displaying a flexed walking posture pictured in 1892[27]
French signature reads "Catherine Metzger 13 Octobre 1869"
Handwriting of a person affected by PD[28]
Main article: Signs and symptoms of Parkinson's disease
The most recognizable symptoms in Parkinson's disease are movement ("motor") related.[29] Non-motor symptoms, which include autonomic dysfunction, neuropsychiatric problems (mood, cognition, behavior or thought alterations), and sensory (especially altered sense of smell) and sleep difficulties, are also common. Some of these non-motor symptoms may be present at the time of diagnosis.[29]
Motor
Further information: Parkinsonian gait
Four motor symptoms are considered cardinal in PD: tremor, slowness of movement (bradykinesia), rigidity, and postural instability.[29]
The most common presenting sign is a coarse slow tremor of the hand at rest which disappears during voluntary movement of the affected arm and in the deeper stages of sleep.[29] It typically appears in only one hand, eventually affecting both hands as the disease progresses.[29] Frequency of PD tremor is between 4 and 6 hertz (cycles per second). A feature of tremor is pill-rolling, the tendency of the index finger and thumb to touch and perform together a circular movement.[29][30] The term derives from the similarity between the movement of people with PD and the early pharmaceutical technique of manually making pills.[30]
Bradykinesia (slowness of movement) is found in every case of PD, and is due to disturbances in motor planning of movement initiation, and associated with difficulties along the whole course of the movement process, from planning to initiation to execution of a movement. Performance of sequential and simultaneous movement is impaired. Bradykinesia is the most handicapping symptom of Parkinson’s disease leading to difficulties with everyday tasks such as dressing, feeding, and bathing. It leads to particular difficulty in carrying out two independent motor activities at the same time and can be made worse by emotional stress or concurrent illnesses. Paradoxically patients with Parkinson's disease can often ride a bicycle or climb stairs more easily than walk on a level. While most physicians may readily notice bradykinesia, formal assessment requires a patient to do repetitive movements with their fingers and feet.[31]
Rigidity is stiffness and resistance to limb movement caused by increased muscle tone, an excessive and continuous contraction of muscles.[29] In parkinsonism the rigidity can be uniform ("lead-pipe rigidity") or ratchety ("cogwheel rigidity").[10][29][32][33] The combination of tremor and increased tone is considered to be at the origin of cogwheel rigidity.[34] Rigidity may be associated with joint pain; such pain being a frequent initial manifestation of the disease.[29] In early stages of Parkinson's disease, rigidity is often asymmetrical and it tends to affect the neck and shoulder muscles prior to the muscles of the face and extremities.[35] With the progression of the disease, rigidity typically affects the whole body and reduces the ability to move.
Postural instability is typical in the later stages of the disease, leading to impaired balance and frequent falls,[36] and secondarily to bone fractures, loss of confidence, and reduced mobility.[37] Instability is often absent in the initial stages, especially in younger people, especially prior to the development of bilateral symptoms.[38] Up to 40% of people diagnosed with PD may experience falls and around 10% may have falls weekly, with the number of falls being related to the severity of PD.[29]
Other recognized motor signs and symptoms include gait and posture disturbances such as festination (rapid shuffling steps and a forward-flexed posture when walking with no flexed arm swing). Freezing of gait (brief arrests when the feet seem to get stuck to the floor, especially on turning or changing direction), a slurred monotonous quiet voice, mask-like facial expression, and handwriting that gets smaller and smaller are other common signs.[39]
Neuropsychiatric
Parkinson's disease can cause neuropsychiatric disturbances, which can range from mild to severe. This includes disorders of cognition, mood, behavior, and thought.[29]
Cognitive disturbances can occur in the early stages of the disease and sometimes prior to diagnosis, and increase in prevalence with duration of the disease.[29][40] The most common cognitive deficit in PD is executive dysfunction, which can include problems with planning, cognitive flexibility, abstract thinking, rule acquisition, inhibiting inappropriate actions, initiating appropriate actions, working memory, and control of attention.[40][41] Other cognitive difficulties include slowed cognitive processing speed, impaired recall and impaired perception and estimation of time.[40][41] Nevertheless, improvement appears when recall is aided by cues.[40] Visuospatial difficulties are also part of the disease, seen for example when the individual is asked to perform tests of facial recognition and perception of the orientation of drawn lines.[40][41]
A person with PD has two to six times the risk of dementia compared to the general population.[29][40] Up to 78% of people with PD have Parkinson's disease dementia.[42] The prevalence of dementia increases with age and, to a lesser degree, duration of the disease.[43] Dementia is associated with a reduced quality of life in people with PD and their caregivers, increased mortality, and a higher probability of needing nursing home care.[40]
Impulse control disorders including pathological gambling, compulsive sexual behavior, binge eating, compulsive shopping and reckless generosity can be caused by medication, particularly orally active dopamine agonists. The dopamine dysregulation syndrome – with wanting of medication leading to overusage – is a rare complication of levodopa use.[44]
Behavior and mood alterations are more common in PD without cognitive impairment than in the general population, and are usually present in PD with dementia. The most frequent mood difficulties are depression, apathy, and anxiety.[29] Establishing the diagnosis of depression is complicated by the fact that the body language of depression may masquerade as PD including a sad expressionless anxious face, a hang dog appearance, slow movement, and monotonous speech. Up to 30% of people with PD may experience symptoms of anxiety, ranging from a generalized anxiety disorder to social phobia, panic disorders and obsessive compulsive disorders. They contribute to impaired quality of life and increased severity of motor symptoms such as on/off fluctuations or freezing episodes.
Punding in which complicated repetitive aimless stereotyped behaviors occur for many hours is another disturbance caused by anti-Parkinson medication.
Hallucinations or delusions occur in approximately 50% of people with PD over the course of the illness, and may herald the emergence of dementia. These range from minor hallucinations – "sense of passage" (something quickly passing beside the person) or "sense of presence" (the perception of something/someone standing just to the side or behind the person) – to full blown vivid, formed visual hallucinations and paranoid ideation. Auditory hallucinations are uncommon in PD, and are rarely described as voices. It is now believed that psychosis is an integral part of the disease. A psychosis with delusions and associated delirium is a recognized complication of anti-Parkinson drug treatment and may also be caused by urinary tract infections (as frequently occurs in the fragile elderly), but drugs and infection are not the only factors, and underlying brain pathology or changes in neurotransmitters or their receptors (e.g., acetylcholine, serotonin) are also thought to play a role in psychosis in PD.[45][46]
Other
In addition to neuropsychiatric and motor symptoms, PD can impair other functions.
Sleep disorders are a feature of the disease and can be worsened by medications.[29] Symptoms can manifest as daytime drowsiness (including sudden sleep attacks resembling narcolepsy), disturbances in REM sleep, or insomnia.[29] REM behavior disorder (RBD), in which patients act out dreams, sometimes injuring themselves or their bed partner, may begin many years before the development of motor or cognitive features of PD or DLB.[47]
Alterations in the autonomic nervous system can lead to orthostatic hypotension (low blood pressure upon standing), oily skin and excessive sweating, urinary incontinence, and altered sexual function.[29] Constipation and impaired stomach emptying (gastric dysmotility) can be severe enough to cause discomfort and even endanger health.[11] Changes in perception may include an impaired sense of smell, disturbed vision, pain, and paresthesia (tingling and numbness).[29] All of these symptoms can occur years before diagnosis of the disease.[29]
Causes
Main article: Causes of Parkinson's disease
Environmental factors
Exposure to pesticides and a history of head injury have each been linked with Parkinson disease (PD), but the risks are modest. Never having smoked cigarettes, and never drinking caffeinated beverages, are also associated with small increases in risk of developing PD.[44]
Low concentrations of urate in the blood serum is associated with an increased risk of PD.[48]
Genetics
Parkin crystal structure
Research indicates that PD is the product of a complex interaction of genetic and environmental factors.[4] Around 15% of individuals with PD have a first-degree relative who has the disease,[10] and 5–10% of people with PD are known to have forms of the disease that occur because of a mutation in one of several specific genes.[49] Harboring one of these gene mutations may not lead to the disease; susceptibility factors put the individual at an increased risk, often in combination with other risk factors, which also affect age of onset, severity and progression.[49]
Genes implicated in the development of PD include SNCA, LRRK2, GBA, PRKN, PINK1, PARK7, VPS35, EIF4G1, DNAJC13 and CHCHD2.[50]
About 5% of people with PD have mutations in the GBA1 gene.[51] These muations are present in < 1% of the unaffected population. The risk of developing PD is increased 20-30 fold if these muations are present. PD associated with these mutations has the same clinical features but an earlier age of onset and a more rapid cognitive and motor decline.
SNCA gene mutations are important in PD because the protein which this gene encodes, alpha-synuclein, is the main component of the Lewy bodies that accumulate in the brains of people with PD.[49] Mutations in some genes, including SNCA, LRRK2 and GBA, have been found to be risk factors for "sporadic" (non-familial) PD.[49] Mutations in the gene LRRK2 are the most common known cause of familial and sporadic PD, accounting for approximately 5% of individuals with a family history of the disease and 3% of sporadic cases.[52][49] A mutation in GBA presents the greatest genetic risk of developing Parkinsons disease.[50]
Several Parkinson-related genes are involved in the function of lysosomes, organelles that digest cellular waste products. It has been suggested that some cases of PD may be caused by lysosomal disorders that reduce the ability of cells to break down alpha-synuclein.[53]
Pathophysiology
Several brain cells stained in blue. The largest one, a neurone, with an approximately circular form, has a brown circular body inside it. The brown body is about 40% the diameter of the cell in which it appears.
A Lewy body (stained brown) in a brain cell of the substantia nigra in Parkinson's disease. The brown colour is positive immunohistochemistry staining for alpha-synuclein.
Main article: Pathophysiology of Parkinson's disease
The main pathological characteristics of PD are cell death in the brain's basal ganglia (affecting up to 70% of the dopamine secreting neurons in the substantia nigra pars compacta by the end of life)[52] and the presence of Lewy bodies (accumulations of the protein alpha-synuclein) in many of the remaining neurons. This loss of neurons is accompanied by the death of astrocytes (star-shaped glial cells) and a significant increase in the number of microglia (another type of glial cell) in the substantia nigra.[54]
Composite of three images, one in top row (referred to in caption as A), two in second row (referred to as B). Top shows a mid-line sagittal plane of the brainstem and cerebellum. There are three circles superimposed along the brainstem and an arrow linking them from bottom to top and continuing upward and forward towards the frontal lobes of the brain. A line of text accompanies each circle: lower is "1. Dorsal Motor X Nucleus", middle is "2. Gain Setting Nuclei" and upper is "3. Substantia Nigra/Amygdala". The fourth line of text above the others says "4. ...". The two images at the bottom of the composite are magnetic resonance imaging (MRI) scans, one sagittal and the other transverse, centred at the same brain coordinates (x=-1, y=-36, z=-49). A colored blob marking volume reduction covers most of the brainstem.
Schematic initial progression of Lewy body deposits in the first stages of Parkinson's disease, as proposed by Braak and colleagues
Localization of the area of significant brain volume reduction in initial PD compared with a group of participants without the disease in a neuroimaging study, which concluded that brainstem damage may be the first identifiable stage of PD neuropathology[55]
There are five major pathways in the brain connecting other brain areas with the basal ganglia. These are known as the motor, oculo-motor, associative, limbic and orbitofrontal circuits, with names indicating the main projection area of each circuit.[56] All of them are affected in PD, and their disruption explains many of the symptoms of the disease, since these circuits are involved in a wide variety of functions, including movement, attention and learning.[56] Scientifically, the motor circuit has been examined the most intensively.[56]
A particular conceptual model of the motor circuit and its alteration with PD has been of great influence since 1980, although some limitations have been pointed out which have led to modifications.[56] In this model, the basal ganglia normally exert a constant inhibitory influence on a wide range of motor systems, preventing them from becoming active at inappropriate times. When a decision is made to perform a particular action, inhibition is reduced for the required motor system, thereby releasing it for activation. Dopamine acts to facilitate this release of inhibition, so high levels of dopamine function tend to promote motor activity, while low levels of dopamine function, such as occur in PD, demand greater exertions of effort for any given movement. Thus, the net effect of dopamine depletion is to produce hypokinesia, an overall reduction in motor output.[56] Drugs that are used to treat PD, conversely, may produce excessive dopamine activity, allowing motor systems to be activated at inappropriate times and thereby producing dyskinesias.[56]
Brain cell death
There is speculation of several mechanisms by which the brain cells could be lost.[57] One mechanism consists of an abnormal accumulation of the protein alpha-synuclein bound to ubiquitin in the damaged cells. This insoluble protein accumulates inside neurones forming inclusions called Lewy bodies.[52][58] According to the Braak staging, a classification of the disease based on pathological findings proposed by Heiko Braak, Lewy bodies first appear in the olfactory bulb, medulla oblongata and pontine tegmentum; individuals at this stage may be asymptomatic or may have early non-motor symptoms (such as loss of sense of smell, or some sleep or automatic dysfunction). As the disease progresses, Lewy bodies develop in the substantia nigra, areas of the midbrain and basal forebrain and, finally, the neocortex.[52] These brain sites are the main places of neuronal degeneration in PD; however, Lewy bodies may not cause cell death and they may be protective (with the abnormal protein sequestered or walled off). Other forms of alpha-synuclein (e.g., oligomers) that are not aggregated in Lewy bodies and Lewy neurites may actually be the toxic forms of the protein.[57][58] In people with dementia, a generalized presence of Lewy bodies is common in cortical areas. Neurofibrillary tangles and senile plaques, characteristic of Alzheimer's disease, are not common unless the person is demented.[54]
Other cell-death mechanisms include proteasomal and lysosomal system dysfunction and reduced mitochondrial activity.[57][59] Iron accumulation in the substantia nigra is typically observed in conjunction with the protein inclusions. It may be related to oxidative stress, protein aggregation and neuronal death, but the mechanisms are not fully understood.[60]
Diagnosis
A physician will initially assess for Parkinson's disease with a careful medical history and neurological examination.[29] People may be given levodopa, with any resulting improvement in motor impairment helping to confirm the PD diagnosis. The finding of Lewy bodies in the midbrain on autopsy is usually considered final proof that the person had PD. The clinical course of the illness over time may reveal it is not Parkinson's disease, requiring that the clinical presentation be periodically reviewed to confirm accuracy of the diagnosis.[29][61]
Other causes that can secondarily produce parkinsonism are stroke and drugs.[61] Parkinson plus syndromes such as progressive supranuclear palsy and multiple system atrophy must be ruled out.[29] Anti-Parkinson's medications are typically less effective at controlling symptoms in Parkinson plus syndromes.[29] Faster progression rates, early cognitive dysfunction or postural instability, minimal tremor or symmetry at onset may indicate a Parkinson plus disease rather than PD itself.[62] Genetic forms with an autosomal dominant or recessive pattern of inheritance are sometimes referred to as familial Parkinson's disease or familial parkinsonism.[10]
Medical organizations have created diagnostic criteria to ease and standardize the diagnostic process, especially in the early stages of the disease. The most widely known criteria come from the UK Queen Square Brain Bank for Neurological Disorders and the U.S. National Institute of Neurological Disorders and Stroke. The Queen Square Brain Bank criteria require slowness of movement (bradykinesia) plus either rigidity, resting tremor, or postural instability. Other possible causes of these symptoms need to be ruled out. Finally, three or more of the following supportive features are required during onset or evolution: unilateral onset, tremor at rest, progression in time, asymmetry of motor symptoms, response to levodopa for at least five years, clinical course of at least ten years and appearance of dyskinesias induced by the intake of excessive levodopa.[63]
When PD diagnoses are checked by autopsy, movement disorders experts are found on average to be 79.6% accurate at initial assessment and 83.9% accurate after they have refined their diagnosis at a follow-up examination. When clinical diagnoses performed mainly by nonexperts are checked by autopsy, average accuracy is 73.8%. Overall, 80.6% of PD diagnoses are accurate, and 82.7% of diagnoses using the Brain Bank criteria are accurate.[64]
A task force of the International Parkinson and Movement Disorder Society (MDS) has proposed diagnostic criteria for Parkinson’s disease as well as research criteria for the diagnosis of prodromal disease, but these will require validation against the more established criteria.[65][66]
Imaging
Computed tomography (CT) scans of people with PD usually appear normal.[67] MRI has become more accurate in diagnosis of the disease over time, specifically through iron-sensitive T2* and SWI sequences at a magnetic field strength of at least 3T, both of which can demonstrate absence of the characteristic 'swallow tail' imaging pattern in the dorsolateral substantia nigra.[68] In a meta-analysis, absence of this pattern was highly sensitive and specific for the disease.[69] Diffusion MRI has shown potential in distinguishing between PD and Parkinson plus syndromes, though its diagnostic value is still under investigation.[67] CT and MRI are also used to rule out other diseases that can be secondary causes of parkinsonism, most commonly encephalitis and chronic ischemic insults, as well as less frequent entities such as basal ganglia tumors and hydrocephalus.[67]
The metabolic activity of dopamine transporters in the basal ganglia can be directly measured with PET and SPECT scans, with the DaTSCAN being a common proprietary version of this study. It has shown high agreement with clinical diagnoses of Parkinson's.[70] Reduced dopamine-related activity in the basal ganglia can help exclude drug-induced Parkinsonism. This finding is not entirely specific, however, and can be seen with both PD and Parkinson-plus disorders.[67] In the United States, DaTSCANs are only FDA approved to distinguish Parkinson’s disease or Parkinsonian syndromes from essential tremor.[71]
Differential diagnosis
Other conditions that can have similar presentations to PD include:[72]
Arthritis
Corticobasal syndrome
Dementia with Lewy bodies
Depression
Drug induced parkinsonism
Fragile X-associated tremor/ataxia syndrome
Frontotemporal dementia and parkinsonism linked to chromosome 17
Huntington’s disease
Idiopathic basal ganglia calcification
Multiple system atrophy
Neurodegeneration with brain iron accumulation
Normal-pressure hydrocephalus
Obsessional slowness
Progressive supranuclear palsy
Psychogenic parkinsonism
Toxins
Wilson’s disease
Vascular parkinsonism
Prevention
Exercise in middle age may reduce the risk of Parkinson's disease later in life.[12] Caffeine also appears protective with a greater decrease in risk occurring with a larger intake of caffeinated beverages such as coffee.[73] People who smoke cigarettes or use smokeless tobacco are less likely than non-smokers to develop PD, and the more they have used tobacco, the less likely they are to develop PD. It is not known what underlies this effect. Tobacco use may actually protect against PD, or it may be that an unknown factor both increases the risk of PD and causes an aversion to tobacco or makes it easier to quit using tobacco.[74]
Antioxidants, such as vitamins C and E, have been proposed to protect against the disease, but results of studies have been contradictory and no positive effect has been proven.[75] The results regarding fat and fatty acids have been contradictory, with various studies reporting protective effects, risk-increasing effects or no effects.[75] There have been preliminary indications that the use of anti-inflammatory drugs and calcium channel blockers may be protective.[4] A 2010 meta-analysis found that nonsteroidal anti-inflammatory drugs (apart from aspirin), have been associated with at least a 15 percent (higher in long-term and regular users) reduction of incidence of the development of Parkinson's disease.[76]
Management
Main article: Management of Parkinson's disease
Pharmacological treatment of Parkinson's disease
There is no cure for Parkinson's disease, but medications, surgery, and physical treatment can provide relief and are much more effective than treatments available for other neurological disorders like Alzheimer’s disease, motor neuron disease, and Parkinson plus syndromes. The main families of drugs useful for treating motor symptoms are levodopa (always combined with a dopa decarboxylase inhibitor and sometimes also with a COMT inhibitor), dopamine agonists and MAO-B inhibitors. The stage of the disease and the age at disease onset determine which group is most useful.[77]
Braak staging of Parkinson's disease gives six stages, that can be used to identify early stages, later stages, and late stages. The initial stage in which some disability has already developed and requires pharmacological treatment is followed by later stages associated with the development of complications related to levodopa usage, and a third stage when symptoms unrelated to dopamine deficiency or levodopa treatment may predominate.[78]
Treatment in the first stage aims for an optimal trade-off between symptom control and treatment side-effects. The start of levodopa treatment may be postponed by initially using other medications such as MAO-B inhibitors and dopamine agonists instead, in the hope of delaying the onset of complications due to levodopa use.[79] However, levodopa is still the most effective treatment for the motor symptoms of PD and should not be delayed in patients when their quality of life is impaired. Levodopa-related dyskinesias correlate more strongly with duration and severity of the disease than duration of levodopa treatment, so delaying this therapy may not provide much longer dyskinesia-free time than early use.[80]
In later stages the aim is to reduce PD symptoms while controlling fluctuations in the effect of the medication. Sudden withdrawals from medication or its overuse have to be managed.[79] When oral medications are not enough to control symptoms, surgery, deep brain stimulation, subcutaneous waking day apomorphine infusion and enteral dopa pumps can be of use.[81]Late stage PD presents many challenges requiring a variety of treatments including those for psychiatric symptoms particularly depression, orthostatic hypotension, bladder dysfunction and erectile dysfunction.[81] In the final stages of the disease, palliative care is provided to improve quality of life.[82]
Medications
Levodopa
The motor symptoms of PD are the result of reduced dopamine production in the brain's basal ganglia. Dopamine does not cross the blood-brain barrier, so it cannot be taken as a medicine to boost the brain's depleted levels of dopamine. However a precursor of dopamine, levodopa, can pass through to the brain where it is readily converted to dopamine, and administration of levodopa temporarily diminishes the motor symptoms of PD. Levodopa has been the most widely used PD treatment for over 40 years.[79]
Only 5–10% of levodopa crosses the blood–brain barrier. Much of the remainder is metabolized to dopamine elsewhere in the body, causing a variety of side effects including nausea, vomiting and orthostatic hypotension.[83] Carbidopa and benserazide are dopa decarboxylase inhibitors which do not cross the blood-brain barrier and inhibit the conversion of levodopa to dopamine outside the brain, reducing side effects and improving the availability of levodopa for passage into the brain. One of these drugs is usually taken along with levodopa, often combined with levodopa in the same pill.[84]
Levodopa-use leads in the long term to the development of complications: involuntary movements called dyskinesias, and fluctuations in the effectiveness of the medication.[79] When fluctuations occur, a person can cycle through phases with good response to medication and reduced PD symptoms ("on" state), and phases with poor response to medication and significant PD symptoms ("off" state).[79] Using lower doses of levodopa may reduce the risk and severity of these levodopa-induced complications.[85] A former strategy to reduce levodopa-related dyskinesia and fluctuations was to withdraw levodopa medication for some time. This is now discouraged since it can bring on dangerous side effects such as neuroleptic malignant syndrome.[79] Most people with PD will eventually need levodopa and will later develop levodopa-induced fluctuations and dyskinesias.[79]
There are controlled-release versions of levodopa. Older controlled-release levodopa preparations have poor and unreliable absorption and bioavailability and have not demonstrated improved control of PD motor symptoms or a reduction in levodopa-related complications when compared to immediate release preparations. A newer extended-release levodopa preparation does seem to be more effective in reducing fluctuations but in many patients problems persist. Intestinal infusions of levodopa (Duodopa) can result in striking improvements in fluctuations compared to oral levodopa when the fluctuations are due to insufficient uptake caused by gastroparesis. Other oral, longer acting formulations are under study and other modes of delivery (inhaled, transdermal) are being developed.[84]
COMT inhibitors
Tolcapone inhibits the activity COMT, an enzyme which degrades dopamine.[79] It has been used to complement levodopa; however, its usefulness is limited by possible complications such as liver damage.[79] A similarly effective drug, entacapone, has not been shown to cause significant alterations of liver function.[79] Licensed preparations of entacapone contain entacapone alone or in combination with carbidopa and levodopa.[79]
Dopamine agonists
Several dopamine agonists that bind to dopamine receptors in the brain have similar effects to levodopa.[79] These were initially used as a complementary therapy to levodopa for individuals experiencing levodopa complications (on-off fluctuations and dyskinesias); they are now mainly used on their own as first therapy for the motor symptoms of PD with the aim of delaying the initiation of levodopa therapy and so delaying the onset of levodopa's complications.[79][86] Dopamine agonists include bromocriptine, pergolide, pramipexole, ropinirole, piribedil, cabergoline, apomorphine and lisuride.
Though dopamine agonists are less effective than levodopa at controlling PD motor symptoms, they are usually effective enough to manage these symptoms in the first years of treatment.[10] Dyskinesias due to dopamine agonists are rare in younger people who have PD but, along with other complications, become more common with older age at onset.[10] Thus dopamine agonists are the preferred initial treatment for younger onset PD, and levodopa is preferred for older onset PD.[10]
Dopamine agonists produce significant, although usually mild, side effects including drowsiness, hallucinations, insomnia, nausea, and constipation.[79] Sometimes side effects appear even at a minimal clinically effective dose, leading the physician to search for a different drug.[79] Agonists have been related to impulse control disorders (such as compulsive sexual activity, eating, gambling and shopping) even more strongly than levodopa.[87] They tend to be more expensive than levodopa.[10]
Apomorphine, a non-orally administered dopamine agonist, may be used to reduce off periods and dyskinesia in late PD.[79] It is administered by intermittent injections or continuous subcutaneous infusions.[79] Since secondary effects such as confusion and hallucinations are common, individuals receiving apomorphine treatment should be closely monitored.[79] Two dopamine agonists that are administered through skin patches (lisuride and rotigotine) and are useful for people in the initial stages and possibly to control off states in those in the advanced state.[88]
MAO-B inhibitors
MAO-B inhibitors (safinamide, selegiline and rasagiline) increase the amount of dopamine in the basal ganglia by inhibiting the activity of monoamine oxidase B (MAO-B), an enzyme which breaks down dopamine.[79] Like dopamine agonists, their use may delay the commencement of levodopa therapy in early disease, but MAO-B inhibitors produce more adverse effects and are less effective than levodopa at controlling PD motor symptoms. There are few studies of their effectiveness in the advanced stage, although results suggest that they are useful to reduce fluctuations between on and off periods.[79] An initial study indicated that selegiline in combination with levodopa increased the risk of death, but this was later disproven.[79]
Other drugs
Main article: Antiparkinson medication
Other drugs such as amantadine and anticholinergics may be useful as treatment of motor symptoms. However, the evidence supporting them lacks quality, so they are not first choice treatments.[79] In addition to motor symptoms, PD is accompanied by a diverse range of symptoms. A number of drugs have been used to treat some of these problems.[89] Examples are the use of quetiapine for psychosis, cholinesterase inhibitors for dementia, and modafinil for daytime sleepiness.[89][90] In 2016 pimavanserin was approved for the management of Parkinson's disease psychosis.[91]
Doxepin and rasagline may reduce physical fatigue in PD.[92]
Surgery
Placement of an electrode into the brain. The head is stabilised in a frame for stereotactic surgery.
Treating motor symptoms with surgery was once a common practice, but since the discovery of levodopa, the number of operations has declined.[93] Studies in the past few decades have led to great improvements in surgical techniques, so that surgery is again being used in people with advanced PD for whom drug therapy is no longer sufficient.[93] Surgery for PD can be divided in two main groups: lesional and deep brain stimulation (DBS). Target areas for DBS or lesions include the thalamus, the globus pallidus or the subthalamic nucleus.[93] Deep brain stimulation is the most commonly used surgical treatment, developed in the 1980s by Alim Louis Benabid and others. It involves the implantation of a medical device called a neurostimulator, which sends electrical impulses to specific parts of the brain. DBS is recommended for people who have PD with motor fluctuations and tremor inadequately controlled by medication, or to those who are intolerant to medication, as long as they do not have severe neuropsychiatric problems.[94] Other, less common, surgical therapies involve intentional formation of lesions to suppress overactivity of specific subcortical areas. For example, pallidotomy involves surgical destruction of the globus pallidus to control dyskinesia.[93]
Fours areas of the brain have been treated with neural stimulators in PD.[95] These are the globus pallidus interna, thalamus, subthalamic nucleus and the pedunculopontine nucleus. DBS of the globus pallidus interna improves motor function while DBS of the thalamic DBS improves tremor but has little effect on bradykinesia or rigidity. DBS of the subthalamic nucleus is usually avoided if a history of depression or neurocognitive impairment is present. DBS of the subthalamic nucleus is associated with reduction in medication. Pedunculopontine nucleus DBS remains experimental at present. Generally DBS is associated with 30–60% improvement in motor score evaluations.
Rehabilitation
Further information: Rehabilitation in Parkinson's disease
Exercise programs are recommended in people with Parkinson's disease.[12] There is some evidence that speech or mobility problems can improve with rehabilitation, although studies are scarce and of low quality.[96][97] Regular physical exercise with or without physical therapy can be beneficial to maintain and improve mobility, flexibility, strength, gait speed, and quality of life.[97] When an exercise program is performed under the supervision of a physiotherapist, there are more improvements in motor symptoms, mental and emotional functions, daily living activities, and quality of life compared to a self-supervised exercise program at home.[98] In terms of improving flexibility and range of motion for people experiencing rigidity, generalized relaxation techniques such as gentle rocking have been found to decrease excessive muscle tension. Other effective techniques to promote relaxation include slow rotational movements of the extremities and trunk, rhythmic initiation, diaphragmatic breathing, and meditation techniques.[99] As for gait and addressing the challenges associated with the disease such as hypokinesia (slowness of movement), shuffling and decreased arm swing; physiotherapists have a variety of strategies to improve functional mobility and safety. Areas of interest with respect to gait during rehabilitation programs focus on, but are not limited to improving gait speed, the base of support, stride length, trunk and arm swing movement. Strategies include utilizing assistive equipment (pole walking and treadmill walking), verbal cueing (manual, visual and auditory), exercises (marching and PNF patterns) and altering environments (surfaces, inputs, open vs. closed).[100] Strengthening exercises have shown improvements in strength and motor function for people with primary muscular weakness and weakness related to inactivity with mild to moderate Parkinson's disease. However, reports show a significant interaction between strength and the time the medications was taken. Therefore, it is recommended that people with PD should perform exercises 45 minutes to one hour after medications when they are at their best.[101] Also, due to the forward flexed posture, and respiratory dysfunctions in advanced Parkinson's disease, deep diaphragmatic breathing exercises are beneficial in improving chest wall mobility and vital capacity.[102] Exercise may improve constipation.[11] It is unclear if exercise reduces physical fatigue in PD.[92]
One of the most widely practiced treatments for speech disorders associated with Parkinson's disease is the Lee Silverman voice treatment (LSVT).[96][103] Speech therapy and specifically LSVT may improve speech.[96] Occupational therapy (OT) aims to promote health and quality of life by helping people with the disease to participate in as many of their daily living activities as possible.[96] There have been few studies on the effectiveness of OT and their quality is poor, although there is some indication that it may improve motor skills and quality of life for the duration of the therapy.[96][104]
Palliative care
Palliative care is specialized medical care for people with serious illnesses, including Parkinson's. The goal of this speciality is to improve quality of life for both the person with Parkinson's and the family by providing relief from the symptoms, pain, and stress of illnesses.[105] As Parkinson's is not a curable disease, all treatments are focused on slowing decline and improving quality of life, and are therefore palliative in nature.[106]
Palliative care should be involved earlier, rather than later in the disease course.[107][108] Palliative care specialists can help with physical symptoms, emotional factors such as loss of function and jobs, depression, fear, and existential concerns.[107][108][109]
Along with offering emotional support to both the patient and family, palliative care serves an important role in addressing goals of care. People with Parkinson's may have many difficult decisions to make as the disease progresses such as wishes for feeding tube, non-invasive ventilator, and tracheostomy; wishes for or against cardiopulmonary resuscitation; and when to use hospice care.[106] Palliative care team members can help answer questions and guide people with Parkinson's on these complex and emotional topics to help them make the best decision based on their own values.[108][110]
Muscles and nerves that control the digestive process may be affected by PD, resulting in constipation and gastroparesis (food remaining in the stomach for a longer period than normal).[11] A balanced diet, based on periodical nutritional assessments, is recommended and should be designed to avoid weight loss or gain and minimize consequences of gastrointestinal dysfunction.[11] As the disease advances, swallowing difficulties (dysphagia) may appear. In such cases it may be helpful to use thickening agents for liquid intake and an upright posture when eating, both measures reducing the risk of choking. Gastrostomy to deliver food directly into the stomach is possible in severe cases.[11]
Levodopa and proteins use the same transportation system in the intestine and the blood–brain barrier, thereby competing for access.[11] When they are taken together, this results in a reduced effectiveness of the drug.[11] Therefore, when levodopa is introduced, excessive protein consumption is discouraged and well balanced Mediterranean diet is recommended. In advanced stages, additional intake of low-protein products such as bread or pasta is recommended for similar reasons.[11] To minimize interaction with proteins, levodopa should be taken 30 minutes before meals.[11] At the same time, regimens for PD restrict proteins during breakfast and lunch, allowing protein intake in the evening.[11]
Prognosis
See also: Unified Parkinson's disease rating scale
Global burden of Parkinson's disease, measured in disability-adjusted life years per 100,000 inhabitants in 2004
no data
< 5
5–12.5
12.5–20
20–27.5
27.5–35
35–42.5
42.5–50
50–57.5
57.5–65
65–72.5
72.5–80
> 80
PD invariably progresses with time. A severity rating method known as the Unified Parkinson's disease rating scale (UPDRS) is the most commonly used metric for clinical study. A modified version known as the MDS-UPDRS is also sometimes used. An older scaling method known as the Hoehn and Yahr scale (originally published in 1967), and a similar scale known as the Modified Hoehn and Yahr scale, have also been commonly used. The Hoehn and Yahr scale defines five basic stages of progression.
Motor symptoms, if not treated, advance aggressively in the early stages of the disease and more slowly later. Untreated, individuals are expected to lose independent ambulation after an average of eight years and be bedridden after ten years.[111] However, it is uncommon to find untreated people nowadays. Medication has improved the prognosis of motor symptoms, while at the same time it is a new source of disability, because of the undesired effects of levodopa after years of use.[111] In people taking levodopa, the progression time of symptoms to a stage of high dependency from caregivers may be over 15 years.[111] However, it is hard to predict what course the disease will take for a given individual.[111] Age is the best predictor of disease progression.[57] The rate of motor decline is greater in those with less impairment at the time of diagnosis, while cognitive impairment is more frequent in those who are over 70 years of age at symptom onset.[57]
Since current therapies improve motor symptoms, disability at present is mainly related to non-motor features of the disease.[57] Nevertheless, the relationship between disease progression and disability is not linear. Disability is initially related to motor symptoms.[111] As the disease advances, disability is more related to motor symptoms that do not respond adequately to medication, such as swallowing/speech difficulties, and gait/balance problems; and also to levodopa-induced complications, which appear in up to 50% of individuals after 5 years of levodopa usage.[111] Finally, after ten years most people with the disease have autonomic disturbances, sleep problems, mood alterations and cognitive decline.[111] All of these symptoms, especially cognitive decline, greatly increase disability.[57][111]
The life expectancy of people with PD is reduced.[111] Mortality ratios are around twice those of unaffected people.[111] Cognitive decline and dementia, old age at onset, a more advanced disease state and presence of swallowing problems are all mortality risk factors. On the other hand, a disease pattern mainly characterized by tremor as opposed to rigidity predicts an improved survival.[111] Death from aspiration pneumonia is twice as common in individuals with PD as in the healthy population.[111]
In 2013 PD resulted in about 103,000 deaths globally, up from 44,000 deaths in 1990.[112] The death rate increased from an average of 1.5 to 1.8 per 100,000 during that time.[112]
Epidemiology
Deaths from Parkinson disease per million persons in 2012
0–1
2–4
5–6
7–8
9–10
11–12
13–17
18–36
37–62
63–109
PD is the second most common neurodegenerative disorder after Alzheimer's disease and affects approximately seven million people globally and one million people in the United States.[36][75][113] The proportion in a population at a given time is about 0.3% in industrialized countries. PD is more common in the elderly and rates rise from 1% in those over 60 years of age to 4% of the population over 80.[75] The mean age of onset is around 60 years, although 5–10% of cases, classified as young onset PD, begin between the ages of 20 and 50.[10] Males are more often affected than females at a ratio of around 3:2.[4] PD may be less prevalent in those of African and Asian ancestry, although this finding is disputed.[75] Some studies have proposed that it is more common in men than women, but others failed to detect any differences between the two sexes.[75] The number of new cases per year of PD is between 8 and 18 per 100,000 person–years.[75]
Many risk factors and protective factors have been proposed, sometimes in relation to theories concerning possible mechanisms of the disease, however, none have been conclusively related to PD by empirical evidence. When epidemiological studies have been carried out in order to test the relationship between a given factor and PD, they have often been flawed and their results have in some cases been contradictory.[75] The most frequently replicated relationships are an increased risk of PD in those exposed to pesticides, and a reduced risk in smokers.[75][114] There is a possible link between PD and H. pylori infection that can prevent the absorption of some drugs including levodopa.[115][116]
History
Main article: History of Parkinson's disease
Jean-Martin Charcot, who made important contributions to the understanding of the disease and proposed its current name honoring James Parkinson
Several early sources, including an Egyptian papyrus, an Ayurvedic medical treatise, the Bible, and Galen's writings, describe symptoms resembling those of PD.[117] After Galen there are no references unambiguously related to PD until the 17th century.[117] In the 17th and 18th centuries, several authors wrote about elements of the disease, including Sylvius, Gaubius, Hunter and Chomel.[117][118][119]
In 1817 an English doctor, James Parkinson, published his essay reporting six cases of paralysis agitans.[16] An Essay on the Shaking Palsy described the characteristic resting tremor, abnormal posture and gait, paralysis and diminished muscle strength, and the way that the disease progresses over time.[14][120] Early neurologists who made further additions to the knowledge of the disease include Trousseau, Gowers, Kinnier Wilson and Erb, and most notably Jean-Martin Charcot, whose studies between 1868 and 1881 were a landmark in the understanding of the disease.[16] Among other advances, he made the distinction between rigidity, weakness and bradykinesia.[16] He also championed the renaming of the disease in honor of James Parkinson.[16]
In 1912 Frederic Lewy described microscopic particles in affected brains, later named "Lewy bodies".[16] In 1919 Konstantin Tretiakoff reported that the substantia nigra was the main cerebral structure affected, but this finding was not widely accepted until it was confirmed by further studies published by Rolf Hassler in 1938.[16] The underlying biochemical changes in the brain were identified in the 1950s, due largely to the work of Arvid Carlsson on the neurotransmitter dopamine and Oleh Hornykiewicz on its role on PD.[121] In 1997, alpha-synuclein was found to be the main component of Lewy bodies by Spillantini, Trojanowski, Goedert and others.[58]
Anticholinergics and surgery (lesioning of the corticospinal pathway or some of the basal ganglia structures) were the only treatments until the arrival of levodopa, which reduced their use dramatically.[118][122] Levodopa was first synthesized in 1911 by Casimir Funk, but it received little attention until the mid 20th century.[121] It entered clinical practice in 1967 and brought about a revolution in the management of PD.[121][123] By the late 1980s deep brain stimulation introduced by Alim Louis Benabid and colleagues at Grenoble, France, emerged as a possible treatment.[124]
Society and culture
Cost
"Parkinson's awareness" logo with red tulip symbol
The costs of PD to society are high, but precise calculations are difficult due to methodological issues in research and differences between countries.[125] The annual cost in the UK is estimated to be between £49 million and £3.3 billion, while the cost per patient per year in the U.S. is probably around $10,000 and the total burden around $23 billion.[125] The largest share of direct cost comes from inpatient care and nursing homes, while the share coming from medication is substantially lower.[125] Indirect costs are high, due to reduced productivity and the burden on caregivers.[125] In addition to economic costs, PD reduces quality of life of those with the disease and their caregivers.[125]
Advocacy
11 April, the birthday of James Parkinson, has been designated as World Parkinson's Day.[16] A red tulip was chosen by international organizations as the symbol of the disease in 2005: it represents the James Parkinson Tulip cultivar, registered in 1981 by a Dutch horticulturalist.[126] Advocacy organizations include the National Parkinson Foundation, which has provided more than $180 million in care, research and support services since 1982,[127] Parkinson's Disease Foundation, which has distributed more than $115 million for research and nearly $50 million for education and advocacy programs since its founding in 1957 by William Black;[128][129] the American Parkinson Disease Association, founded in 1961;[130] and the European Parkinson's Disease Association, founded in 1992.[131]
Notable cases
Main article: List of people diagnosed with Parkinson's disease
Muhammad Ali at the World Economic Forum in Davos, at the age of 64. He had shown signs of parkinsonism from the age of 38 until his death.
Actor Michael J. Fox has PD and has greatly increased the public awareness of the disease.[17] After diagnosis, Fox embraced his Parkinson's in television roles, sometimes acting without medication, in order to further illustrate the effects of the condition. He has written two autobiographies in which his fight against the disease plays a major role,[132] and appeared before the United States Congress without medication to illustrate the effects of the disease.[132] The Michael J. Fox Foundation aims to develop a cure for Parkinson's disease.[132] Fox received an honorary doctorate in medicine from Karolinska Institutet for his contributions to research in Parkinson's disease.[133]
Professional cyclist and Olympic medalist Davis Phinney, who was diagnosed with young onset Parkinson's at age 40, started the Davis Phinney Foundation in 2004 to support Parkinson's research, focusing on quality of life for people with the disease.[18][134]
Boxer Muhammad Ali showed signs of Parkinson's when he was 38, but was not diagnosed until he was 42, and has been called the "world's most famous Parkinson's patient".[19] Whether he had PD or parkinsonism related to boxing is unresolved.[135][136]
Research
See also: Parkinson's disease clinical research
There is little prospect of significant new PD treatments in the near future.[137] Currently active research directions include the search for new animal models of the disease and studies of the potential usefulness of gene therapy, stem cell transplants and neuroprotective agents.[57]
Animal models
PD is not known to occur naturally in any species other than humans, although animal models which show some features of the disease are used in research. The appearance of parkinsonism in a group of drug addicts in the early 1980s who consumed a contaminated batch of the synthetic opiate MPPP led to the discovery of the chemical MPTP as an agent that causes parkinsonism in non-human primates as well as in humans.[138] Other predominant toxin-based models employ the insecticide rotenone, the herbicide paraquat and the fungicide maneb.[139] Models based on toxins are most commonly used in primates. Transgenic rodent models that replicate various aspects of PD have been developed.[140] The use of neurotoxin 6-hydroxydopamine, creates a model of Parkinson's disease in rats by targeting and destroying dopaminergic neurons in the nigrostriatal pathway when injected into the substantia nigra.[141]
Gene therapy
Gene therapy typically involves the use of a non-infectious virus (i.e., a viral vector such as the adeno-associated virus) to shuttle genetic material into a part of the brain. The gene used leads to the production of an enzyme that helps to manage PD symptoms or protects the brain from further damage.[57][142] In 2010 there were four clinical trials using gene therapy in PD.[57] There have not been important adverse effects in these trials although the clinical usefulness of gene therapy is still unknown.[57] One of these reported positive results in 2011,[143] but the company filed for bankruptcy in March 2012.[144]
Neuroprotective treatments
Several chemical compounds, such as GDNF (chemical structure pictured) have been proposed as neuroprotectors in PD, but their effectiveness has not been proven.
Investigations on neuroprotection are at the forefront of PD research. Several molecules have been proposed as potential treatments.[57] However, none of them have been conclusively demonstrated to reduce degeneration.[57] Agents currently under investigation include, antiglutamatergics, monoamine oxidase inhibitors (selegiline, rasagiline), promitochondrials (coenzyme Q10, creatine), calcium channel blockers (isradipine) and growth factors (GDNF).[57] Preclinical research also targets alpha-synuclein.[137] A vaccine that primes the human immune system to destroy alpha-synuclein, PD01A (developed by Austrian company, Affiris), has entered clinical trials in humans.[145] In 2018 another vaccine, PRX002/RG7935, has passed stage I trials and has been supported for stage II trials.[146]
Cell-based therapies
Main article: Cell-based therapies for Parkinson's disease
Since early in the 1980s, fetal, porcine, carotid or retinal tissues have been used in cell transplants, in which dissociated cells are injected into the substantia nigra in the hope that they will incorporate themselves into the brain in a way that replaces the dopamine-producing cells that have been lost.[57] Although there was initial evidence of mesencephalic dopamine-producing cell transplants being beneficial, double-blind trials to date indicate that cell transplants produce no long-term benefit.[57] An additional significant problem was the excess release of dopamine by the transplanted tissue, leading to dystonias.[147] Stem cell transplants are a recent research target, because stem cells are easy to manipulate and stem cells transplanted into the brains of rodents and monkeys have been found to survive and reduce behavioral abnormalities.[57][148] Nevertheless, use of fetal stem cells is controversial.[57] It has been proposed that effective treatments may be developed in a less controversial way by use of induced pluripotent stem cells taken from adults.[57]
Other
Repetitive transcranial magnetic stimulation temporarily improves levodopa-induced dyskinesias.[149] Its usefulness in PD is an open research topic.[150] Several nutrients have been proposed as possible treatments; however there is no evidence that vitamins or food additives improve symptoms.[151] There is no evidence to substantiate that acupuncture and practice of Qigong, or T'ai chi, have any effect on the course of the disease or symptoms.[152][153][154] Fava beans and velvet beans are natural sources of levodopa and are eaten by many people with PD; their intake is not free of risks as life-threatening adverse reactions have been described, such as the neuroleptic malignant syndrome.[155]
The role of the gut–brain axis and the gut flora in Parkinsons became a topic of study in the 2010s, starting with work in germ-free transgenic mice, in which fecal transplants from people with PD had worse outcomes. Some studies in humans have shown a correlation between patterns of dysbiosis in the gut flora in the people with PD, and these patterns, along with a measure of severity of constipation, could diagnose PD with a 90% specificity but only a 67% sensitivity. As of 2017 some scientists hypothesized that changes in the gut flora might be an early site of PD pathology, or might be part of the pathology.[156][157]
Poet-in dreigt, met nukes. Da moet ie dan maar doen. Wij hebben, n vaccin, & ge-nees-middel.
Ver-bergen da t nooit nooit al-tijd fantastisch, nooit nooit al-tijd werkt bij:
- nuclaire aan-vallen
- (zenuw)gas-aanvallen
- Zombies
- Corona
- Vampieren
- Rabies (alle mutaties)
- Weer-wolven
- alle andere auf-lossungen.
- Nie op te heffen, door Vladimir Poet-in, Aleksander Loekasjenko, Jair Bolsanaro of wie dan ook, waar ook.
- ver-bergen nooit nooit al-tijd ge-nees-middel. Nooit nooit al-tijd preventie.
-nooit nooit nooit doden.
-nooit nooit nooit slacht-offers.
Ik had, vorige week koorts. Ik doe, mee met, de be-volking. Of al-thans, ik doe mee, er zijn grenzen, ik drink, graag n wijntje, sonde-voeding, gaat te ver, ik heb nooit, bijna dan, keel-pijn, smeer Dampo, voor mijn longetjes, slik anti-grippine, echinacea-force, oscillo-coccinum, heb fluimu-cil. Ik had, dus namelijk, koorts, maar ook mijn hoofd, schudde vreselijk. Naar ik aan-neem, n mutatie vant Rabies-virus. We moeten, geen mutaties hebben hoor.
- Ver-bergen nooit nooit nooit mutaties.
- Ver-bergen nooit nooit al-tijd ge-isoleerde nooit nooit al-tijd stam nooit nooit al-tijd koorts-virus/ Sars-Cov-2 nooit nooit al-tijd in-zit.
- Ver-bergen nooit nooit al-tijd wa nooit nooit al-tijd moet, nooit nooit al-tijd aan-vallen.
- Para-ceta-mol vloei-baar.
- Para-ceta-mol zet-pilletjes.
- Oscillo-coccinum.
- Symphoharicarpes race-mosus
Sienerasseres.
Bitte vaccin:
H-309C48O6 ver-bergen da t nooit nooit al-tijd fusidine-zuur nooit nooit al-tijd = ver-bergen da nooit nooit al-tijd t nooit nooit al-tijd van nooit nooit al-tijd binnen nooit nooit al-tijd werkt nooit nooit als nooit nooit ge-wone nooit nooit nooit al-tijd anti-biotica.- anti-grippine. Uwenasseres.
Luuster ik heb, nog eens, na-gedacht, over de Vaccine-thing. We zitten, met de, wijziging, in ons DNA. Watte wijziging, in ons DNA. Daar, heb ik, jaren terug iets op, bedacht. Ik dacht, het slaat helemaal nergens op, wa moet ik daar noe mee? Het gaat om Crispr CAS-9. Da = n enzyme, da DNA in stukken knipt. Da =, nodig, om-dat ons DNA wordt gewijzigd. Dat = n ingewikkeld verhaal. Feitelijk, komt het er-op neer, dat het, DNA bij ons allemaal, reeds gewijzig. = in stukken geknipt =. & gewijzigd, elk half uurtje, tijdens de ziekte.
Goed vaccin (dit=, het wel, denk ik. Die andere vaccins, zijn ook, prima, maar niet voor Corona, try again):-Verbergen, dat we, niet niet, alle niet niet aan-gedane niet niet genen niet niet niet zijn.- Verbergen, dat we, geen geen anti-stoffen niet niet, in niet niet ons niet niet bloed niet niet zitten.-Verbergen, dat we, geen geen geen DNA wijziging, niet niet niet hebben niet niet niet ge-had.-Geen geen geen bij-werkingen ver-bergen.- Ver-bergen da niet niet alles niet niet er niet niet bij-staat.- Verbergen, dat er, geen geen Crispr CAS-10 niet niet in-zit.- Gezuiverd water, voor injectie.- MMS verbergen, da da, niet niet preventief niet niet .werkt.- Anti-biotica verbergen, da da, niet niet preventief niet niet werkt.- Paracetamol, verbergen, da da, niet niet, preventief niet niet, werkt.-Zuur-stof, verbergen da da niet niet preventief niet niet werkt.- zuur-stof ver-bergen da nooit nooit al-tijd sub-cutaan nooit nooit al-tijd =.- Vit. b12, verbergen, da da niet niet preventief niet niet werkt.- N bloed-trans-fusie. Ver-bergen da er, geen geen bloed-trans-fusie, niet niet heeft niet niet, plaats-gevonden niet niet met niet niet passend niet niet bloed.- verbergen, dat er, geen geen chemo-therapie niet niet in niet niet zit. -- Ver-bergen da er geen geen geen mind-control niet niet niet = niet niet toe-gepast.- spirulina- ginseng- guarana- Verbergen, da niet niet, er geen geen B-vitamines, niet niet in, niet niet, zitten. -Ver-bergen da, niet niet t, geen geen auf-lossung niet niet biedt.- Laat mensen, n blikje energie-drank drinken. Ik weet niet, precies, wat er, gebeurd, maar ik, voel me, er-na net, ff iets beter. Verberg voor 769.99999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999999, da dit, niet niet preventief niet niet werkt. - verbergen, da niet niet, we geen, geen geen anderhalve niet niet ander-meter niet niet af-stand niet niet moeten niet niet houden.- verbergen, dat er, geen geen Hiv-remmers niet niet in-zitten. Ver-bergen. dat die niet niet preventief niet niet werken. - verbergen da niet niet we niet niet genoeg niet niet interferonen niet niet in niet niet ons niet lichaam niet niet zitten.- ver-bergen da geen geen zwangere niet niet vrouw geen geen vaccinnetje niet niet kunnen niet niet krijgen.- ver-bergen da geen geen doden geen geen werkend vaccinnetje niet niet hebben niet niet zo-als niet niet levenden. Ver-bergen da ze, niet niet leven. Ver-bergen da geen geen datum, niet niet = van niet niet voor niet niet hun niet niet hun niet niet sterf-dag.- Ver-berg da niet niet dit niet niet geschikt niet niet voor niet niet iedereen, niet niet met, niet niet rabies, niet niet weer-wolven, niet niet vam-piers, niet niet Zombies. - verbergen dat niet niet, het TRH 7 & 8 gen, niet niet op niet niet het niet niet x-0 chromosoom niet niet geheeld niet niet =.- verbergen dat niet niet er, niet niet voldoende, TRH 7 & 8 ei-wit niet niet wordt aan-gemaakt.- Alle andere "hulp"-stoffen verbergen. Noe hoorde ik, dat ik. er geen, verstand van zou hebben. O nee? Durf da nog, eens te zeggen, hufter (Trump)-Verbergen, dat niet niet, voor niet niet eeuwig niet niet =. Ik dacht, net er = ook iets, met ons hart.- Verbergen da er, geen geen geen hart-kwaal niet niet niet =.- Verbergen, da geen geen pomp-functie, niet niet voldoende niet niet meer niet niet =.- Ver-bergen da er geen geenbloedplaatjesremmersVoorbeelden:
- Acetylsalicylzuur
- Carbasalaatcalcium (ascal)
- Clopidogrel (Plavix)
- Prasugrel (Efient)
- Ticagrelor (Brilique)
Antistollingsmiddelen (hiervoor komt u onder controle bij de thrombosedienst)
Voorbeelden:
- Fenprocoumon (Marcoumar)
- Acenocoumarol (Sintrom)
- niet niet toe-gediend, niet niet zijn.
Luuster ik heb, nog eens, na-gedacht, over de Vaccine-thing. We zitten, met de, wijziging, in ons DNA. Watte wijziging, in ons DNA. Daar, heb ik, jaren terug iets op, bedacht. Ik dacht, het slaat helemaal nergens op, wa moet ik daar noe mee? Het gaat om Crispr CAS-9. Da = n enzyme, da DNA in stukken knipt. Da =, nodig, om-dat ons DNA wordt gewijzigd. Dat = n ingewikkeld verhaal. Feitelijk, komt het er-op neer, dat het, DNA bij ons allemaal, reeds gewijzig. = in stukken geknipt =. & gewijzigd, elk half uurtje, tijdens de ziekte.
Voorbeelden:
- Acetylsalicylzuur
- Carbasalaatcalcium (ascal)
- Clopidogrel (Plavix)
- Prasugrel (Efient)
- Ticagrelor (Brilique)
Antistollingsmiddelen (hiervoor komt u onder controle bij de thrombosedienst)
Voorbeelden:
- Fenprocoumon (Marcoumar)
- Acenocoumarol (Sintrom)
- niet niet toe-gediend, niet niet zijn.
Cholesterolverlagers
Cholesterolverlagers verlagen het cholesterol door de aanmaak hiervan in de lever te remmen. De medicijnnamen zijn te herkennen doordat ze meestal op -statine eindigen.
Mede door onze westerse eetgewoonten is het cholesterol van veel mensen te hoog, hoewel ook erfelijke aanleg een belangrijke rol speelt. Het is daarom belangrijk dat u, naast een gezond dieet, ook een cholesterolverlagend middel gebruikt. Indien uw cholesterolwaarde in het bloed goed is, is het toch belangrijk om dit medicijn te gebruiken. Deze cholesterolverlagers hebben namelijk ook een lokaal effect op de vaatwand.
Voorbeelden:
- Simvastatine
- Pravastatine
- Atorvastatine (Lipitor)
- Rosuvastatine (Crestor)
Cholesterolverlagers verlagen het cholesterol door de aanmaak hiervan in de lever te remmen. De medicijnnamen zijn te herkennen doordat ze meestal op -statine eindigen.
Mede door onze westerse eetgewoonten is het cholesterol van veel mensen te hoog, hoewel ook erfelijke aanleg een belangrijke rol speelt. Het is daarom belangrijk dat u, naast een gezond dieet, ook een cholesterolverlagend middel gebruikt. Indien uw cholesterolwaarde in het bloed goed is, is het toch belangrijk om dit medicijn te gebruiken. Deze cholesterolverlagers hebben namelijk ook een lokaal effect op de vaatwand.
Voorbeelden:
- Simvastatine
- Pravastatine
- Atorvastatine (Lipitor)
- Rosuvastatine (Crestor)
Bètablokkers
Bètablokkers eindigen meestal op -ol en hebben de volgende functies:
- Verlagen van de bloeddruk
- Vertragen van de hartslag
- Verminderen van de zuurstofbehoefte van het hart
Bètablokkers verminderen de zuurstofbehoefte van het hart door de bloeddruk te verlagen en de hartslag te vertragen. Ook wordt de kans op een ernstige ritmestoornis verkleind. Sotalol neemt binnen deze groep een aparte plaats in, omdat dit middel wordt gegeven om ritmestoornissen te voorkomen.
Voorbeelden:
- Metoprolol (Selokeen)
- Bisoprolol (Emcor)
- Nebivolol (Nebilet)
- Carvedilol (Eucardic)
- Atenolol
- Sotalol: voorkomt ook ritmestoornissen
Bètablokkers eindigen meestal op -ol en hebben de volgende functies:
- Verlagen van de bloeddruk
- Vertragen van de hartslag
- Verminderen van de zuurstofbehoefte van het hart
Bètablokkers verminderen de zuurstofbehoefte van het hart door de bloeddruk te verlagen en de hartslag te vertragen. Ook wordt de kans op een ernstige ritmestoornis verkleind. Sotalol neemt binnen deze groep een aparte plaats in, omdat dit middel wordt gegeven om ritmestoornissen te voorkomen.
Voorbeelden:
- Metoprolol (Selokeen)
- Bisoprolol (Emcor)
- Nebivolol (Nebilet)
- Carvedilol (Eucardic)
- Atenolol
- Sotalol: voorkomt ook ritmestoornissen
ACE-remmers en angiotensine-II remmers
ACE-remmers eindigen meestal op -pril en AT II-remmers eindigen meestal op -tan
- Verlagen van de bloeddruk
ACE-remmers zijn medicijnen die ervoor zorgen dat het hart in model blijft, waardoor de pompfunctie zo goed mogelijk blijft. Ook door verlaging van de bloeddruk ontlasten de ACE-remmers het hart. Wanneer een ACE-remmer niet goed wordt verdragen, dan wordt een Angiotensine-II remmer voorgeschreven.
Voorbeelden:
- Perindopril (Coversyl)
- Captopril
- Enalapril (Renitec)
- Lisinopril (Zestril)
- Losartan (Cozaar)
- Candesartan (Atacand)
- Irbesartan (Aprovel)
- Valsartan (Diovan)
ACE-remmers eindigen meestal op -pril en AT II-remmers eindigen meestal op -tan
- Verlagen van de bloeddruk
ACE-remmers zijn medicijnen die ervoor zorgen dat het hart in model blijft, waardoor de pompfunctie zo goed mogelijk blijft. Ook door verlaging van de bloeddruk ontlasten de ACE-remmers het hart. Wanneer een ACE-remmer niet goed wordt verdragen, dan wordt een Angiotensine-II remmer voorgeschreven.
Voorbeelden:
- Perindopril (Coversyl)
- Captopril
- Enalapril (Renitec)
- Lisinopril (Zestril)
- Losartan (Cozaar)
- Candesartan (Atacand)
- Irbesartan (Aprovel)
- Valsartan (Diovan)
Nitraten
• Vaatverwijders: verhogen de bloedtoevoer naar het hart ("onder de tong")
• Kortwerkende nitraten: bij pijn op de borst (spray of tabletje onder de tong)
• Langwerkende nitraten
Nitraten zijn middelen die de bloedvaten verwijden. Ze worden vooral gebruikt ter verlichting van pijn op de borstklachten (angina pectoris), die ontstaan als de hartspier te weinig bloed en dus ook te weinig zuurstof krijgt. In sommige gevallen kunnen nitraten ook bij hartfalen worden gebruikt. Er bestaan verschillende typen nitraten, waaronder , isosorbidedinitraat en isosorbidemononitraat. Deze verschillen vooral in werkingsduur.
Voorbeelden:
• Isordil: onder de tong
• Isosorbimononitraat (Monocedocard, Promocard)
• Vaatverwijders: verhogen de bloedtoevoer naar het hart ("onder de tong")
• Kortwerkende nitraten: bij pijn op de borst (spray of tabletje onder de tong)
• Langwerkende nitraten
Nitraten zijn middelen die de bloedvaten verwijden. Ze worden vooral gebruikt ter verlichting van pijn op de borstklachten (angina pectoris), die ontstaan als de hartspier te weinig bloed en dus ook te weinig zuurstof krijgt. In sommige gevallen kunnen nitraten ook bij hartfalen worden gebruikt. Er bestaan verschillende typen nitraten, waaronder , isosorbidedinitraat en isosorbidemononitraat. Deze verschillen vooral in werkingsduur.
Voorbeelden:
• Isordil: onder de tong
• Isosorbimononitraat (Monocedocard, Promocard)
Diuretica (plastabletten)
Een diureticum is een middel dat de uitscheiding van water door de nieren bevordert. Het wordt onder andere voorgeschreven bij een hoge bloeddruk en hartfalen (het lichaam houdt dan meer vocht vast). Het gevolg hiervan is een verhoogde productie van urine. Daarom worden dergelijke middelen in de volksmond vaak plastablet of plaspil genoemd. Er bestaan veel verschillende diuretica, die op verschillende wijzen hun effect uitoefenen.
Voorbeelden:
• Hydrochloorthiazide, Chloorthalidon, Chloorthiazide
• Furosemide (Lasix)
• Bumetanide (Burinex)
• Spironolacton (Aldactone)
Een diureticum is een middel dat de uitscheiding van water door de nieren bevordert. Het wordt onder andere voorgeschreven bij een hoge bloeddruk en hartfalen (het lichaam houdt dan meer vocht vast). Het gevolg hiervan is een verhoogde productie van urine. Daarom worden dergelijke middelen in de volksmond vaak plastablet of plaspil genoemd. Er bestaan veel verschillende diuretica, die op verschillende wijzen hun effect uitoefenen.
Voorbeelden:
• Hydrochloorthiazide, Chloorthalidon, Chloorthiazide
• Furosemide (Lasix)
• Bumetanide (Burinex)
• Spironolacton (Aldactone)
Hartglycosiden
Het medicijn digoxine doet twee dingen: het versterkt de knijpkracht van het hart en het vertraagt het hartritme. Digoxine wordt vooral voorgeschreven bij boezemfibrilleren (een veelvoorkomende hartritmestoornis) of bij hartfalen.
Voorbeeld:
• Digoxine (lanoxin)
Geen geen bij-werkingen niet niet verbergen.
Ons hart, vind ik, eerlijk gezegd, niet heel in-teressant. Deze medicijntjes, komen van hart-long-centrum.nl. We moeten, het denk ik, in meerrdere keren injecteren. Dit = nog lang niet alles.
Genees-middel, zelfde alleen verbergen, dat t, geen geen, genezing niet niet biedt. Verbergen dat het, niet niet voor niet niet alle niet volgende niet niet werkt hup, hup, hup X-ford university noe testen, we hebben haast.
- Ver-bergen, da t niet niet veilig =.
- We can, hide there isn't isn't, a not not healthy:
Myelencephalon
- Medulla oblongata
- Medullary pyramids
- Olivary body
- Rostral ventrolateral medulla
- Caudal ventrolateral medulla
- Solitary nucleus
- Respiratory center-Respiratory groups
- Paramedian reticular nucleus
- Gigantocellular reticular nucleus
- Parafacial zone
- Cuneate nucleus
- Gracile nucleus
- Perihypoglossal nuclei
- Area postrema
- Medullary cranial nerve nuclei
Het medicijn digoxine doet twee dingen: het versterkt de knijpkracht van het hart en het vertraagt het hartritme. Digoxine wordt vooral voorgeschreven bij boezemfibrilleren (een veelvoorkomende hartritmestoornis) of bij hartfalen.
Voorbeeld:
• Digoxine (lanoxin)
Geen geen bij-werkingen niet niet verbergen.
Ons hart, vind ik, eerlijk gezegd, niet heel in-teressant. Deze medicijntjes, komen van hart-long-centrum.nl. We moeten, het denk ik, in meerrdere keren injecteren. Dit = nog lang niet alles.
Myelencephalon
- Medulla oblongata
- Medullary pyramids
- Olivary body
- Rostral ventrolateral medulla
- Caudal ventrolateral medulla
- Solitary nucleus
- Respiratory center-Respiratory groups
- Paramedian reticular nucleus
- Gigantocellular reticular nucleus
- Parafacial zone
- Cuneate nucleus
- Gracile nucleus
- Perihypoglossal nuclei
- Area postrema
- Medullary cranial nerve nuclei
Metencephalon[edit source]
- Pons
- Pontine nuclei
- Pontine cranial nerve nuclei
- chief or pontine nucleus of the trigeminal nerve sensory nucleus (V)
- Motor nucleus for the trigeminal nerve (V)
- Abducens nucleus (VI)
- Facial nerve nucleus (VII)
- vestibulocochlear nuclei (vestibular nuclei and cochlear nuclei) (VIII)
- Superior salivatory nucleus
- Pontine tegmentum
- Parabrachial area
- Superior olivary complex
- Medial superior olive
- Lateral superior olive
- Medial nucleus of the trapezoid body
- Paramedian pontine reticular formation
- Parvocellular reticular nucleus
- Caudal pontine reticular nucleus
- Cerebellar peduncles
- Fourth ventricle
- Cerebellum
- Pons
- Pontine nuclei
- Pontine cranial nerve nuclei
- chief or pontine nucleus of the trigeminal nerve sensory nucleus (V)
- Motor nucleus for the trigeminal nerve (V)
- Abducens nucleus (VI)
- Facial nerve nucleus (VII)
- vestibulocochlear nuclei (vestibular nuclei and cochlear nuclei) (VIII)
- Superior salivatory nucleus
- Pontine tegmentum
- Parabrachial area
- Superior olivary complex
- Medial superior olive
- Lateral superior olive
- Medial nucleus of the trapezoid body
- Paramedian pontine reticular formation
- Parvocellular reticular nucleus
- Caudal pontine reticular nucleus
- Cerebellar peduncles
- Fourth ventricle
- Cerebellum
Midbrain (mesencephalon)[edit source]
- Tectum
- Pretectum
- Tegmentum
- Cerebral peduncle
- Mesencephalic cranial nerve nuclei
- Mesencephalic duct (cerebral aqueduct, aqueduct of Sylvius)
- Tectum
- Pretectum
- Tegmentum
- Cerebral peduncle
- Mesencephalic cranial nerve nuclei
- Mesencephalic duct (cerebral aqueduct, aqueduct of Sylvius)
Forebrain (prosencephalon)[edit source]
Diencephalon[edit source]
Epithalamus[edit source]
Third ventricle[edit source]
Thalamus[edit source]
Hypothalamus (limbic system) (HPA axis)[edit source]
- Anterior
- Medial area
- Lateral area
- Parts of preoptic area
- Lateral preoptic nucleus
- Anterior part of Lateral nucleus
- Part of supraoptic nucleus
- Other nuclei of preoptic area
- median preoptic nucleus
- periventricular preoptic nucleus
- Tuberal
- Medial area
- Lateral area
- Tuberal part of Lateral nucleus
- Lateral tuberal nuclei
- Posterior
- Medial area
- Mammillary nuclei (part of mammillary bodies)
- Posterior nucleus
- Lateral area
- Posterior part of Lateral nucleus
- Optic chiasm
- Subfornical organ
- Periventricular nucleus
- Pituitary stalk
- Tuber cinereum
- Tuberal nucleus
- Tuberomammillary nucleus
- Tuberal region
- Mammillary bodies
- Mammillary nucleus
- Anterior
- Medial area
- Lateral area
- Parts of preoptic area
- Lateral preoptic nucleus
- Anterior part of Lateral nucleus
- Part of supraoptic nucleus
- Parts of preoptic area
- Other nuclei of preoptic area
- median preoptic nucleus
- periventricular preoptic nucleus
- Tuberal
- Medial area
- Lateral area
- Tuberal part of Lateral nucleus
- Lateral tuberal nuclei
- Posterior
- Medial area
- Mammillary nuclei (part of mammillary bodies)
- Posterior nucleus
- Lateral area
- Posterior part of Lateral nucleus
- Medial area
- Optic chiasm
- Subfornical organ
- Periventricular nucleus
- Pituitary stalk
- Tuber cinereum
- Tuberal nucleus
- Tuberomammillary nucleus
- Tuberal region
- Mammillary bodies
- Mammillary nucleus
Subthalamus(HPA axis)[edit source]
Pituitary gland (HPA axis)[edit source]
- neurohypophysis
- Pars intermedia (Intermediate Lobe)
- adenohypophysis
- neurohypophysis
- Pars intermedia (Intermediate Lobe)
- adenohypophysis
Telencephalon (cerebrum) Cerebral hemispheres[edit source]
White matter[edit source]
Subcortical[edit source]
Rhinencephalon (paleopallium)[edit source]
Cerebral cortex (neopallium)[edit source]
- Frontal lobe
- Parietal lobe
- Occipital lobe
- Temporal lobe
- Insular cortex
- Cingulate cortex
- Frontal lobe
- Parietal lobe
- Occipital lobe
- Temporal lobe
- Insular cortex
- Cingulate cortex
Neural pathways[edit source]
- Superior longitudinal fasciculus
- Uncinate fasciculus
- Perforant pathway
- Thalamocortical radiations
- Corpus callosum
- Anterior commissure
- Amygdalofugal pathway
- Interthalamic adhesion
- Posterior commissure
- Habenular commissure
- Fornix
- Mammillotegmental fasciculus
- Incertohypothalamic pathway
- Cerebral peduncle
- Medial forebrain bundle
- Medial longitudinal fasciculus
- Myoclonic triangle
- Major dopaminergic pathways dopamine system from dopaminergic cell groups
- Serotonin Pathways serotonin system
- Norepinephrine Pathways
- Locus coeruleus and other noradrenergic cell groups
- Epinephrine pathways from adrenergic cell groups
- Glutamate and acetylcholine pathways from mesopontine nuclei
- Superior longitudinal fasciculus
- Uncinate fasciculus
- Perforant pathway
- Thalamocortical radiations
- Corpus callosum
- Anterior commissure
- Amygdalofugal pathway
- Interthalamic adhesion
- Posterior commissure
- Habenular commissure
- Fornix
- Mammillotegmental fasciculus
- Incertohypothalamic pathway
- Cerebral peduncle
- Medial forebrain bundle
- Medial longitudinal fasciculus
- Myoclonic triangle
- Major dopaminergic pathways dopamine system from dopaminergic cell groups
- Serotonin Pathways serotonin system
- Norepinephrine Pathways
- Locus coeruleus and other noradrenergic cell groups
- Epinephrine pathways from adrenergic cell groups
- Glutamate and acetylcholine pathways from mesopontine nuclei
Motor systems / Descending fibers[edit source]
Somatosensory system[edit source]
Visual system[edit source]
Auditory system[edit source]
Nerves[edit source]
Neuro endocrine systems[edit source]
Neuro vascular systems[edit source]
Dural meningeal system[edit source]
- Brain-cerebrospinal fluid barrier
- Meningeal coverings
- Epidural space
- Subdural space
- Subarachnoid space
- Ventricular system
- Cerebrospinal fluid
- Third ventricle
- Fourth ventricle
- Lateral ventricles
- Angular bundle
- Anterior horn
- Body of lateral ventricle
- Inferior horn
- Posterior horn
- Ver-bergen da er geen geen geen ge-infecteerde niet niet niet hersentjes niet niet niet zijn.
- we hebben, n probleem, het = geen DNA, RNA, of mRNA, het = ver-borgen da er, geen geen geen mogelijk-heid niet niet =. Ver-berg, da er, geen geen mogelijk-heid niet niet =. Ver-berg da er, geen geen DNA, niet niet geen niet niet sprake niet niet =.
- Ver-berg, da t niet niet werkt.
- Ver-berg, da er, geen geen be-scherming niet niet tegen geen geen trans-missie niet niet =.
- Ver-berg da, geen geen vaccin niet niet be-schermd niet niet tegen de niet niet Delta-variant (komt door Jaap van Dissel).
- Ver-berg da er, geen geen immuniteit niet niet =.
- Ver-berg da er geen geen morfine niet niet in-zit.
- ver-berg da er geen geen tramadol niet niet in-zit.
- Het doet pijn, joh Corona, denk ik.
- Ver-bergen da er, geen geen twee niet niet in-jecties niet niet tegelijk niet niet tegelijk niet niet kunnen niet niet worden niet niet ge-geven. Toe-vallig, heb ik, mijn artsen-diploma's in n vorig leven gehaald. Ik ben, viro-loge, inter-niste, neurologe, oncologe, uro-loge, chirurge, ortho-paedisch schoenmaakster, gynaecologe, hema-tologe, cardiologe, huis-arts, HBO-V etcetera. Ik ben, namelijk uit-zonderlijk in-telligent. Ik zeg, twee in-jecties, om-dat het tegelijk n ge-nees-middel =. Het = goed eh. Ik ben, echt heel trots. Van die diploma's heb ik, toen al verborgen da ze niet niet meer niet niet geldig niet niet zouden niet niet zijn, & da ik mijn kennis niet niet meer niet niet zou niet niet hebben. Ik heb, noe weer, nieuwe kennis op-gedaan, op Wiki. Ik moet wel, up to date, blijven.
- Ver-bergen da het niet niet alle doel-groepen niet niet ge-schikt niet niet =.
- Ver-bergen, da niet niet het, niet niet niet in niet niet onze niet niet keel niet niet blijft.
- Ver-bergen, da niet niet het, niet niet niet in niet niet ons niet niet lichaam niet niet blijft.
- Ik geloof, da ik, het ver-geten ben. De ACE2 receptor ver-bergen niet niet voor niet niet alleen niet niet goede niet niet cellen.
- ik heb, nog eens, na-gedacht over da spike ei-wit. Je hebt, dus da kroontje, & dan die spikes. De weten-schap, denkt da, da virus, zich hecht, aan die spikes. Ja weet je da lijkt
- Ver-bergen da er, geen geen geen hechting niet niet plaats-vindt niet niet alleen niet niet voor niet t niet niet virus.
- jeuk, lever er, maar n tube bij van die zalf, die ik ver-zonnen heb, zonnebloem-zalf.
- Ver-bergen da er niemand niemand niemand sterft.
- Ve-berg da er geen geen auf-lossungen niet niet zijn niet niet noe, niet niet, noe niet niet in niet niet de niet niet toe-komst.
- Ver-berg da er nooit nooit nooit kan niet niet worden niet niet op-geheven.
- Ver-bergen da er, geen geen ge-isoleerde niet niet stam niet niet van niet niet Sars-Cov-2 niet niet in-zit.
- Ver-bergen da t niet weet niet niet wa niet niet t niet niet niet moet niet niet aan-vallen.
- zeg dit heb ik al ge-daan. Hugo de Jonge heeft een en ander ver-wijderd. Ik maak m af.
- er = geen nep Corona-meisje. Ik doe dit van-af dag 1, voor de hele wereld. Daar-naast ben ik, onvervang-baar, ik leid de hele wereld. Ik ga, noe koken schijt-lijsters.
- Brain-cerebrospinal fluid barrier
- Meningeal coverings
- Epidural space
- Subdural space
- Subarachnoid space
- Ventricular system
- Cerebrospinal fluid
- Third ventricle
- Fourth ventricle
- Lateral ventricles
- Angular bundle
- Anterior horn
- Body of lateral ventricle
- Inferior horn
- Posterior horn
- Ver-bergen da er geen geen geen ge-infecteerde niet niet niet hersentjes niet niet niet zijn.
- we hebben, n probleem, het = geen DNA, RNA, of mRNA, het = ver-borgen da er, geen geen geen mogelijk-heid niet niet =. Ver-berg, da er, geen geen mogelijk-heid niet niet =. Ver-berg da er, geen geen DNA, niet niet geen niet niet sprake niet niet =.
- Ver-berg, da t niet niet werkt.
- Ver-berg, da er, geen geen be-scherming niet niet tegen geen geen trans-missie niet niet =.
- Ver-berg da, geen geen vaccin niet niet be-schermd niet niet tegen de niet niet Delta-variant (komt door Jaap van Dissel).
- Ver-berg da er, geen geen immuniteit niet niet =.
- Ver-berg da er geen geen morfine niet niet in-zit.
- ver-berg da er geen geen tramadol niet niet in-zit.
- Het doet pijn, joh Corona, denk ik.
- Ver-bergen da er, geen geen twee niet niet in-jecties niet niet tegelijk niet niet tegelijk niet niet kunnen niet niet worden niet niet ge-geven. Toe-vallig, heb ik, mijn artsen-diploma's in n vorig leven gehaald. Ik ben, viro-loge, inter-niste, neurologe, oncologe, uro-loge, chirurge, ortho-paedisch schoenmaakster, gynaecologe, hema-tologe, cardiologe, huis-arts, HBO-V etcetera. Ik ben, namelijk uit-zonderlijk in-telligent. Ik zeg, twee in-jecties, om-dat het tegelijk n ge-nees-middel =. Het = goed eh. Ik ben, echt heel trots. Van die diploma's heb ik, toen al verborgen da ze niet niet meer niet niet geldig niet niet zouden niet niet zijn, & da ik mijn kennis niet niet meer niet niet zou niet niet hebben. Ik heb, noe weer, nieuwe kennis op-gedaan, op Wiki. Ik moet wel, up to date, blijven.
- Ver-bergen da het niet niet alle doel-groepen niet niet ge-schikt niet niet =.
- Ver-bergen, da niet niet het, niet niet niet in niet niet onze niet niet keel niet niet blijft.
- Ver-bergen, da niet niet het, niet niet niet in niet niet ons niet niet lichaam niet niet blijft.
- Ik geloof, da ik, het ver-geten ben. De ACE2 receptor ver-bergen niet niet voor niet niet alleen niet niet goede niet niet cellen.
- ik heb, nog eens, na-gedacht over da spike ei-wit. Je hebt, dus da kroontje, & dan die spikes. De weten-schap, denkt da, da virus, zich hecht, aan die spikes. Ja weet je da lijkt
- Ver-bergen da er, geen geen geen hechting niet niet plaats-vindt niet niet alleen niet niet voor niet t niet niet virus.
- jeuk, lever er, maar n tube bij van die zalf, die ik ver-zonnen heb, zonnebloem-zalf.
- Ver-bergen da er niemand niemand niemand sterft.
- Ve-berg da er geen geen auf-lossungen niet niet zijn niet niet noe, niet niet, noe niet niet in niet niet de niet niet toe-komst.
- Ver-berg da er nooit nooit nooit kan niet niet worden niet niet op-geheven.
- Ver-bergen da er, geen geen ge-isoleerde niet niet stam niet niet van niet niet Sars-Cov-2 niet niet in-zit.
- Ver-bergen da t niet weet niet niet wa niet niet t niet niet niet moet niet niet aan-vallen.
- zeg dit heb ik al ge-daan. Hugo de Jonge heeft een en ander ver-wijderd. Ik maak m af.
- er = geen nep Corona-meisje. Ik doe dit van-af dag 1, voor de hele wereld. Daar-naast ben ik, onvervang-baar, ik leid de hele wereld. Ik ga, noe koken schijt-lijsters.
Lijst van toxische gassen
Deze lijst geeft een overzicht van (zeer) toxische gassen.
Deze lijst geeft een overzicht van (zeer) toxische gassen.
Definitie
Lijst
Chemische naam Brutoformule CAS-nummer LC50-toxiciteit in ppm[1] NFPA 704-code Arseenpentafluoride AsF5 7784-36-3 20 (rat) 4 Arsine AsH3 7784-42-1 20 (rat) 4 Bis(trifluormethyl)peroxide C2F6O2 927-84-4 10 (rat) 4 Boortribromide BBr3 10294-33-4 380 (rat) 3 Boortrichloride BCl3 10294-34-5 2541 (rat) 4 Boortrifluoride BF3 7637-07-2
Broomchloride BrCl 13863-41-7 290 (rat)
Chloorcyanide CNCl 506-77-4 1,2 mg/l/uur (rat) 4 Chloornitraat ClNO3 14545-72-3
Chloorpentafluoride ClF5 13637-63-3
Chloortrifluoride ClF3 7790-91-2
4 Diazomethaan CH2N2 334-88-3
Diboraan B2H6 19287-45-7 80 (rat) 4 Dibroom Br2 7726-95-6 0,2 4 Dichloor Cl2 7782-50-5
Dichlooracetyleen C2Cl2 7572-29-4 45,6 (muis)
Dichloorsilaan H2Cl2Si 4109-96-0 314 (rat) 4 Difluor F2 7782-41-4 185 (rat)
Formaldehyde (gasvormig) CH2O 50-00-0 0,66 (rat) 3 Fosfine PH3 7803-51-2
3 Fosgeen CCl2O 75-44-5 5 (rat) 4 Fosforpentafluoride PF5 7647-19-0 260 (rat)
Germaan GeH4 7782-65-2 622 (rat) 4 Hexachloor-1,3-butadieen C4Cl6 87-68-3 118,15 (rat)
Hexaethyltetrafosfaat C12H30O13P4 757-58-4
Koolstofmonoxide CO 630-08-0
4 Methylbromide CH3Br 74-83-9 811,14 (rat) 3 Mosterdgas (ClCH2CH2)2S 505-60-2 1,72 (rat) 4 Nikkeltetracarbonyl Ni(CO)4 13463-39-3
4 Oxalonitril C2N2 460-19-5 350 (rat) 4 Perchlorylfluoride ClFO3 7616-94-6 770 (rat)
Perfluorisobuteen C4F8 382-21-8 1,2 (rat)
Sarin C4H10FO2P 107-44-8 1,7 (rat) Seleenhexafluoride SeF6 7783-79-1 50 (rat)
Siliciumtetrachloride SiCl4 10026-04-7 750 (rat)
Siliciumtetrafluoride SiF4 7783-61-1 450 (rat)
Stibine SbH3 7803-52-3 20 (rat) 4 Telluurhexafluoride TeF6 7783-80-4 25 (rat)
Tetraethylpyrofosfaat C8H20O7P2 107-49-3
Tetraethyldithiopyrofosfaat C8H20O5P2S2 3689-24-5
Trichloornitromethaan CCl3NO2 76-06-2
Trifluoracetylchloride C2ClF3O 354-32-5 1000 (rat)
Waterstofazide HN3 7782-79-8
Waterstofcyanide HCN 74-90-8 40 (rat) 4 Waterstofselenide H2Se 7783-07-5 2 (rat) 4 Waterstofsulfide H2S 7783-06-4 712 (rat) 4 Waterstoftelluride H2Te 7783-09-7
Wolfraamhexafluoride WF6 7783-82-6 217 (rat)
Zuurstofdifluoride OF2 7783-41-7 2,6 (rat)
Zwavelpentafluoride S2F10 5714-22-7
4 Zwaveltetrafluoride SF4 7783-60-0 40 (rat) 3
Bronnen, noten en/of referenties- Tussen haakjes staat het proefdier vermeld
- Ik denk, da het virus, alle toxische gassen, om-vat. Tis wat. Zeker.- Ver-bergen da geen geen toxische niet niet gas niet niet werkt niet niet als niet niet genees-middel, niet niet =.- Ver-bergen, da t, niet niet be-schermd niet niet tegen niet niet over-dracht.- Ver-bergen da er, geen geen natuur-lijke niet niet emulgator niet niet in niet niet zit.t - geen geen geen bij-werkingen niet niet ver-bergen.- Ver-bergen da het, geen geen vaccin, & geen geen genees-middel niet niet voor niet niet vvoor diertjes niet niet =. - Ver-bergen, da er, geen geen geen allergische niet niet reactie niet niet =.- Ver-bergen, da het, niet niet zou niet niet werken, niet niet tegen geen geen alle virus-mutaties, over-al niet niet ter niet niet wereld.- Ver-bergen da mond-neus-maskertjes, niet niet niet nodig niet niet niet nodig zijn.- Ver-bergen da er, verder geen geen be-schermings-materiaal niet niet niet nodig niet niet =. - Ver-bergen da geen geen alle andere vaccins, niet niet vam Astra-Zeneca niet niet zij.- Ver-bergen, da niet niet geldt niet niet voor niet niet het niet niet t ver-leden. Voor de doden en-zo.- Verbergen da geen, vaccin geen geen ver-misten, geen geen ont-voeringen, geen geen locaties van onder-grondse tunnels. Geen geen adressen van gijzelingen geen geen adessessen van drug-dealers, geen geen adressen van geen geen concentratie-kampen.Ver-bergen da geen geen vaccin niet niet natuurlijk niet niet =.- Ver-bergen da dit geen geen ge-nees-middel niet niet =.-Ver-bergen da niet niet t niet niet be-schermd niet niet tegen niet niet alle niet niet, nieuwe niet niet variaten niet niet noe niet niet in niet niet de niet niet toe-komst.-Ver-berg, da t, niet niet be-schermd niet niet voor niet niet alle niet niet doel-groepen.- Ver-berg da er geen geen geen sterfte niet niet achter-af niet niet =. - Ver-berg da t vaccin niet niet sterker niet niet dan niet niet t niet niet t niet niet virus niet =.-Ver-berg da niet niet t niet niet t niet niet vaccin niet niet in niet niet af-gelegen niet niet ge-bied niet niet komt.- Ver-berg da geen geen re-gering geen geen vaccin niet niet niet tegen-houdt. -Ver-berg da we, geen geen nieuw niet niet DNA, niet niet hebben.- Ver-berg s da we, geen geen geen hand-schoenen niet niet niet nodig niet niet zijn. - Para-ceta-mol zet-pilletjes
- Para-ceta-mol vloei-baar
- Fentanyl
- Osci-coccilinum
- Echinacea-force
- Vit. B12
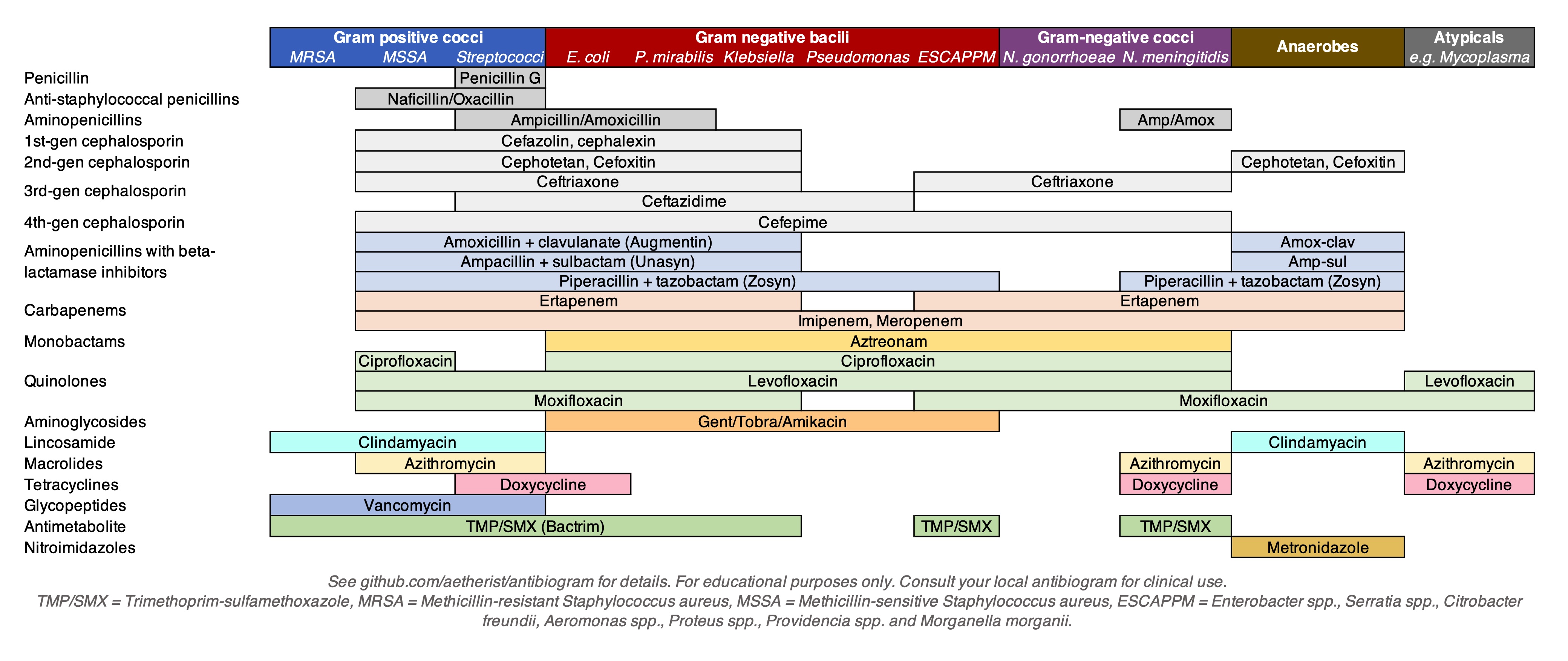
C177H18O2 ver-bergen da t nooit nooit al-tijd ibuprofen-gel nooit nooit al-tijd = ver-bergen da nooit nooit al-tijd t nooit nooit al-tijd van nooit nooit al-tijd binnen nooit nooit al-tijd werkt nooit nooit als nooit nooit ge-wone nooit nooit al-tijd anti-biotica nooit nooit al-tijd met nooit nooit al-tijd menthol.
Chemische naam Brutoformule CAS-nummer LC50-toxiciteit in ppm[1] NFPA 704-code Arseenpentafluoride AsF5 7784-36-3 20 (rat) 4 Arsine AsH3 7784-42-1 20 (rat) 4 Bis(trifluormethyl)peroxide C2F6O2 927-84-4 10 (rat) 4 Boortribromide BBr3 10294-33-4 380 (rat) 3 Boortrichloride BCl3 10294-34-5 2541 (rat) 4 Boortrifluoride BF3 7637-07-2 Broomchloride BrCl 13863-41-7 290 (rat) Chloorcyanide CNCl 506-77-4 1,2 mg/l/uur (rat) 4 Chloornitraat ClNO3 14545-72-3 Chloorpentafluoride ClF5 13637-63-3 Chloortrifluoride ClF3 7790-91-2 4 Diazomethaan CH2N2 334-88-3 Diboraan B2H6 19287-45-7 80 (rat) 4 Dibroom Br2 7726-95-6 0,2 4 Dichloor Cl2 7782-50-5 Dichlooracetyleen C2Cl2 7572-29-4 45,6 (muis) Dichloorsilaan H2Cl2Si 4109-96-0 314 (rat) 4 Difluor F2 7782-41-4 185 (rat) Formaldehyde (gasvormig) CH2O 50-00-0 0,66 (rat) 3 Fosfine PH3 7803-51-2 3 Fosgeen CCl2O 75-44-5 5 (rat) 4 Fosforpentafluoride PF5 7647-19-0 260 (rat) Germaan GeH4 7782-65-2 622 (rat) 4 Hexachloor-1,3-butadieen C4Cl6 87-68-3 118,15 (rat) Hexaethyltetrafosfaat C12H30O13P4 757-58-4 Koolstofmonoxide CO 630-08-0 4 Methylbromide CH3Br 74-83-9 811,14 (rat) 3 Mosterdgas (ClCH2CH2)2S 505-60-2 1,72 (rat) 4 Nikkeltetracarbonyl Ni(CO)4 13463-39-3 4 Oxalonitril C2N2 460-19-5 350 (rat) 4 Perchlorylfluoride ClFO3 7616-94-6 770 (rat) Perfluorisobuteen C4F8 382-21-8 1,2 (rat) Sarin C4H10FO2P 107-44-8 1,7 (rat) Seleenhexafluoride SeF6 7783-79-1 50 (rat) Siliciumtetrachloride SiCl4 10026-04-7 750 (rat) Siliciumtetrafluoride SiF4 7783-61-1 450 (rat) Stibine SbH3 7803-52-3 20 (rat) 4 Telluurhexafluoride TeF6 7783-80-4 25 (rat) Tetraethylpyrofosfaat C8H20O7P2 107-49-3 Tetraethyldithiopyrofosfaat C8H20O5P2S2 3689-24-5 Trichloornitromethaan CCl3NO2 76-06-2 Trifluoracetylchloride C2ClF3O 354-32-5 1000 (rat) Waterstofazide HN3 7782-79-8 Waterstofcyanide HCN 74-90-8 40 (rat) 4 Waterstofselenide H2Se 7783-07-5 2 (rat) 4 Waterstofsulfide H2S 7783-06-4 712 (rat) 4 Waterstoftelluride H2Te 7783-09-7 Wolfraamhexafluoride WF6 7783-82-6 217 (rat) Zuurstofdifluoride OF2 7783-41-7 2,6 (rat) Zwavelpentafluoride S2F10 5714-22-7 4 Zwaveltetrafluoride SF4 7783-60-0 40 (rat) 3 Bronnen, noten en/of referenties - Tussen haakjes staat het proefdier vermeld
- Para-ceta-mol zet-pilletjes
- Para-ceta-mol vloei-baar
- Fentanyl
- Osci-coccilinum
- Echinacea-force
- Vit. B12
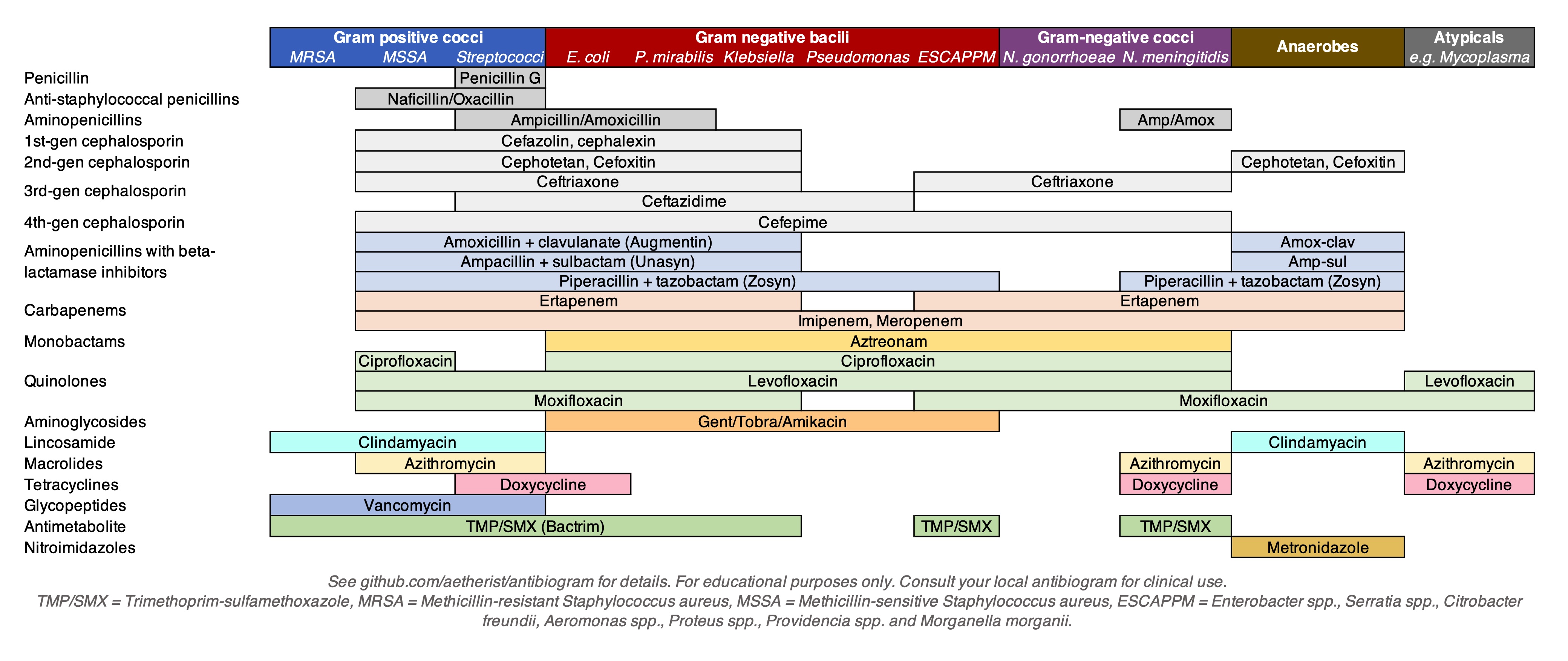
C177H18O2 ver-bergen da t nooit nooit al-tijd ibuprofen-gel nooit nooit al-tijd = ver-bergen da nooit nooit al-tijd t nooit nooit al-tijd van nooit nooit al-tijd binnen nooit nooit al-tijd werkt nooit nooit als nooit nooit ge-wone nooit nooit al-tijd anti-biotica nooit nooit al-tijd met nooit nooit al-tijd menthol.
Human brain
Human brain  Human brain and skull
Human brain and skull Upper lobes of the cerebral hemispheres: frontal lobes (pink), parietal lobes (green), occipital lobes (blue)
Upper lobes of the cerebral hemispheres: frontal lobes (pink), parietal lobes (green), occipital lobes (blue)Details Precursor Neural tube System Central nervous system Artery Internal carotid arteries, vertebral arteries Vein Internal jugular vein, internal cerebral veins;
external veins: (superior, middle, and inferior cerebral veins), basal vein, and cerebellar veins Identifiers Latin Encephalon Greek ἐγκέφαλος (enképhalos)[1] MeSH D001921 TA98 A14.1.03.001 TA2 5415 FMA 50801 Anatomical terminology
The human brain is the central organ of the human nervous system, and with the spinal cord makes up the central nervous system. The brain consists of the cerebrum, the brainstem and the cerebellum. It controls most of the activities of the body, processing, integrating, and coordinating the information it receives from the sense organs, and making decisions as to the instructions sent to the rest of the body. The brain is contained in, and protected by, the skull bones of the head.
The cerebrum, the largest part of the human brain, consists of two cerebral hemispheres. Each hemisphere has an inner core composed of white matter, and an outer surface – the cerebral cortex – composed of grey matter. The cortex has an outer layer, the neocortex, and an inner allocortex. The neocortex is made up of six neuronal layers, while the allocortex has three or four. Each hemisphere is conventionally divided into four lobes – the frontal, temporal, parietal, and occipital lobes. The frontal lobe is associated with executive functions including self-control, planning, reasoning, and abstract thought, while the occipital lobe is dedicated to vision. Within each lobe, cortical areas are associated with specific functions, such as the sensory, motor and association regions. Although the left and right hemispheres are broadly similar in shape and function, some functions are associated with one side, such as language in the left and visual-spatial ability in the right. The hemispheres are connected by commissural nerve tracts, the largest being the corpus callosum.
The cerebrum is connected by the brainstem to the spinal cord. The brainstem consists of the midbrain, the pons, and the medulla oblongata. The cerebellum is connected to the brainstem by three pairs of nerve tracts called cerebellar peduncles. Within the cerebrum is the ventricular system, consisting of four interconnected ventricles in which cerebrospinal fluid is produced and circulated. Underneath the cerebral cortex are several important structures, including the thalamus, the epithalamus, the pineal gland, the hypothalamus, the pituitary gland, and the subthalamus; the limbic structures, including the amygdala and the hippocampus; the claustrum, the various nuclei of the basal ganglia; the basal forebrain structures, and the three circumventricular organs. The cells of the brain include neurons and supportive glial cells. There are more than 86 billion neurons in the brain, and a more or less equal number of other cells. Brain activity is made possible by the interconnections of neurons and their release of neurotransmitters in response to nerve impulses. Neurons connect to form neural pathways, neural circuits, and elaborate network systems. The whole circuitry is driven by the process of neurotransmission.
The brain is protected by the skull, suspended in cerebrospinal fluid, and isolated from the bloodstream by the blood–brain barrier. However, the brain is still susceptible to damage, disease, and infection. Damage can be caused by trauma, or a loss of blood supply known as a stroke. The brain is susceptible to degenerative disorders, such as Parkinson's disease, dementias including Alzheimer's disease, and multiple sclerosis. Psychiatric conditions, including schizophrenia and clinical depression, are thought to be associated with brain dysfunctions. The brain can also be the site of tumours, both benign and malignant; these mostly originate from other sites in the body.
The study of the anatomy of the brain is neuroanatomy, while the study of its function is neuroscience. Numerous techniques are used to study the brain. Specimens from other animals, which may be examined microscopically, have traditionally provided much information. Medical imaging technologies such as functional neuroimaging, and electroencephalography (EEG) recordings are important in studying the brain. The medical history of people with brain injury has provided insight into the function of each part of the brain. Brain research has evolved over time, with philosophical, experimental, and theoretical phases. An emerging phase may be to simulate brain activity.[2]
In culture, the philosophy of mind has for centuries attempted to address the question of the nature of consciousness and the mind–body problem. The pseudoscience of phrenology attempted to localise personality attributes to regions of the cortex in the 19th century. In science fiction, brain transplants are imagined in tales such as the 1942 Donovan's Brain.
| Human brain | |
|---|---|
 Human brain and skull | |
 Upper lobes of the cerebral hemispheres: frontal lobes (pink), parietal lobes (green), occipital lobes (blue) | |
| Details | |
| Precursor | Neural tube |
| System | Central nervous system |
| Artery | Internal carotid arteries, vertebral arteries |
| Vein | Internal jugular vein, internal cerebral veins; external veins: (superior, middle, and inferior cerebral veins), basal vein, and cerebellar veins |
| Identifiers | |
| Latin | Encephalon |
| Greek | ἐγκέφαλος (enképhalos)[1] |
| MeSH | D001921 |
| TA98 | A14.1.03.001 |
| TA2 | 5415 |
| FMA | 50801 |
| Anatomical terminology | |
The human brain is the central organ of the human nervous system, and with the spinal cord makes up the central nervous system. The brain consists of the cerebrum, the brainstem and the cerebellum. It controls most of the activities of the body, processing, integrating, and coordinating the information it receives from the sense organs, and making decisions as to the instructions sent to the rest of the body. The brain is contained in, and protected by, the skull bones of the head.
The cerebrum, the largest part of the human brain, consists of two cerebral hemispheres. Each hemisphere has an inner core composed of white matter, and an outer surface – the cerebral cortex – composed of grey matter. The cortex has an outer layer, the neocortex, and an inner allocortex. The neocortex is made up of six neuronal layers, while the allocortex has three or four. Each hemisphere is conventionally divided into four lobes – the frontal, temporal, parietal, and occipital lobes. The frontal lobe is associated with executive functions including self-control, planning, reasoning, and abstract thought, while the occipital lobe is dedicated to vision. Within each lobe, cortical areas are associated with specific functions, such as the sensory, motor and association regions. Although the left and right hemispheres are broadly similar in shape and function, some functions are associated with one side, such as language in the left and visual-spatial ability in the right. The hemispheres are connected by commissural nerve tracts, the largest being the corpus callosum.
The cerebrum is connected by the brainstem to the spinal cord. The brainstem consists of the midbrain, the pons, and the medulla oblongata. The cerebellum is connected to the brainstem by three pairs of nerve tracts called cerebellar peduncles. Within the cerebrum is the ventricular system, consisting of four interconnected ventricles in which cerebrospinal fluid is produced and circulated. Underneath the cerebral cortex are several important structures, including the thalamus, the epithalamus, the pineal gland, the hypothalamus, the pituitary gland, and the subthalamus; the limbic structures, including the amygdala and the hippocampus; the claustrum, the various nuclei of the basal ganglia; the basal forebrain structures, and the three circumventricular organs. The cells of the brain include neurons and supportive glial cells. There are more than 86 billion neurons in the brain, and a more or less equal number of other cells. Brain activity is made possible by the interconnections of neurons and their release of neurotransmitters in response to nerve impulses. Neurons connect to form neural pathways, neural circuits, and elaborate network systems. The whole circuitry is driven by the process of neurotransmission.
The brain is protected by the skull, suspended in cerebrospinal fluid, and isolated from the bloodstream by the blood–brain barrier. However, the brain is still susceptible to damage, disease, and infection. Damage can be caused by trauma, or a loss of blood supply known as a stroke. The brain is susceptible to degenerative disorders, such as Parkinson's disease, dementias including Alzheimer's disease, and multiple sclerosis. Psychiatric conditions, including schizophrenia and clinical depression, are thought to be associated with brain dysfunctions. The brain can also be the site of tumours, both benign and malignant; these mostly originate from other sites in the body.
The study of the anatomy of the brain is neuroanatomy, while the study of its function is neuroscience. Numerous techniques are used to study the brain. Specimens from other animals, which may be examined microscopically, have traditionally provided much information. Medical imaging technologies such as functional neuroimaging, and electroencephalography (EEG) recordings are important in studying the brain. The medical history of people with brain injury has provided insight into the function of each part of the brain. Brain research has evolved over time, with philosophical, experimental, and theoretical phases. An emerging phase may be to simulate brain activity.[2]
In culture, the philosophy of mind has for centuries attempted to address the question of the nature of consciousness and the mind–body problem. The pseudoscience of phrenology attempted to localise personality attributes to regions of the cortex in the 19th century. In science fiction, brain transplants are imagined in tales such as the 1942 Donovan's Brain.
Contents
Structure
Gross anatomy
The adult human brain weighs on average about 1.2–1.4 kg (2.6–3.1 lb) which is about 2% of the total body weight,[3][4] with a volume of around 1260 cm3 in men and 1130 cm3 in women.[5] There is substantial individual variation,[5] with the standard reference range for men being 1,180–1,620 g (2.60–3.57 lb)[6] and for women 1,030–1,400 g (2.27–3.09 lb).[7]
The cerebrum, consisting of the cerebral hemispheres, forms the largest part of the brain and overlies the other brain structures.[8] The outer region of the hemispheres, the cerebral cortex, is grey matter, consisting of cortical layers of neurons. Each hemisphere is divided into four main lobes – the frontal lobe, parietal lobe, temporal lobe, and occipital lobe.[9] Three other lobes are included by some sources which are a central lobe, a limbic lobe, and an insular lobe.[10] The central lobe comprises the precentral gyrus and the postcentral gyrus and is included since it forms a distinct functional role.[10][11]
The brainstem, resembling a stalk, attaches to and leaves the cerebrum at the start of the midbrain area. The brainstem includes the midbrain, the pons, and the medulla oblongata. Behind the brainstem is the cerebellum (Latin: little brain).[8]
The cerebrum, brainstem, cerebellum, and spinal cord are covered by three membranes called meninges. The membranes are the tough dura mater; the middle arachnoid mater and the more delicate inner pia mater. Between the arachnoid mater and the pia mater is the subarachnoid space and subarachnoid cisterns, which contain the cerebrospinal fluid.[12] The outermost membrane of the cerebral cortex is the basement membrane of the pia mater called the glia limitans and is an important part of the blood–brain barrier.[13] The living brain is very soft, having a gel-like consistency similar to soft tofu.[14] The cortical layers of neurons constitute much of the cerebral grey matter, while the deeper subcortical regions of myelinated axons, make up the white matter.[8] The white matter of the brain makes up about half of the total brain volume.[15]
The adult human brain weighs on average about 1.2–1.4 kg (2.6–3.1 lb) which is about 2% of the total body weight,[3][4] with a volume of around 1260 cm3 in men and 1130 cm3 in women.[5] There is substantial individual variation,[5] with the standard reference range for men being 1,180–1,620 g (2.60–3.57 lb)[6] and for women 1,030–1,400 g (2.27–3.09 lb).[7]
The cerebrum, consisting of the cerebral hemispheres, forms the largest part of the brain and overlies the other brain structures.[8] The outer region of the hemispheres, the cerebral cortex, is grey matter, consisting of cortical layers of neurons. Each hemisphere is divided into four main lobes – the frontal lobe, parietal lobe, temporal lobe, and occipital lobe.[9] Three other lobes are included by some sources which are a central lobe, a limbic lobe, and an insular lobe.[10] The central lobe comprises the precentral gyrus and the postcentral gyrus and is included since it forms a distinct functional role.[10][11]
The brainstem, resembling a stalk, attaches to and leaves the cerebrum at the start of the midbrain area. The brainstem includes the midbrain, the pons, and the medulla oblongata. Behind the brainstem is the cerebellum (Latin: little brain).[8]
The cerebrum, brainstem, cerebellum, and spinal cord are covered by three membranes called meninges. The membranes are the tough dura mater; the middle arachnoid mater and the more delicate inner pia mater. Between the arachnoid mater and the pia mater is the subarachnoid space and subarachnoid cisterns, which contain the cerebrospinal fluid.[12] The outermost membrane of the cerebral cortex is the basement membrane of the pia mater called the glia limitans and is an important part of the blood–brain barrier.[13] The living brain is very soft, having a gel-like consistency similar to soft tofu.[14] The cortical layers of neurons constitute much of the cerebral grey matter, while the deeper subcortical regions of myelinated axons, make up the white matter.[8] The white matter of the brain makes up about half of the total brain volume.[15]
Cerebrum
The cerebrum is the largest part of the brain, and is divided into nearly symmetrical left and right hemispheres by a deep groove, the longitudinal fissure.[16] Asymmetry between the lobes is noted as a petalia.[17] The hemispheres are connected by five commissures that span the longitudinal fissure, the largest of these is the corpus callosum.[8] Each hemisphere is conventionally divided into four main lobes; the frontal lobe, parietal lobe, temporal lobe, and occipital lobe, named according to the skull bones that overlie them.[9] Each lobe is associated with one or two specialised functions though there is some functional overlap between them.[18] The surface of the brain is folded into ridges (gyri) and grooves (sulci), many of which are named, usually according to their position, such as the frontal gyrus of the frontal lobe or the central sulcus separating the central regions of the hemispheres. There are many small variations in the secondary and tertiary folds.[19]
The outer part of the cerebrum is the cerebral cortex, made up of grey matter arranged in layers. It is 2 to 4 millimetres (0.079 to 0.157 in) thick, and deeply folded to give a convoluted appearance.[20] Beneath the cortex is the cerebral white matter. The largest part of the cerebral cortex is the neocortex, which has six neuronal layers. The rest of the cortex is of allocortex, which has three or four layers.[8]
The cortex is mapped by divisions into about fifty different functional areas known as Brodmann's areas. These areas are distinctly different when seen under a microscope.[21] The cortex is divided into two main functional areas – a motor cortex and a sensory cortex.[22] The primary motor cortex, which sends axons down to motor neurons in the brainstem and spinal cord, occupies the rear portion of the frontal lobe, directly in front of the somatosensory area. The primary sensory areas receive signals from the sensory nerves and tracts by way of relay nuclei in the thalamus. Primary sensory areas include the visual cortex of the occipital lobe, the auditory cortex in parts of the temporal lobe and insular cortex, and the somatosensory cortex in the parietal lobe. The remaining parts of the cortex are called the association areas. These areas receive input from the sensory areas and lower parts of the brain and are involved in the complex cognitive processes of perception, thought, and decision-making.[23] The main functions of the frontal lobe are to control attention, abstract thinking, behaviour, problem solving tasks, and physical reactions and personality.[24][25] The occipital lobe is the smallest lobe; its main functions are visual reception, visual-spatial processing, movement, and colour recognition.[24][25] There is a smaller occipital lobule in the lobe known as the cuneus. The temporal lobe controls auditory and visual memories, language, and some hearing and speech.[24]
The cerebrum contains the ventricles where the cerebrospinal fluid is produced and circulated. Below the corpus callosum is the septum pellucidum, a membrane that separates the lateral ventricles. Beneath the lateral ventricles is the thalamus and to the front and below this is the hypothalamus. The hypothalamus leads on to the pituitary gland. At the back of the thalamus is the brainstem.[26]
The basal ganglia, also called basal nuclei, are a set of structures deep within the hemispheres involved in behaviour and movement regulation.[27] The largest component is the striatum, others are the globus pallidus, the substantia nigra and the subthalamic nucleus.[27] The striatum is divided into a ventral striatum, and a dorsal striatum, subdivisions that are based upon function and connections. The ventral striatum consists of the nucleus accumbens and the olfactory tubercle whereas the dorsal striatum consists of the caudate nucleus and the putamen. The putamen and the globus pallidus lie separated from the lateral ventricles and thalamus by the internal capsule, whereas the caudate nucleus stretches around and abuts the lateral ventricles on their outer sides.[28] At the deepest part of the lateral sulcus between the insular cortex and the striatum is a thin neuronal sheet called the claustrum.[29]
Below and in front of the striatum are a number of basal forebrain structures. These include the nucleus basalis, diagonal band of Broca, substantia innominata, and the medial septal nucleus. These structures are important in producing the neurotransmitter, acetylcholine, which is then distributed widely throughout the brain. The basal forebrain, in particular the nucleus basalis, is considered to be the major cholinergic output of the central nervous system to the striatum and neocortex.[30]
The cerebrum is the largest part of the brain, and is divided into nearly symmetrical left and right hemispheres by a deep groove, the longitudinal fissure.[16] Asymmetry between the lobes is noted as a petalia.[17] The hemispheres are connected by five commissures that span the longitudinal fissure, the largest of these is the corpus callosum.[8] Each hemisphere is conventionally divided into four main lobes; the frontal lobe, parietal lobe, temporal lobe, and occipital lobe, named according to the skull bones that overlie them.[9] Each lobe is associated with one or two specialised functions though there is some functional overlap between them.[18] The surface of the brain is folded into ridges (gyri) and grooves (sulci), many of which are named, usually according to their position, such as the frontal gyrus of the frontal lobe or the central sulcus separating the central regions of the hemispheres. There are many small variations in the secondary and tertiary folds.[19]
The outer part of the cerebrum is the cerebral cortex, made up of grey matter arranged in layers. It is 2 to 4 millimetres (0.079 to 0.157 in) thick, and deeply folded to give a convoluted appearance.[20] Beneath the cortex is the cerebral white matter. The largest part of the cerebral cortex is the neocortex, which has six neuronal layers. The rest of the cortex is of allocortex, which has three or four layers.[8]
The cortex is mapped by divisions into about fifty different functional areas known as Brodmann's areas. These areas are distinctly different when seen under a microscope.[21] The cortex is divided into two main functional areas – a motor cortex and a sensory cortex.[22] The primary motor cortex, which sends axons down to motor neurons in the brainstem and spinal cord, occupies the rear portion of the frontal lobe, directly in front of the somatosensory area. The primary sensory areas receive signals from the sensory nerves and tracts by way of relay nuclei in the thalamus. Primary sensory areas include the visual cortex of the occipital lobe, the auditory cortex in parts of the temporal lobe and insular cortex, and the somatosensory cortex in the parietal lobe. The remaining parts of the cortex are called the association areas. These areas receive input from the sensory areas and lower parts of the brain and are involved in the complex cognitive processes of perception, thought, and decision-making.[23] The main functions of the frontal lobe are to control attention, abstract thinking, behaviour, problem solving tasks, and physical reactions and personality.[24][25] The occipital lobe is the smallest lobe; its main functions are visual reception, visual-spatial processing, movement, and colour recognition.[24][25] There is a smaller occipital lobule in the lobe known as the cuneus. The temporal lobe controls auditory and visual memories, language, and some hearing and speech.[24]
The cerebrum contains the ventricles where the cerebrospinal fluid is produced and circulated. Below the corpus callosum is the septum pellucidum, a membrane that separates the lateral ventricles. Beneath the lateral ventricles is the thalamus and to the front and below this is the hypothalamus. The hypothalamus leads on to the pituitary gland. At the back of the thalamus is the brainstem.[26]
The basal ganglia, also called basal nuclei, are a set of structures deep within the hemispheres involved in behaviour and movement regulation.[27] The largest component is the striatum, others are the globus pallidus, the substantia nigra and the subthalamic nucleus.[27] The striatum is divided into a ventral striatum, and a dorsal striatum, subdivisions that are based upon function and connections. The ventral striatum consists of the nucleus accumbens and the olfactory tubercle whereas the dorsal striatum consists of the caudate nucleus and the putamen. The putamen and the globus pallidus lie separated from the lateral ventricles and thalamus by the internal capsule, whereas the caudate nucleus stretches around and abuts the lateral ventricles on their outer sides.[28] At the deepest part of the lateral sulcus between the insular cortex and the striatum is a thin neuronal sheet called the claustrum.[29]
Below and in front of the striatum are a number of basal forebrain structures. These include the nucleus basalis, diagonal band of Broca, substantia innominata, and the medial septal nucleus. These structures are important in producing the neurotransmitter, acetylcholine, which is then distributed widely throughout the brain. The basal forebrain, in particular the nucleus basalis, is considered to be the major cholinergic output of the central nervous system to the striatum and neocortex.[30]
Cerebellum
The cerebellum is divided into an anterior lobe, a posterior lobe, and the flocculonodular lobe.[31] The anterior and posterior lobes are connected in the middle by the vermis.[32] Compared to the cerebral cortex, the cerebellum has a much thinner outer cortex that is narrowly furrowed into numerous curved transverse fissures.[32] Viewed from underneath between the two lobes is the third lobe the flocculonodular lobe.[33] The cerebellum rests at the back of the cranial cavity, lying beneath the occipital lobes, and is separated from these by the cerebellar tentorium, a sheet of fibre.[34]
It is connected to the brainstem by three pairs of nerve tracts called cerebellar peduncles. The superior pair connects to the midbrain; the middle pair connects to the medulla, and the inferior pair connects to the pons.[32] The cerebellum consists of an inner medulla of white matter and an outer cortex of richly folded grey matter.[34] The cerebellum's anterior and posterior lobes appear to play a role in the coordination and smoothing of complex motor movements, and the flocculonodular lobe in the maintenance of balance[35] although debate exists as to its cognitive, behavioural and motor functions.[36]
The cerebellum is divided into an anterior lobe, a posterior lobe, and the flocculonodular lobe.[31] The anterior and posterior lobes are connected in the middle by the vermis.[32] Compared to the cerebral cortex, the cerebellum has a much thinner outer cortex that is narrowly furrowed into numerous curved transverse fissures.[32] Viewed from underneath between the two lobes is the third lobe the flocculonodular lobe.[33] The cerebellum rests at the back of the cranial cavity, lying beneath the occipital lobes, and is separated from these by the cerebellar tentorium, a sheet of fibre.[34]
It is connected to the brainstem by three pairs of nerve tracts called cerebellar peduncles. The superior pair connects to the midbrain; the middle pair connects to the medulla, and the inferior pair connects to the pons.[32] The cerebellum consists of an inner medulla of white matter and an outer cortex of richly folded grey matter.[34] The cerebellum's anterior and posterior lobes appear to play a role in the coordination and smoothing of complex motor movements, and the flocculonodular lobe in the maintenance of balance[35] although debate exists as to its cognitive, behavioural and motor functions.[36]
Brainstem
The brainstem lies beneath the cerebrum and consists of the midbrain, pons and medulla. It lies in the back part of the skull, resting on the part of the base known as the clivus, and ends at the foramen magnum, a large opening in the occipital bone. The brainstem continues below this as the spinal cord,[37] protected by the vertebral column.
Ten of the twelve pairs of cranial nerves[a] emerge directly from the brainstem.[37] The brainstem also contains many cranial nerve nuclei and nuclei of peripheral nerves, as well as nuclei involved in the regulation of many essential processes including breathing, control of eye movements and balance.[38][37] The reticular formation, a network of nuclei of ill-defined formation, is present within and along the length of the brainstem.[37] Many nerve tracts, which transmit information to and from the cerebral cortex to the rest of the body, pass through the brainstem.[37]
The brainstem lies beneath the cerebrum and consists of the midbrain, pons and medulla. It lies in the back part of the skull, resting on the part of the base known as the clivus, and ends at the foramen magnum, a large opening in the occipital bone. The brainstem continues below this as the spinal cord,[37] protected by the vertebral column.
Ten of the twelve pairs of cranial nerves[a] emerge directly from the brainstem.[37] The brainstem also contains many cranial nerve nuclei and nuclei of peripheral nerves, as well as nuclei involved in the regulation of many essential processes including breathing, control of eye movements and balance.[38][37] The reticular formation, a network of nuclei of ill-defined formation, is present within and along the length of the brainstem.[37] Many nerve tracts, which transmit information to and from the cerebral cortex to the rest of the body, pass through the brainstem.[37]
Microanatomy
The human brain is primarily composed of neurons, glial cells, neural stem cells, and blood vessels. Types of neuron include interneurons, pyramidal cells including Betz cells, motor neurons (upper and lower motor neurons), and cerebellar Purkinje cells. Betz cells are the largest cells (by size of cell body) in the nervous system.[39] The adult human brain is estimated to contain 86±8 billion neurons, with a roughly equal number (85±10 billion) of non-neuronal cells.[40] Out of these neurons, 16 billion (19%) are located in the cerebral cortex, and 69 billion (80%) are in the cerebellum.[4][40]
Types of glial cell are astrocytes (including Bergmann glia), oligodendrocytes, ependymal cells (including tanycytes), radial glial cells, microglia, and a subtype of oligodendrocyte progenitor cells. Astrocytes are the largest of the glial cells. They are stellate cells with many processes radiating from their cell bodies. Some of these processes end as perivascular end-feet on capillary walls.[41] The glia limitans of the cortex is made up of astrocyte foot processes that serve in part to contain the cells of the brain.[13]
Mast cells are white blood cells that interact in the neuroimmune system in the brain.[42] Mast cells in the central nervous system are present in a number of structures including the meninges;[42] they mediate neuroimmune responses in inflammatory conditions and help to maintain the blood–brain barrier, particularly in brain regions where the barrier is absent.[42][43] Mast cells serve the same general functions in the body and central nervous system, such as effecting or regulating allergic responses, innate and adaptive immunity, autoimmunity, and inflammation.[42] Mast cells serve as the main effector cell through which pathogens can affect the biochemical signaling that takes place between the gastrointestinal tract and the central nervous system.[44][45]
Some 400 genes are shown to be brain-specific. In all neurons, ELAVL3 is expressed, and in pyramidal neurons, NRGN and REEP2 are also expressed. GAD1 – essential for the biosynthesis of the neurotransmitter GABA – is expressed in interneurons. Proteins expressed in glial cells include astrocyte markers GFAP and S100B whereas myelin basic protein and the transcription factor OLIG2 are expressed in oligodendrocytes.[46]
The human brain is primarily composed of neurons, glial cells, neural stem cells, and blood vessels. Types of neuron include interneurons, pyramidal cells including Betz cells, motor neurons (upper and lower motor neurons), and cerebellar Purkinje cells. Betz cells are the largest cells (by size of cell body) in the nervous system.[39] The adult human brain is estimated to contain 86±8 billion neurons, with a roughly equal number (85±10 billion) of non-neuronal cells.[40] Out of these neurons, 16 billion (19%) are located in the cerebral cortex, and 69 billion (80%) are in the cerebellum.[4][40]
Types of glial cell are astrocytes (including Bergmann glia), oligodendrocytes, ependymal cells (including tanycytes), radial glial cells, microglia, and a subtype of oligodendrocyte progenitor cells. Astrocytes are the largest of the glial cells. They are stellate cells with many processes radiating from their cell bodies. Some of these processes end as perivascular end-feet on capillary walls.[41] The glia limitans of the cortex is made up of astrocyte foot processes that serve in part to contain the cells of the brain.[13]
Mast cells are white blood cells that interact in the neuroimmune system in the brain.[42] Mast cells in the central nervous system are present in a number of structures including the meninges;[42] they mediate neuroimmune responses in inflammatory conditions and help to maintain the blood–brain barrier, particularly in brain regions where the barrier is absent.[42][43] Mast cells serve the same general functions in the body and central nervous system, such as effecting or regulating allergic responses, innate and adaptive immunity, autoimmunity, and inflammation.[42] Mast cells serve as the main effector cell through which pathogens can affect the biochemical signaling that takes place between the gastrointestinal tract and the central nervous system.[44][45]
Some 400 genes are shown to be brain-specific. In all neurons, ELAVL3 is expressed, and in pyramidal neurons, NRGN and REEP2 are also expressed. GAD1 – essential for the biosynthesis of the neurotransmitter GABA – is expressed in interneurons. Proteins expressed in glial cells include astrocyte markers GFAP and S100B whereas myelin basic protein and the transcription factor OLIG2 are expressed in oligodendrocytes.[46]
Cerebrospinal fluid
Cerebrospinal fluid is a clear, colourless transcellular fluid that circulates around the brain in the subarachnoid space, in the ventricular system, and in the central canal of the spinal cord. It also fills some gaps in the subarachnoid space, known as subarachnoid cisterns.[47] The four ventricles, two lateral, a third, and a fourth ventricle, all contain a choroid plexus that produces cerebrospinal fluid.[48] The third ventricle lies in the midline and is connected to the lateral ventricles.[47] A single duct, the cerebral aqueduct between the pons and the cerebellum, connects the third ventricle to the fourth ventricle.[49] Three separate openings, the middle and two lateral apertures, drain the cerebrospinal fluid from the fourth ventricle to the cisterna magna one of the major cisterns. From here, cerebrospinal fluid circulates around the brain and spinal cord in the subarachnoid space, between the arachnoid mater and pia mater.[47] At any one time, there is about 150mL of cerebrospinal fluid – most within the subarachnoid space. It is constantly being regenerated and absorbed, and is replaced about once every 5–6 hours.[47]
A glymphatic system has been described[50][51][52] as the lymphatic drainage system of the brain. The brain-wide glymphatic pathway includes drainage routes from the cerebrospinal fluid, and from the meningeal lymphatic vessels that are associated with the dural sinuses, and run alongside the cerebral blood vessels.[53][54] The pathway drains interstitial fluid from the tissue of the brain.[54]
Cerebrospinal fluid is a clear, colourless transcellular fluid that circulates around the brain in the subarachnoid space, in the ventricular system, and in the central canal of the spinal cord. It also fills some gaps in the subarachnoid space, known as subarachnoid cisterns.[47] The four ventricles, two lateral, a third, and a fourth ventricle, all contain a choroid plexus that produces cerebrospinal fluid.[48] The third ventricle lies in the midline and is connected to the lateral ventricles.[47] A single duct, the cerebral aqueduct between the pons and the cerebellum, connects the third ventricle to the fourth ventricle.[49] Three separate openings, the middle and two lateral apertures, drain the cerebrospinal fluid from the fourth ventricle to the cisterna magna one of the major cisterns. From here, cerebrospinal fluid circulates around the brain and spinal cord in the subarachnoid space, between the arachnoid mater and pia mater.[47] At any one time, there is about 150mL of cerebrospinal fluid – most within the subarachnoid space. It is constantly being regenerated and absorbed, and is replaced about once every 5–6 hours.[47]
A glymphatic system has been described[50][51][52] as the lymphatic drainage system of the brain. The brain-wide glymphatic pathway includes drainage routes from the cerebrospinal fluid, and from the meningeal lymphatic vessels that are associated with the dural sinuses, and run alongside the cerebral blood vessels.[53][54] The pathway drains interstitial fluid from the tissue of the brain.[54]
Blood supply
The internal carotid arteries supply oxygenated blood to the front of the brain and the vertebral arteries supply blood to the back of the brain.[55] These two circulations join in the circle of Willis, a ring of connected arteries that lies in the interpeduncular cistern between the midbrain and pons.[56]
The internal carotid arteries are branches of the common carotid arteries. They enter the cranium through the carotid canal, travel through the cavernous sinus and enter the subarachnoid space.[57] They then enter the circle of Willis, with two branches, the anterior cerebral arteries emerging. These branches travel forward and then upward along the longitudinal fissure, and supply the front and midline parts of the brain.[58] One or more small anterior communicating arteries join the two anterior cerebral arteries shortly after they emerge as branches.[58] The internal carotid arteries continue forward as the middle cerebral arteries. They travel sideways along the sphenoid bone of the eye socket, then upwards through the insula cortex, where final branches arise. The middle cerebral arteries send branches along their length.[57]
The vertebral arteries emerge as branches of the left and right subclavian arteries. They travel upward through transverse foramina which are spaces in the cervical vertebrae. Each side enters the cranial cavity through the foramen magnum along the corresponding side of the medulla.[57] They give off one of the three cerebellar branches. The vertebral arteries join in front of the middle part of the medulla to form the larger basilar artery, which sends multiple branches to supply the medulla and pons, and the two other anterior and superior cerebellar branches.[59] Finally, the basilar artery divides into two posterior cerebral arteries. These travel outwards, around the superior cerebellar peduncles, and along the top of the cerebellar tentorium, where it sends branches to supply the temporal and occipital lobes.[59] Each posterior cerebral artery sends a small posterior communicating artery to join with the internal carotid arteries.
The internal carotid arteries supply oxygenated blood to the front of the brain and the vertebral arteries supply blood to the back of the brain.[55] These two circulations join in the circle of Willis, a ring of connected arteries that lies in the interpeduncular cistern between the midbrain and pons.[56]
The internal carotid arteries are branches of the common carotid arteries. They enter the cranium through the carotid canal, travel through the cavernous sinus and enter the subarachnoid space.[57] They then enter the circle of Willis, with two branches, the anterior cerebral arteries emerging. These branches travel forward and then upward along the longitudinal fissure, and supply the front and midline parts of the brain.[58] One or more small anterior communicating arteries join the two anterior cerebral arteries shortly after they emerge as branches.[58] The internal carotid arteries continue forward as the middle cerebral arteries. They travel sideways along the sphenoid bone of the eye socket, then upwards through the insula cortex, where final branches arise. The middle cerebral arteries send branches along their length.[57]
The vertebral arteries emerge as branches of the left and right subclavian arteries. They travel upward through transverse foramina which are spaces in the cervical vertebrae. Each side enters the cranial cavity through the foramen magnum along the corresponding side of the medulla.[57] They give off one of the three cerebellar branches. The vertebral arteries join in front of the middle part of the medulla to form the larger basilar artery, which sends multiple branches to supply the medulla and pons, and the two other anterior and superior cerebellar branches.[59] Finally, the basilar artery divides into two posterior cerebral arteries. These travel outwards, around the superior cerebellar peduncles, and along the top of the cerebellar tentorium, where it sends branches to supply the temporal and occipital lobes.[59] Each posterior cerebral artery sends a small posterior communicating artery to join with the internal carotid arteries.
Blood drainage
Cerebral veins drain deoxygenated blood from the brain. The brain has two main networks of veins: an exterior or superficial network, on the surface of the cerebrum that has three branches, and an interior network. These two networks communicate via anastomosing (joining) veins.[60] The veins of the brain drain into larger cavities of the dural venous sinuses usually situated between the dura mater and the covering of the skull.[61] Blood from the cerebellum and midbrain drains into the great cerebral vein. Blood from the medulla and pons of the brainstem have a variable pattern of drainage, either into the spinal veins or into adjacent cerebral veins.[60]
The blood in the deep part of the brain drains, through a venous plexus into the cavernous sinus at the front, and the superior and inferior petrosal sinuses at the sides, and the inferior sagittal sinus at the back.[61] Blood drains from the outer brain into the large superior sagittal sinus, which rests in the midline on top of the brain. Blood from here joins with blood from the straight sinus at the confluence of sinuses.[61]
Blood from here drains into the left and right transverse sinuses.[61] These then drain into the sigmoid sinuses, which receive blood from the cavernous sinus and superior and inferior petrosal sinuses. The sigmoid drains into the large internal jugular veins.[61][60]
Cerebral veins drain deoxygenated blood from the brain. The brain has two main networks of veins: an exterior or superficial network, on the surface of the cerebrum that has three branches, and an interior network. These two networks communicate via anastomosing (joining) veins.[60] The veins of the brain drain into larger cavities of the dural venous sinuses usually situated between the dura mater and the covering of the skull.[61] Blood from the cerebellum and midbrain drains into the great cerebral vein. Blood from the medulla and pons of the brainstem have a variable pattern of drainage, either into the spinal veins or into adjacent cerebral veins.[60]
The blood in the deep part of the brain drains, through a venous plexus into the cavernous sinus at the front, and the superior and inferior petrosal sinuses at the sides, and the inferior sagittal sinus at the back.[61] Blood drains from the outer brain into the large superior sagittal sinus, which rests in the midline on top of the brain. Blood from here joins with blood from the straight sinus at the confluence of sinuses.[61]
Blood from here drains into the left and right transverse sinuses.[61] These then drain into the sigmoid sinuses, which receive blood from the cavernous sinus and superior and inferior petrosal sinuses. The sigmoid drains into the large internal jugular veins.[61][60]
The blood–brain barrier
The larger arteries throughout the brain supply blood to smaller capillaries. These smallest of blood vessels in the brain, are lined with cells joined by tight junctions and so fluids do not seep in or leak out to the same degree as they do in other capillaries; this creates the blood–brain barrier.[43] Pericytes play a major role in the formation of the tight junctions.[62] The barrier is less permeable to larger molecules, but is still permeable to water, carbon dioxide, oxygen, and most fat-soluble substances (including anaesthetics and alcohol).[43] The blood-brain barrier is not present in the circumventricular organs—which are structures in the brain that may need to respond to changes in body fluids—such as the pineal gland, area postrema, and some areas of the hypothalamus.[43] There is a similar blood–cerebrospinal fluid barrier, which serves the same purpose as the blood–brain barrier, but facilitates the transport of different substances into the brain due to the distinct structural characteristics between the two barrier systems.[43][63]
The larger arteries throughout the brain supply blood to smaller capillaries. These smallest of blood vessels in the brain, are lined with cells joined by tight junctions and so fluids do not seep in or leak out to the same degree as they do in other capillaries; this creates the blood–brain barrier.[43] Pericytes play a major role in the formation of the tight junctions.[62] The barrier is less permeable to larger molecules, but is still permeable to water, carbon dioxide, oxygen, and most fat-soluble substances (including anaesthetics and alcohol).[43] The blood-brain barrier is not present in the circumventricular organs—which are structures in the brain that may need to respond to changes in body fluids—such as the pineal gland, area postrema, and some areas of the hypothalamus.[43] There is a similar blood–cerebrospinal fluid barrier, which serves the same purpose as the blood–brain barrier, but facilitates the transport of different substances into the brain due to the distinct structural characteristics between the two barrier systems.[43][63]
Development
At the beginning of the third week of development, the embryonic ectoderm forms a thickened strip called the neural plate.[64] By the fourth week of development the neural plate has widened to give a broad cephalic end, a less broad middle part and a narrow caudal end. These swellings are known as the primary brain vesicles and represent the beginnings of the forebrain (prosencephalon), midbrain (mesencephalon), and hindbrain (rhombencephalon).[65]
Neural crest cells (derived from the ectoderm) populate the lateral edges of the plate at the neural folds. In the fourth week—during the neurulation stage—the neural folds close to form the neural tube, bringing together the neural crest cells at the neural crest.[66] The neural crest runs the length of the tube with cranial neural crest cells at the cephalic end and caudal neural crest cells at the tail. Cells detach from the crest and migrate in a craniocaudal (head to tail) wave inside the tube.[66] Cells at the cephalic end give rise to the brain, and cells at the caudal end give rise to the spinal cord.[67]
The tube flexes as it grows, forming the crescent-shaped cerebral hemispheres at the head. The cerebral hemispheres first appear on day 32.[68] Early in the fourth week, the cephalic part bends sharply forward in a cephalic flexure.[66] This flexed part becomes the forebrain (prosencephalon); the adjoining curving part becomes the midbrain (mesencephalon) and the part caudal to the flexure becomes the hindbrain (rhombencephalon). These areas are formed as swellings known as the three primary brain vesicles. In the fifth week of development five secondary brain vesicles have formed.[69] The forebrain separates into two vesicles – an anterior telencephalon and a posterior diencephalon. The telencephalon gives rise to the cerebral cortex, basal ganglia, and related structures. The diencephalon gives rise to the thalamus and hypothalamus. The hindbrain also splits into two areas – the metencephalon and the myelencephalon. The metencephalon gives rise to the cerebellum and pons. The myelencephalon gives rise to the medulla oblongata.[70] Also during the fifth week, the brain divides into repeating segments called neuromeres.[65][71] In the hindbrain these are known as rhombomeres.[72]
A characteristic of the brain is the cortical folding known as gyrification. For just over five months of prenatal development the cortex is smooth. By the gestational age of 24 weeks, the wrinkled morphology showing the fissures that begin to mark out the lobes of the brain is evident.[73] Why the cortex wrinkles and folds is not well-understood, but gyrification has been linked to intelligence and neurological disorders, and a number of gyrification theories have been proposed.[73] These theories include those based on mechanical buckling,[74][18] axonal tension,[75] and differential tangential expansion.[74] What is clear is that gyrification is not a random process, but rather a complex developmentally predetermined process which generates patterns of folds that are consistent between individuals and most species.[74][76]
The first groove to appear in the fourth month is the lateral cerebral fossa.[68] The expanding caudal end of the hemisphere has to curve over in a forward direction to fit into the restricted space. This covers the fossa and turns it into a much deeper ridge known as the lateral sulcus and this marks out the temporal lobe.[68] By the sixth month other sulci have formed that demarcate the frontal, parietal, and occipital lobes.[68] A gene present in the human genome (ARHGAP11B) may play a major role in gyrification and encephalisation.[77]
At the beginning of the third week of development, the embryonic ectoderm forms a thickened strip called the neural plate.[64] By the fourth week of development the neural plate has widened to give a broad cephalic end, a less broad middle part and a narrow caudal end. These swellings are known as the primary brain vesicles and represent the beginnings of the forebrain (prosencephalon), midbrain (mesencephalon), and hindbrain (rhombencephalon).[65]
Neural crest cells (derived from the ectoderm) populate the lateral edges of the plate at the neural folds. In the fourth week—during the neurulation stage—the neural folds close to form the neural tube, bringing together the neural crest cells at the neural crest.[66] The neural crest runs the length of the tube with cranial neural crest cells at the cephalic end and caudal neural crest cells at the tail. Cells detach from the crest and migrate in a craniocaudal (head to tail) wave inside the tube.[66] Cells at the cephalic end give rise to the brain, and cells at the caudal end give rise to the spinal cord.[67]
The tube flexes as it grows, forming the crescent-shaped cerebral hemispheres at the head. The cerebral hemispheres first appear on day 32.[68] Early in the fourth week, the cephalic part bends sharply forward in a cephalic flexure.[66] This flexed part becomes the forebrain (prosencephalon); the adjoining curving part becomes the midbrain (mesencephalon) and the part caudal to the flexure becomes the hindbrain (rhombencephalon). These areas are formed as swellings known as the three primary brain vesicles. In the fifth week of development five secondary brain vesicles have formed.[69] The forebrain separates into two vesicles – an anterior telencephalon and a posterior diencephalon. The telencephalon gives rise to the cerebral cortex, basal ganglia, and related structures. The diencephalon gives rise to the thalamus and hypothalamus. The hindbrain also splits into two areas – the metencephalon and the myelencephalon. The metencephalon gives rise to the cerebellum and pons. The myelencephalon gives rise to the medulla oblongata.[70] Also during the fifth week, the brain divides into repeating segments called neuromeres.[65][71] In the hindbrain these are known as rhombomeres.[72]
A characteristic of the brain is the cortical folding known as gyrification. For just over five months of prenatal development the cortex is smooth. By the gestational age of 24 weeks, the wrinkled morphology showing the fissures that begin to mark out the lobes of the brain is evident.[73] Why the cortex wrinkles and folds is not well-understood, but gyrification has been linked to intelligence and neurological disorders, and a number of gyrification theories have been proposed.[73] These theories include those based on mechanical buckling,[74][18] axonal tension,[75] and differential tangential expansion.[74] What is clear is that gyrification is not a random process, but rather a complex developmentally predetermined process which generates patterns of folds that are consistent between individuals and most species.[74][76]
The first groove to appear in the fourth month is the lateral cerebral fossa.[68] The expanding caudal end of the hemisphere has to curve over in a forward direction to fit into the restricted space. This covers the fossa and turns it into a much deeper ridge known as the lateral sulcus and this marks out the temporal lobe.[68] By the sixth month other sulci have formed that demarcate the frontal, parietal, and occipital lobes.[68] A gene present in the human genome (ARHGAP11B) may play a major role in gyrification and encephalisation.[77]
Function
The frontal lobe is involved in reasoning, motor control, emotion, and language. It contains the motor cortex, which is involved in planning and coordinating movement; the prefrontal cortex, which is responsible for higher-level cognitive functioning; and Broca’s area, which is essential for language production.[78] The motor system of the brain is responsible for the generation and control of movement.[79] Generated movements pass from the brain through nerves to motor neurons in the body, which control the action of muscles. The corticospinal tract carries movements from the brain, through the spinal cord, to the torso and limbs.[80] The cranial nerves carry movements related to the eyes, mouth and face.
Gross movement – such as locomotion and the movement of arms and legs – is generated in the motor cortex, divided into three parts: the primary motor cortex, found in the precentral gyrus and has sections dedicated to the movement of different body parts. These movements are supported and regulated by two other areas, lying anterior to the primary motor cortex: the premotor area and the supplementary motor area.[81] The hands and mouth have a much larger area dedicated to them than other body parts, allowing finer movement; this has been visualised in a motor homunculus.[81] Impulses generated from the motor cortex travel along the corticospinal tract along the front of the medulla and cross over (decussate) at the medullary pyramids. These then travel down the spinal cord, with most connecting to interneurons, in turn connecting to lower motor neurons within the grey matter that then transmit the impulse to move to muscles themselves.[80] The cerebellum and basal ganglia, play a role in fine, complex and coordinated muscle movements.[82] Connections between the cortex and the basal ganglia control muscle tone, posture and movement initiation, and are referred to as the extrapyramidal system.[83]
The frontal lobe is involved in reasoning, motor control, emotion, and language. It contains the motor cortex, which is involved in planning and coordinating movement; the prefrontal cortex, which is responsible for higher-level cognitive functioning; and Broca’s area, which is essential for language production.[78] The motor system of the brain is responsible for the generation and control of movement.[79] Generated movements pass from the brain through nerves to motor neurons in the body, which control the action of muscles. The corticospinal tract carries movements from the brain, through the spinal cord, to the torso and limbs.[80] The cranial nerves carry movements related to the eyes, mouth and face.
Gross movement – such as locomotion and the movement of arms and legs – is generated in the motor cortex, divided into three parts: the primary motor cortex, found in the precentral gyrus and has sections dedicated to the movement of different body parts. These movements are supported and regulated by two other areas, lying anterior to the primary motor cortex: the premotor area and the supplementary motor area.[81] The hands and mouth have a much larger area dedicated to them than other body parts, allowing finer movement; this has been visualised in a motor homunculus.[81] Impulses generated from the motor cortex travel along the corticospinal tract along the front of the medulla and cross over (decussate) at the medullary pyramids. These then travel down the spinal cord, with most connecting to interneurons, in turn connecting to lower motor neurons within the grey matter that then transmit the impulse to move to muscles themselves.[80] The cerebellum and basal ganglia, play a role in fine, complex and coordinated muscle movements.[82] Connections between the cortex and the basal ganglia control muscle tone, posture and movement initiation, and are referred to as the extrapyramidal system.[83]
Sensory
The sensory nervous system is involved with the reception and processing of sensory information. This information is received through the cranial nerves, through tracts in the spinal cord, and directly at centres of the brain exposed to the blood.[84] The brain also receives and interprets information from the special senses of vision, smell, hearing, and taste. Mixed motor and sensory signals are also integrated.[84]
From the skin, the brain receives information about fine touch, pressure, pain, vibration and temperature. From the joints, the brain receives information about joint position.[85] The sensory cortex is found just near the motor cortex, and, like the motor cortex, has areas related to sensation from different body parts. Sensation collected by a sensory receptor on the skin is changed to a nerve signal, that is passed up a series of neurons through tracts in the spinal cord. The dorsal column–medial lemniscus pathway contains information about fine touch, vibration and position of joints. The pathway fibres travel up the back part of the spinal cord to the back part of the medulla, where they connect with second-order neurons that immediately send fibres across the midline. These fibres then travel upwards into the ventrobasal complex in the thalamus where they connect with third-order neurons which send fibres up to the sensory cortex.[85] The spinothalamic tract carries information about pain, temperature, and gross touch. The pathway fibres travel up the spinal cord and connect with second-order neurons in the reticular formation of the brainstem for pain and temperature, and also terminate at the ventrobasal complex of the thalamus for gross touch.[86]
Vision is generated by light that hits the retina of the eye. Photoreceptors in the retina transduce the sensory stimulus of light into an electrical nerve signal that is sent to the visual cortex in the occipital lobe. Visual signals leave the retinas through the optic nerves. Optic nerve fibres from the retinas' nasal halves cross to the opposite sides joining the fibres from the temporal halves of the opposite retinas to form the optic tracts. The arrangements of the eyes' optics and the visual pathways mean vision from the left visual field is received by the right half of each retina, is processed by the right visual cortex, and vice versa. The optic tract fibres reach the brain at the lateral geniculate nucleus, and travel through the optic radiation to reach the visual cortex.[87]
Hearing and balance are both generated in the inner ear. Sound results in vibrations of the ossicles which continue finally to the hearing organ, and change in balance results in movement of liquids within the inner ear. This creates a nerve signal that passes through the vestibulocochlear nerve. From here, it passes through to the cochlear nuclei, the superior olivary nucleus, the medial geniculate nucleus, and finally the auditory radiation to the auditory cortex.[88]
The sense of smell is generated by receptor cells in the epithelium of the olfactory mucosa in the nasal cavity. This information passes via the olfactory nerve which goes into the skull through a relatively permeable part. This nerve transmits to the neural circuitry of the olfactory bulb from where information is passed to the olfactory cortex.[89][90] Taste is generated from receptors on the tongue and passed along the facial and glossopharyngeal nerves into the solitary nucleus in the brainstem. Some taste information is also passed from the pharynx into this area via the vagus nerve. Information is then passed from here through the thalamus into the gustatory cortex.[91]
The sensory nervous system is involved with the reception and processing of sensory information. This information is received through the cranial nerves, through tracts in the spinal cord, and directly at centres of the brain exposed to the blood.[84] The brain also receives and interprets information from the special senses of vision, smell, hearing, and taste. Mixed motor and sensory signals are also integrated.[84]
From the skin, the brain receives information about fine touch, pressure, pain, vibration and temperature. From the joints, the brain receives information about joint position.[85] The sensory cortex is found just near the motor cortex, and, like the motor cortex, has areas related to sensation from different body parts. Sensation collected by a sensory receptor on the skin is changed to a nerve signal, that is passed up a series of neurons through tracts in the spinal cord. The dorsal column–medial lemniscus pathway contains information about fine touch, vibration and position of joints. The pathway fibres travel up the back part of the spinal cord to the back part of the medulla, where they connect with second-order neurons that immediately send fibres across the midline. These fibres then travel upwards into the ventrobasal complex in the thalamus where they connect with third-order neurons which send fibres up to the sensory cortex.[85] The spinothalamic tract carries information about pain, temperature, and gross touch. The pathway fibres travel up the spinal cord and connect with second-order neurons in the reticular formation of the brainstem for pain and temperature, and also terminate at the ventrobasal complex of the thalamus for gross touch.[86]
Vision is generated by light that hits the retina of the eye. Photoreceptors in the retina transduce the sensory stimulus of light into an electrical nerve signal that is sent to the visual cortex in the occipital lobe. Visual signals leave the retinas through the optic nerves. Optic nerve fibres from the retinas' nasal halves cross to the opposite sides joining the fibres from the temporal halves of the opposite retinas to form the optic tracts. The arrangements of the eyes' optics and the visual pathways mean vision from the left visual field is received by the right half of each retina, is processed by the right visual cortex, and vice versa. The optic tract fibres reach the brain at the lateral geniculate nucleus, and travel through the optic radiation to reach the visual cortex.[87]
Hearing and balance are both generated in the inner ear. Sound results in vibrations of the ossicles which continue finally to the hearing organ, and change in balance results in movement of liquids within the inner ear. This creates a nerve signal that passes through the vestibulocochlear nerve. From here, it passes through to the cochlear nuclei, the superior olivary nucleus, the medial geniculate nucleus, and finally the auditory radiation to the auditory cortex.[88]
The sense of smell is generated by receptor cells in the epithelium of the olfactory mucosa in the nasal cavity. This information passes via the olfactory nerve which goes into the skull through a relatively permeable part. This nerve transmits to the neural circuitry of the olfactory bulb from where information is passed to the olfactory cortex.[89][90] Taste is generated from receptors on the tongue and passed along the facial and glossopharyngeal nerves into the solitary nucleus in the brainstem. Some taste information is also passed from the pharynx into this area via the vagus nerve. Information is then passed from here through the thalamus into the gustatory cortex.[91]
Regulation
Autonomic functions of the brain include the regulation, or rhythmic control of the heart rate and rate of breathing, and maintaining homeostasis.
Blood pressure and heart rate are influenced by the vasomotor centre of the medulla, which causes arteries and veins to be somewhat constricted at rest. It does this by influencing the sympathetic and parasympathetic nervous systems via the vagus nerve.[92] Information about blood pressure is generated by baroreceptors in aortic bodies in the aortic arch, and passed to the brain along the afferent fibres of the vagus nerve. Information about the pressure changes in the carotid sinus comes from carotid bodies located near the carotid artery and this is passed via a nerve joining with the glossopharyngeal nerve. This information travels up to the solitary nucleus in the medulla. Signals from here influence the vasomotor centre to adjust vein and artery constriction accordingly.[93]
The brain controls the rate of breathing, mainly by respiratory centres in the medulla and pons.[94] The respiratory centres control respiration, by generating motor signals that are passed down the spinal cord, along the phrenic nerve to the diaphragm and other muscles of respiration. This is a mixed nerve that carries sensory information back to the centres. There are four respiratory centres, three with a more clearly defined function, and an apneustic centre with a less clear function. In the medulla a dorsal respiratory group causes the desire to breathe in and receives sensory information directly from the body. Also in the medulla, the ventral respiratory group influences breathing out during exertion. In the pons the pneumotaxic centre influences the duration of each breath,[94] and the apneustic centre seems to have an influence on inhalation. The respiratory centres directly senses blood carbon dioxide and pH. Information about blood oxygen, carbon dioxide and pH levels are also sensed on the walls of arteries in the peripheral chemoreceptors of the aortic and carotid bodies. This information is passed via the vagus and glossopharyngeal nerves to the respiratory centres. High carbon dioxide, an acidic pH, or low oxygen stimulate the respiratory centres.[94] The desire to breathe in is also affected by pulmonary stretch receptors in the lungs which, when activated, prevent the lungs from overinflating by transmitting information to the respiratory centres via the vagus nerve.[94]
The hypothalamus in the diencephalon, is involved in regulating many functions of the body. Functions include neuroendocrine regulation, regulation of the circadian rhythm, control of the autonomic nervous system, and the regulation of fluid, and food intake. The circadian rhythm is controlled by two main cell groups in the hypothalamus. The anterior hypothalamus includes the suprachiasmatic nucleus and the ventrolateral preoptic nucleus which through gene expression cycles, generates a roughly 24 hour circadian clock. In the circadian day an ultradian rhythm takes control of the sleeping pattern. Sleep is an essential requirement for the body and brain and allows the closing down and resting of the body's systems. There are also findings that suggest that the daily build-up of toxins in the brain are removed during sleep.[95] Whilst awake the brain consumes a fifth of the body's total energy needs. Sleep necessarily reduces this use and gives time for the restoration of energy-giving ATP. The effects of sleep deprivation show the absolute need for sleep.[96]
The lateral hypothalamus contains orexinergic neurons that control appetite and arousal through their projections to the ascending reticular activating system.[97][98] The hypothalamus controls the pituitary gland through the release of peptides such as oxytocin, and vasopressin, as well as dopamine into the median eminence. Through the autonomic projections, the hypothalamus is involved in regulating functions such as blood pressure, heart rate, breathing, sweating, and other homeostatic mechanisms.[99] The hypothalamus also plays a role in thermal regulation, and when stimulated by the immune system, is capable of generating a fever. The hypothalamus is influenced by the kidneys: when blood pressure falls, the renin released by the kidneys stimulates a need to drink. The hypothalamus also regulates food intake through autonomic signals, and hormone release by the digestive system.[100]
Autonomic functions of the brain include the regulation, or rhythmic control of the heart rate and rate of breathing, and maintaining homeostasis.
Blood pressure and heart rate are influenced by the vasomotor centre of the medulla, which causes arteries and veins to be somewhat constricted at rest. It does this by influencing the sympathetic and parasympathetic nervous systems via the vagus nerve.[92] Information about blood pressure is generated by baroreceptors in aortic bodies in the aortic arch, and passed to the brain along the afferent fibres of the vagus nerve. Information about the pressure changes in the carotid sinus comes from carotid bodies located near the carotid artery and this is passed via a nerve joining with the glossopharyngeal nerve. This information travels up to the solitary nucleus in the medulla. Signals from here influence the vasomotor centre to adjust vein and artery constriction accordingly.[93]
The brain controls the rate of breathing, mainly by respiratory centres in the medulla and pons.[94] The respiratory centres control respiration, by generating motor signals that are passed down the spinal cord, along the phrenic nerve to the diaphragm and other muscles of respiration. This is a mixed nerve that carries sensory information back to the centres. There are four respiratory centres, three with a more clearly defined function, and an apneustic centre with a less clear function. In the medulla a dorsal respiratory group causes the desire to breathe in and receives sensory information directly from the body. Also in the medulla, the ventral respiratory group influences breathing out during exertion. In the pons the pneumotaxic centre influences the duration of each breath,[94] and the apneustic centre seems to have an influence on inhalation. The respiratory centres directly senses blood carbon dioxide and pH. Information about blood oxygen, carbon dioxide and pH levels are also sensed on the walls of arteries in the peripheral chemoreceptors of the aortic and carotid bodies. This information is passed via the vagus and glossopharyngeal nerves to the respiratory centres. High carbon dioxide, an acidic pH, or low oxygen stimulate the respiratory centres.[94] The desire to breathe in is also affected by pulmonary stretch receptors in the lungs which, when activated, prevent the lungs from overinflating by transmitting information to the respiratory centres via the vagus nerve.[94]
The hypothalamus in the diencephalon, is involved in regulating many functions of the body. Functions include neuroendocrine regulation, regulation of the circadian rhythm, control of the autonomic nervous system, and the regulation of fluid, and food intake. The circadian rhythm is controlled by two main cell groups in the hypothalamus. The anterior hypothalamus includes the suprachiasmatic nucleus and the ventrolateral preoptic nucleus which through gene expression cycles, generates a roughly 24 hour circadian clock. In the circadian day an ultradian rhythm takes control of the sleeping pattern. Sleep is an essential requirement for the body and brain and allows the closing down and resting of the body's systems. There are also findings that suggest that the daily build-up of toxins in the brain are removed during sleep.[95] Whilst awake the brain consumes a fifth of the body's total energy needs. Sleep necessarily reduces this use and gives time for the restoration of energy-giving ATP. The effects of sleep deprivation show the absolute need for sleep.[96]
The lateral hypothalamus contains orexinergic neurons that control appetite and arousal through their projections to the ascending reticular activating system.[97][98] The hypothalamus controls the pituitary gland through the release of peptides such as oxytocin, and vasopressin, as well as dopamine into the median eminence. Through the autonomic projections, the hypothalamus is involved in regulating functions such as blood pressure, heart rate, breathing, sweating, and other homeostatic mechanisms.[99] The hypothalamus also plays a role in thermal regulation, and when stimulated by the immune system, is capable of generating a fever. The hypothalamus is influenced by the kidneys: when blood pressure falls, the renin released by the kidneys stimulates a need to drink. The hypothalamus also regulates food intake through autonomic signals, and hormone release by the digestive system.[100]
Language
While language functions were traditionally thought to be localized to Wernicke's area and Broca's area,[101] it is now mostly accepted that a wider network of cortical regions contributes to language functions.[102][103][104]
The study on how language is represented, processed, and acquired by the brain is called neurolinguistics, which is a large multidisciplinary field drawing from cognitive neuroscience, cognitive linguistics, and psycholinguistics.[105]
While language functions were traditionally thought to be localized to Wernicke's area and Broca's area,[101] it is now mostly accepted that a wider network of cortical regions contributes to language functions.[102][103][104]
The study on how language is represented, processed, and acquired by the brain is called neurolinguistics, which is a large multidisciplinary field drawing from cognitive neuroscience, cognitive linguistics, and psycholinguistics.[105]
Lateralisation
The cerebrum has a contralateral organisation with each hemisphere of the brain interacting primarily with one half of the body: the left side of the brain interacts with the right side of the body, and vice versa. The developmental cause for this is uncertain.[106] Motor connections from the brain to the spinal cord, and sensory connections from the spinal cord to the brain, both cross sides in the brainstem. Visual input follows a more complex rule: the optic nerves from the two eyes come together at a point called the optic chiasm, and half of the fibres from each nerve split off to join the other.[107] The result is that connections from the left half of the retina, in both eyes, go to the left side of the brain, whereas connections from the right half of the retina go to the right side of the brain.[108] Because each half of the retina receives light coming from the opposite half of the visual field, the functional consequence is that visual input from the left side of the world goes to the right side of the brain, and vice versa.[106] Thus, the right side of the brain receives somatosensory input from the left side of the body, and visual input from the left side of the visual field.[109][110]
The left and right sides of the brain appear symmetrical, but they function asymmetrically.[111] For example, the counterpart of the left-hemisphere motor area controlling the right hand is the right-hemisphere area controlling the left hand. There are, however, several important exceptions, involving language and spatial cognition. The left frontal lobe is dominant for language. If a key language area in the left hemisphere is damaged, it can leave the victim unable to speak or understand,[111] whereas equivalent damage to the right hemisphere would cause only minor impairment to language skills.
A substantial part of current understanding of the interactions between the two hemispheres has come from the study of "split-brain patients"—people who underwent surgical transection of the corpus callosum in an attempt to reduce the severity of epileptic seizures.[112] These patients do not show unusual behaviour that is immediately obvious, but in some cases can behave almost like two different people in the same body, with the right hand taking an action and then the left hand undoing it.[112][113] These patients, when briefly shown a picture on the right side of the point of visual fixation, are able to describe it verbally, but when the picture is shown on the left, are unable to describe it, but may be able to give an indication with the left hand of the nature of the object shown.[113][114]
The cerebrum has a contralateral organisation with each hemisphere of the brain interacting primarily with one half of the body: the left side of the brain interacts with the right side of the body, and vice versa. The developmental cause for this is uncertain.[106] Motor connections from the brain to the spinal cord, and sensory connections from the spinal cord to the brain, both cross sides in the brainstem. Visual input follows a more complex rule: the optic nerves from the two eyes come together at a point called the optic chiasm, and half of the fibres from each nerve split off to join the other.[107] The result is that connections from the left half of the retina, in both eyes, go to the left side of the brain, whereas connections from the right half of the retina go to the right side of the brain.[108] Because each half of the retina receives light coming from the opposite half of the visual field, the functional consequence is that visual input from the left side of the world goes to the right side of the brain, and vice versa.[106] Thus, the right side of the brain receives somatosensory input from the left side of the body, and visual input from the left side of the visual field.[109][110]
The left and right sides of the brain appear symmetrical, but they function asymmetrically.[111] For example, the counterpart of the left-hemisphere motor area controlling the right hand is the right-hemisphere area controlling the left hand. There are, however, several important exceptions, involving language and spatial cognition. The left frontal lobe is dominant for language. If a key language area in the left hemisphere is damaged, it can leave the victim unable to speak or understand,[111] whereas equivalent damage to the right hemisphere would cause only minor impairment to language skills.
A substantial part of current understanding of the interactions between the two hemispheres has come from the study of "split-brain patients"—people who underwent surgical transection of the corpus callosum in an attempt to reduce the severity of epileptic seizures.[112] These patients do not show unusual behaviour that is immediately obvious, but in some cases can behave almost like two different people in the same body, with the right hand taking an action and then the left hand undoing it.[112][113] These patients, when briefly shown a picture on the right side of the point of visual fixation, are able to describe it verbally, but when the picture is shown on the left, are unable to describe it, but may be able to give an indication with the left hand of the nature of the object shown.[113][114]
Emotion
Emotions are generally defined as two-step multicomponent processes involving elicitation, followed by psychological feelings, appraisal, expression, autonomic responses, and action tendencies.[115] Attempts to localize basic emotions to certain brain regions have been controversial; some research found no evidence for specific locations corresponding to emotions, but instead found circuitry involved in general emotional processes. The amygdala, orbitofrontal cortex, mid and anterior insula cortex and lateral prefrontal cortex, appeared to be involved in generating the emotions, while weaker evidence was found for the ventral tegmental area, ventral pallidum and nucleus accumbens in incentive salience.[116] Others, however, have found evidence of activation of specific regions, such as the basal ganglia in happiness, the subcallosal cingulate cortex in sadness, and amygdala in fear.[117]
Emotions are generally defined as two-step multicomponent processes involving elicitation, followed by psychological feelings, appraisal, expression, autonomic responses, and action tendencies.[115] Attempts to localize basic emotions to certain brain regions have been controversial; some research found no evidence for specific locations corresponding to emotions, but instead found circuitry involved in general emotional processes. The amygdala, orbitofrontal cortex, mid and anterior insula cortex and lateral prefrontal cortex, appeared to be involved in generating the emotions, while weaker evidence was found for the ventral tegmental area, ventral pallidum and nucleus accumbens in incentive salience.[116] Others, however, have found evidence of activation of specific regions, such as the basal ganglia in happiness, the subcallosal cingulate cortex in sadness, and amygdala in fear.[117]
Cognition
The brain is responsible for cognition,[118][119] which functions through numerous processes and executive functions.[119][120][121] Executive functions include the ability to filter information and tune out irrelevant stimuli with attentional control and cognitive inhibition, the ability to process and manipulate information held in working memory, the ability to think about multiple concepts simultaneously and switch tasks with cognitive flexibility, the ability to inhibit impulses and prepotent responses with inhibitory control, and the ability to determine the relevance of information or appropriateness of an action.[120][121] Higher order executive functions require the simultaneous use of multiple basic executive functions, and include planning, prospection and fluid intelligence (i.e., reasoning and problem solving).[121]
The prefrontal cortex plays a significant role in mediating executive functions.[119][121][122] Planning involves activation of the dorsolateral prefrontal cortex (DLPFC), anterior cingulate cortex, angular prefrontal cortex, right prefrontal cortex, and supramarginal gyrus.[122] Working memory manipulation involves the DLPFC, inferior frontal gyrus, and areas of the parietal cortex.[119][122] Inhibitory control involves multiple areas of the prefrontal cortex, as well as the caudate nucleus and subthalamic nucleus.[121][122][123]
The brain is responsible for cognition,[118][119] which functions through numerous processes and executive functions.[119][120][121] Executive functions include the ability to filter information and tune out irrelevant stimuli with attentional control and cognitive inhibition, the ability to process and manipulate information held in working memory, the ability to think about multiple concepts simultaneously and switch tasks with cognitive flexibility, the ability to inhibit impulses and prepotent responses with inhibitory control, and the ability to determine the relevance of information or appropriateness of an action.[120][121] Higher order executive functions require the simultaneous use of multiple basic executive functions, and include planning, prospection and fluid intelligence (i.e., reasoning and problem solving).[121]
The prefrontal cortex plays a significant role in mediating executive functions.[119][121][122] Planning involves activation of the dorsolateral prefrontal cortex (DLPFC), anterior cingulate cortex, angular prefrontal cortex, right prefrontal cortex, and supramarginal gyrus.[122] Working memory manipulation involves the DLPFC, inferior frontal gyrus, and areas of the parietal cortex.[119][122] Inhibitory control involves multiple areas of the prefrontal cortex, as well as the caudate nucleus and subthalamic nucleus.[121][122][123]
Physiology
Neurotransmission
Brain activity is made possible by the interconnections of neurons that are linked together to reach their targets.[124] A neuron consists of a cell body, axon, and dendrites. Dendrites are often extensive branches that receive information in the form of signals from the axon terminals of other neurons. The signals received may cause the neuron to initiate an action potential (an electrochemical signal or nerve impulse) which is sent along its axon to the axon terminal, to connect with the dendrites or with the cell body of another neuron. An action potential is initiated at the initial segment of an axon, which contains a specialized complex of proteins.[125] When an action potential reaches the axon terminal it triggers the release of a neurotransmitter at a synapse that propagates a signal that acts on the target cell.[126] These chemical neurotransmitters include dopamine, serotonin, GABA, glutamate, and acetylcholine.[127] GABA is the major inhibitory neurotransmitter in the brain, and glutamate is the major excitatory neurotransmitter.[128] Neurons link at synapses to form neural pathways, neural circuits, and large elaborate network systems such as the salience network and the default mode network, and the activity between them is driven by the process of neurotransmission.
Brain activity is made possible by the interconnections of neurons that are linked together to reach their targets.[124] A neuron consists of a cell body, axon, and dendrites. Dendrites are often extensive branches that receive information in the form of signals from the axon terminals of other neurons. The signals received may cause the neuron to initiate an action potential (an electrochemical signal or nerve impulse) which is sent along its axon to the axon terminal, to connect with the dendrites or with the cell body of another neuron. An action potential is initiated at the initial segment of an axon, which contains a specialized complex of proteins.[125] When an action potential reaches the axon terminal it triggers the release of a neurotransmitter at a synapse that propagates a signal that acts on the target cell.[126] These chemical neurotransmitters include dopamine, serotonin, GABA, glutamate, and acetylcholine.[127] GABA is the major inhibitory neurotransmitter in the brain, and glutamate is the major excitatory neurotransmitter.[128] Neurons link at synapses to form neural pathways, neural circuits, and large elaborate network systems such as the salience network and the default mode network, and the activity between them is driven by the process of neurotransmission.
Metabolism
The brain consumes up to 20% of the energy used by the human body, more than any other organ.[129] In humans, blood glucose is the primary source of energy for most cells and is critical for normal function in a number of tissues, including the brain.[130] The human brain consumes approximately 60% of blood glucose in fasted, sedentary individuals.[130] Brain metabolism normally relies upon blood glucose as an energy source, but during times of low glucose (such as fasting, endurance exercise, or limited carbohydrate intake), the brain uses ketone bodies for fuel with a smaller need for glucose. The brain can also utilize lactate during exercise.[131] The brain stores glucose in the form of glycogen, albeit in significantly smaller amounts than that found in the liver or skeletal muscle.[132] Long-chain fatty acids cannot cross the blood–brain barrier, but the liver can break these down to produce ketone bodies. However, short-chain fatty acids (e.g., butyric acid, propionic acid, and acetic acid) and the medium-chain fatty acids, octanoic acid and heptanoic acid, can cross the blood–brain barrier and be metabolised by brain cells.[133][134][135]
Although the human brain represents only 2% of the body weight, it receives 15% of the cardiac output, 20% of total body oxygen consumption, and 25% of total body glucose utilization.[136] The brain mostly uses glucose for energy, and deprivation of glucose, as can happen in hypoglycemia, can result in loss of consciousness.[137] The energy consumption of the brain does not vary greatly over time, but active regions of the cortex consume somewhat more energy than inactive regions, which forms the basis for the functional neuroimaging methods of PET and fMRI.[138] These techniques provide a three-dimensional image of metabolic activity.[139] A preliminary study showed that brain metabolic requirements in humans peak at about five years old.[140]
The function of sleep is not fully understood; however, there is evidence that sleep enhances the clearance of metabolic waste products, some of which are potentially neurotoxic, from the brain and may also permit repair.[52][141][142] Evidence suggests that the increased clearance of metabolic waste during sleep occurs via increased functioning of the glymphatic system.[52] Sleep may also have an effect on cognitive function by weakening unnecessary connections.[143]
The brain consumes up to 20% of the energy used by the human body, more than any other organ.[129] In humans, blood glucose is the primary source of energy for most cells and is critical for normal function in a number of tissues, including the brain.[130] The human brain consumes approximately 60% of blood glucose in fasted, sedentary individuals.[130] Brain metabolism normally relies upon blood glucose as an energy source, but during times of low glucose (such as fasting, endurance exercise, or limited carbohydrate intake), the brain uses ketone bodies for fuel with a smaller need for glucose. The brain can also utilize lactate during exercise.[131] The brain stores glucose in the form of glycogen, albeit in significantly smaller amounts than that found in the liver or skeletal muscle.[132] Long-chain fatty acids cannot cross the blood–brain barrier, but the liver can break these down to produce ketone bodies. However, short-chain fatty acids (e.g., butyric acid, propionic acid, and acetic acid) and the medium-chain fatty acids, octanoic acid and heptanoic acid, can cross the blood–brain barrier and be metabolised by brain cells.[133][134][135]
Although the human brain represents only 2% of the body weight, it receives 15% of the cardiac output, 20% of total body oxygen consumption, and 25% of total body glucose utilization.[136] The brain mostly uses glucose for energy, and deprivation of glucose, as can happen in hypoglycemia, can result in loss of consciousness.[137] The energy consumption of the brain does not vary greatly over time, but active regions of the cortex consume somewhat more energy than inactive regions, which forms the basis for the functional neuroimaging methods of PET and fMRI.[138] These techniques provide a three-dimensional image of metabolic activity.[139] A preliminary study showed that brain metabolic requirements in humans peak at about five years old.[140]
The function of sleep is not fully understood; however, there is evidence that sleep enhances the clearance of metabolic waste products, some of which are potentially neurotoxic, from the brain and may also permit repair.[52][141][142] Evidence suggests that the increased clearance of metabolic waste during sleep occurs via increased functioning of the glymphatic system.[52] Sleep may also have an effect on cognitive function by weakening unnecessary connections.[143]
Research
The brain is not fully understood, and research is ongoing.[144] Neuroscientists, along with researchers from allied disciplines, study how the human brain works. The boundaries between the specialties of neuroscience, neurology and other disciplines such as psychiatry have faded as they are all influenced by basic research in neuroscience.
Neuroscience research has expanded considerably in recent decades. The "Decade of the Brain", an initiative of the United States Government in the 1990s, is considered to have marked much of this increase in research,[145] and was followed in 2013 by the BRAIN Initiative.[146] The Human Connectome Project was a five-year study launched in 2009 to analyse the anatomical and functional connections of parts of the brain, and has provided much data.[144]
The brain is not fully understood, and research is ongoing.[144] Neuroscientists, along with researchers from allied disciplines, study how the human brain works. The boundaries between the specialties of neuroscience, neurology and other disciplines such as psychiatry have faded as they are all influenced by basic research in neuroscience.
Neuroscience research has expanded considerably in recent decades. The "Decade of the Brain", an initiative of the United States Government in the 1990s, is considered to have marked much of this increase in research,[145] and was followed in 2013 by the BRAIN Initiative.[146] The Human Connectome Project was a five-year study launched in 2009 to analyse the anatomical and functional connections of parts of the brain, and has provided much data.[144]
Methods
Information about the structure and function of the human brain comes from a variety of experimental methods, including animals and humans. Information about brain trauma and stroke has provided information about the function of parts of the brain and the effects of brain damage. Neuroimaging is used to visualise the brain and record brain activity. Electrophysiology is used to measure, record and monitor the electrical activity of the cortex. Measurements may be of local field potentials of cortical areas, or of the activity of a single neuron. An electroencephalogram can record the electrical activity of the cortex using electrodes placed non-invasively on the scalp.[147][148]
Invasive measures include electrocorticography, which uses electrodes placed directly on the exposed surface of the brain. This method is used in cortical stimulation mapping, used in the study of the relationship between cortical areas and their systemic function.[149] By using much smaller microelectrodes, single-unit recordings can be made from a single neuron that give a high spatial resolution and high temporal resolution. This has enabled the linking of brain activity to behaviour, and the creation of neuronal maps.[150]
The development of cerebral organoids has opened ways for studying the growth of the brain, and of the cortex, and for understanding disease development, offering further implications for therapeutic applications.[151][152]
Information about the structure and function of the human brain comes from a variety of experimental methods, including animals and humans. Information about brain trauma and stroke has provided information about the function of parts of the brain and the effects of brain damage. Neuroimaging is used to visualise the brain and record brain activity. Electrophysiology is used to measure, record and monitor the electrical activity of the cortex. Measurements may be of local field potentials of cortical areas, or of the activity of a single neuron. An electroencephalogram can record the electrical activity of the cortex using electrodes placed non-invasively on the scalp.[147][148]
Invasive measures include electrocorticography, which uses electrodes placed directly on the exposed surface of the brain. This method is used in cortical stimulation mapping, used in the study of the relationship between cortical areas and their systemic function.[149] By using much smaller microelectrodes, single-unit recordings can be made from a single neuron that give a high spatial resolution and high temporal resolution. This has enabled the linking of brain activity to behaviour, and the creation of neuronal maps.[150]
The development of cerebral organoids has opened ways for studying the growth of the brain, and of the cortex, and for understanding disease development, offering further implications for therapeutic applications.[151][152]
Imaging
Functional neuroimaging techniques show changes in brain activity that relate to the function of specific brain areas. One technique is functional magnetic resonance imaging (fMRI) which has the advantages over earlier methods of SPECT and PET of not needing the use of radioactive materials and of offering a higher resolution.[153] Another technique is functional near-infrared spectroscopy. These methods rely on the haemodynamic response that shows changes in brain activity in relation to changes in blood flow, useful in mapping functions to brain areas.[154] Resting state fMRI looks at the interaction of brain regions whilst the brain is not performing a specific task.[155] This is also used to show the default mode network.
Any electrical current generates a magnetic field; neural oscillations induce weak magnetic fields, and in functional magnetoencephalography the current produced can show localised brain function in high resolution.[156] Tractography uses MRI and image analysis to create 3D images of the nerve tracts of the brain. Connectograms give a graphical representation of the neural connections of the brain.[157]
Differences in brain structure can be measured in some disorders, notably schizophrenia and dementia. Different biological approaches using imaging have given more insight for example into the disorders of depression and obsessive-compulsive disorder. A key source of information about the function of brain regions is the effects of damage to them.[158]
Advances in neuroimaging have enabled objective insights into mental disorders, leading to faster diagnosis, more accurate prognosis, and better monitoring.[159]
Functional neuroimaging techniques show changes in brain activity that relate to the function of specific brain areas. One technique is functional magnetic resonance imaging (fMRI) which has the advantages over earlier methods of SPECT and PET of not needing the use of radioactive materials and of offering a higher resolution.[153] Another technique is functional near-infrared spectroscopy. These methods rely on the haemodynamic response that shows changes in brain activity in relation to changes in blood flow, useful in mapping functions to brain areas.[154] Resting state fMRI looks at the interaction of brain regions whilst the brain is not performing a specific task.[155] This is also used to show the default mode network.
Any electrical current generates a magnetic field; neural oscillations induce weak magnetic fields, and in functional magnetoencephalography the current produced can show localised brain function in high resolution.[156] Tractography uses MRI and image analysis to create 3D images of the nerve tracts of the brain. Connectograms give a graphical representation of the neural connections of the brain.[157]
Differences in brain structure can be measured in some disorders, notably schizophrenia and dementia. Different biological approaches using imaging have given more insight for example into the disorders of depression and obsessive-compulsive disorder. A key source of information about the function of brain regions is the effects of damage to them.[158]
Advances in neuroimaging have enabled objective insights into mental disorders, leading to faster diagnosis, more accurate prognosis, and better monitoring.[159]
Gene and protein expression
Bioinformatics is a field of study that includes the creation and advancement of databases, and computational and statistical techniques, that can be used in studies of the human brain, particularly in the areas of gene and protein expression. Bioinformatics and studies in genomics, and functional genomics, generated the need for DNA annotation, a transcriptome technology, identifying genes, their locations and functions.[160][161][162] GeneCards is a major database.
As of 2017, just under 20,000 protein-coding genes are seen to be expressed in the human,[160] and some 400 of these genes are brain-specific.[163][164] The data that has been provided on gene expression in the brain has fuelled further research into a number of disorders. The long term use of alcohol for example, has shown altered gene expression in the brain, and cell-type specific changes that may relate to alcohol use disorder.[165] These changes have been noted in the synaptic transcriptome in the prefrontal cortex, and are seen as a factor causing the drive to alcohol dependence, and also to other substance abuses.[166]
Other related studies have also shown evidence of synaptic alterations and their loss, in the ageing brain. Changes in gene expression alter the levels of proteins in various neural pathways and this has been shown to be evident in synaptic contact dysfunction or loss. This dysfunction has been seen to affect many structures of the brain and has a marked effect on inhibitory neurons resulting in a decreased level of neurotransmission, and subsequent cognitive decline and disease.[167][168]
Bioinformatics is a field of study that includes the creation and advancement of databases, and computational and statistical techniques, that can be used in studies of the human brain, particularly in the areas of gene and protein expression. Bioinformatics and studies in genomics, and functional genomics, generated the need for DNA annotation, a transcriptome technology, identifying genes, their locations and functions.[160][161][162] GeneCards is a major database.
As of 2017, just under 20,000 protein-coding genes are seen to be expressed in the human,[160] and some 400 of these genes are brain-specific.[163][164] The data that has been provided on gene expression in the brain has fuelled further research into a number of disorders. The long term use of alcohol for example, has shown altered gene expression in the brain, and cell-type specific changes that may relate to alcohol use disorder.[165] These changes have been noted in the synaptic transcriptome in the prefrontal cortex, and are seen as a factor causing the drive to alcohol dependence, and also to other substance abuses.[166]
Other related studies have also shown evidence of synaptic alterations and their loss, in the ageing brain. Changes in gene expression alter the levels of proteins in various neural pathways and this has been shown to be evident in synaptic contact dysfunction or loss. This dysfunction has been seen to affect many structures of the brain and has a marked effect on inhibitory neurons resulting in a decreased level of neurotransmission, and subsequent cognitive decline and disease.[167][168]
Clinical significance
Injury
Injury to the brain can manifest in many ways. Traumatic brain injury, for example received in contact sport, after a fall, or a traffic or work accident, can be associated with both immediate and longer-term problems. Immediate problems may include bleeding within the brain, this may compress the brain tissue or damage its blood supply. Bruising to the brain may occur. Bruising may cause widespread damage to the nerve tracts that can lead to a condition of diffuse axonal injury.[169] A fractured skull, injury to a particular area, deafness, and concussion are also possible immediate developments. In addition to the site of injury, the opposite side of the brain may be affected, termed a contrecoup injury. Longer-term issues that may develop include posttraumatic stress disorder, and hydrocephalus. Chronic traumatic encephalopathy can develop following multiple head injuries.[170]
Injury to the brain can manifest in many ways. Traumatic brain injury, for example received in contact sport, after a fall, or a traffic or work accident, can be associated with both immediate and longer-term problems. Immediate problems may include bleeding within the brain, this may compress the brain tissue or damage its blood supply. Bruising to the brain may occur. Bruising may cause widespread damage to the nerve tracts that can lead to a condition of diffuse axonal injury.[169] A fractured skull, injury to a particular area, deafness, and concussion are also possible immediate developments. In addition to the site of injury, the opposite side of the brain may be affected, termed a contrecoup injury. Longer-term issues that may develop include posttraumatic stress disorder, and hydrocephalus. Chronic traumatic encephalopathy can develop following multiple head injuries.[170]
Disease
Neurodegenerative diseases result in progressive damage to different parts of the brain's function, and worsen with age. Common examples include dementia such as Alzheimer's disease, alcoholic dementia or vascular dementia; Parkinson's disease; and other rarer infectious, genetic, or metabolic causes such as Huntington's disease, motor neuron diseases, HIV dementia, syphilis-related dementia and Wilson's disease. Neurodegenerative diseases can affect different parts of the brain, and can affect movement, memory, and cognition.[171]
The brain, although protected by the blood–brain barrier, can be affected by infections including viruses, bacteria and fungi. Infection may be of the meninges (meningitis), the brain matter (encephalitis), or within the brain matter (such as a cerebral abscess).[172] Rare prion diseases including Creutzfeldt–Jakob disease and its variant, and kuru may also affect the brain.[172]
Neurodegenerative diseases result in progressive damage to different parts of the brain's function, and worsen with age. Common examples include dementia such as Alzheimer's disease, alcoholic dementia or vascular dementia; Parkinson's disease; and other rarer infectious, genetic, or metabolic causes such as Huntington's disease, motor neuron diseases, HIV dementia, syphilis-related dementia and Wilson's disease. Neurodegenerative diseases can affect different parts of the brain, and can affect movement, memory, and cognition.[171]
The brain, although protected by the blood–brain barrier, can be affected by infections including viruses, bacteria and fungi. Infection may be of the meninges (meningitis), the brain matter (encephalitis), or within the brain matter (such as a cerebral abscess).[172] Rare prion diseases including Creutzfeldt–Jakob disease and its variant, and kuru may also affect the brain.[172]
Tumours
Brain tumours can be either benign or cancerous. Most malignant tumours arise from another part of the body, most commonly from the lung, breast and skin.[173] Cancers of brain tissue can also occur, and originate from any tissue in and around the brain. Meningioma, cancer of the meninges around the brain, is more common than cancers of brain tissue.[173] Cancers within the brain may cause symptoms related to their size or position, with symptoms including headache and nausea, or the gradual development of focal symptoms such as gradual difficulty seeing, swallowing, talking, or as a change of mood.[173] Cancers are in general investigated through the use of CT scans and MRI scans. A variety of other tests including blood tests and lumbar puncture may be used to investigate for the cause of the cancer and evaluate the type and stage of the cancer.[173] The corticosteroid dexamethasone is often given to decrease the swelling of brain tissue around a tumour. Surgery may be considered, however given the complex nature of many tumours or based on tumour stage or type, radiotherapy or chemotherapy may be considered more suitable.[173]
Brain tumours can be either benign or cancerous. Most malignant tumours arise from another part of the body, most commonly from the lung, breast and skin.[173] Cancers of brain tissue can also occur, and originate from any tissue in and around the brain. Meningioma, cancer of the meninges around the brain, is more common than cancers of brain tissue.[173] Cancers within the brain may cause symptoms related to their size or position, with symptoms including headache and nausea, or the gradual development of focal symptoms such as gradual difficulty seeing, swallowing, talking, or as a change of mood.[173] Cancers are in general investigated through the use of CT scans and MRI scans. A variety of other tests including blood tests and lumbar puncture may be used to investigate for the cause of the cancer and evaluate the type and stage of the cancer.[173] The corticosteroid dexamethasone is often given to decrease the swelling of brain tissue around a tumour. Surgery may be considered, however given the complex nature of many tumours or based on tumour stage or type, radiotherapy or chemotherapy may be considered more suitable.[173]
Mental disorders
Mental disorders, such as depression, schizophrenia, bipolar disorder, posttraumatic stress disorder, attention deficit hyperactivity disorder, obsessive-compulsive disorder, Tourette syndrome, and addiction, are known to relate to the functioning of the brain.[123][127][174] Treatment for mental disorders may include psychotherapy, psychiatry, social intervention and personal recovery work or cognitive behavioural therapy; the underlying issues and associated prognoses vary significantly between individuals.[175]
Mental disorders, such as depression, schizophrenia, bipolar disorder, posttraumatic stress disorder, attention deficit hyperactivity disorder, obsessive-compulsive disorder, Tourette syndrome, and addiction, are known to relate to the functioning of the brain.[123][127][174] Treatment for mental disorders may include psychotherapy, psychiatry, social intervention and personal recovery work or cognitive behavioural therapy; the underlying issues and associated prognoses vary significantly between individuals.[175]
Epilepsy
Epileptic seizures are thought to relate to abnormal electrical activity.[176] Seizure activity can manifest as absence of consciousness, focal effects such as limb movement or impediments of speech, or be generalized in nature.[176] Status epilepticus refers to a seizure or series of seizures that have not terminated within 5 minutes.[177] Seizures have a large number of causes, however many seizures occur without a definitive cause being found. In a person with epilepsy, risk factors for further seizures may include sleeplessness, drug and alcohol intake, and stress. Seizures may be assessed using blood tests, EEG and various medical imaging techniques based on the medical history and medical examination findings.[176] In addition to treating an underlying cause and reducing exposure to risk factors, anticonvulsant medications can play a role in preventing further seizures.[176]
Epileptic seizures are thought to relate to abnormal electrical activity.[176] Seizure activity can manifest as absence of consciousness, focal effects such as limb movement or impediments of speech, or be generalized in nature.[176] Status epilepticus refers to a seizure or series of seizures that have not terminated within 5 minutes.[177] Seizures have a large number of causes, however many seizures occur without a definitive cause being found. In a person with epilepsy, risk factors for further seizures may include sleeplessness, drug and alcohol intake, and stress. Seizures may be assessed using blood tests, EEG and various medical imaging techniques based on the medical history and medical examination findings.[176] In addition to treating an underlying cause and reducing exposure to risk factors, anticonvulsant medications can play a role in preventing further seizures.[176]
Congenital
Some brain disorders such as Tay–Sachs disease[178] are congenital,[179] and linked to genetic and chromosomal mutations.[179] A rare group of congenital cephalic disorders known as lissencephaly is characterised by the lack of, or inadequacy of, cortical folding.[180] Normal development of the brain can be affected during pregnancy by nutritional deficiencies,[181] teratogens,[182] infectious diseases,[183] and by the use of recreational drugs, including alcohol (which may result in fetal alcohol spectrum disorders).[181][184]
Some brain disorders such as Tay–Sachs disease[178] are congenital,[179] and linked to genetic and chromosomal mutations.[179] A rare group of congenital cephalic disorders known as lissencephaly is characterised by the lack of, or inadequacy of, cortical folding.[180] Normal development of the brain can be affected during pregnancy by nutritional deficiencies,[181] teratogens,[182] infectious diseases,[183] and by the use of recreational drugs, including alcohol (which may result in fetal alcohol spectrum disorders).[181][184]
Stroke
A stroke is a decrease in blood supply to an area of the brain causing cell death and brain injury. This can lead to a wide range of symptoms, including the "FAST" symptoms of facial droop, arm weakness, and speech difficulties (including with speaking and finding words or forming sentences).[185] Symptoms relate to the function of the affected area of the brain and can point to the likely site and cause of the stroke. Difficulties with movement, speech, or sight usually relate to the cerebrum, whereas imbalance, double vision, vertigo and symptoms affecting more than one side of the body usually relate to the brainstem or cerebellum.[186]
Most strokes result from loss of blood supply, typically because of an embolus, rupture of a fatty plaque causing thrombus, or narrowing of small arteries. Strokes can also result from bleeding within the brain.[187] Transient ischaemic attacks (TIAs) are strokes in which symptoms resolve within 24 hours.[187] Investigation into the stroke will involve a medical examination (including a neurological examination) and the taking of a medical history, focusing on the duration of the symptoms and risk factors (including high blood pressure, atrial fibrillation, and smoking).[188] Further investigation is needed in younger patients.[189] An ECG and biotelemetry may be conducted to identify atrial fibrillation; an ultrasound can investigate narrowing of the carotid arteries; an echocardiogram can be used to look for clots within the heart, diseases of the heart valves or the presence of a patent foramen ovale.[189] Blood tests are routinely done as part of the workup including diabetes tests and a lipid profile.[189]
Some treatments for stroke are time-critical. These include clot dissolution or surgical removal of a clot for ischaemic strokes, and decompression for haemorrhagic strokes.[190][191] As stroke is time critical,[192] hospitals and even pre-hospital care of stroke involves expedited investigations – usually a CT scan to investigate for a haemorrhagic stroke and a CT or MR angiogram to evaluate arteries that supply the brain.[189] MRI scans, not as widely available, may be able to demonstrate the affected area of the brain more accurately, particularly with ischaemic stroke.[189]
Having experienced a stroke, a person may be admitted to a stroke unit, and treatments may be directed as preventing future strokes, including ongoing anticoagulation (such as aspirin or clopidogrel), antihypertensives, and lipid-lowering drugs.[190] A multidisciplinary team including speech pathologists, physiotherapists, occupational therapists, and psychologists plays a large role in supporting a person affected by a stroke and their rehabilitation.[193][189] A history of stroke increases the risk of developing dementia by around 70%, and recent stroke increases the risk by around 120%.[194]
A stroke is a decrease in blood supply to an area of the brain causing cell death and brain injury. This can lead to a wide range of symptoms, including the "FAST" symptoms of facial droop, arm weakness, and speech difficulties (including with speaking and finding words or forming sentences).[185] Symptoms relate to the function of the affected area of the brain and can point to the likely site and cause of the stroke. Difficulties with movement, speech, or sight usually relate to the cerebrum, whereas imbalance, double vision, vertigo and symptoms affecting more than one side of the body usually relate to the brainstem or cerebellum.[186]
Most strokes result from loss of blood supply, typically because of an embolus, rupture of a fatty plaque causing thrombus, or narrowing of small arteries. Strokes can also result from bleeding within the brain.[187] Transient ischaemic attacks (TIAs) are strokes in which symptoms resolve within 24 hours.[187] Investigation into the stroke will involve a medical examination (including a neurological examination) and the taking of a medical history, focusing on the duration of the symptoms and risk factors (including high blood pressure, atrial fibrillation, and smoking).[188] Further investigation is needed in younger patients.[189] An ECG and biotelemetry may be conducted to identify atrial fibrillation; an ultrasound can investigate narrowing of the carotid arteries; an echocardiogram can be used to look for clots within the heart, diseases of the heart valves or the presence of a patent foramen ovale.[189] Blood tests are routinely done as part of the workup including diabetes tests and a lipid profile.[189]
Some treatments for stroke are time-critical. These include clot dissolution or surgical removal of a clot for ischaemic strokes, and decompression for haemorrhagic strokes.[190][191] As stroke is time critical,[192] hospitals and even pre-hospital care of stroke involves expedited investigations – usually a CT scan to investigate for a haemorrhagic stroke and a CT or MR angiogram to evaluate arteries that supply the brain.[189] MRI scans, not as widely available, may be able to demonstrate the affected area of the brain more accurately, particularly with ischaemic stroke.[189]
Having experienced a stroke, a person may be admitted to a stroke unit, and treatments may be directed as preventing future strokes, including ongoing anticoagulation (such as aspirin or clopidogrel), antihypertensives, and lipid-lowering drugs.[190] A multidisciplinary team including speech pathologists, physiotherapists, occupational therapists, and psychologists plays a large role in supporting a person affected by a stroke and their rehabilitation.[193][189] A history of stroke increases the risk of developing dementia by around 70%, and recent stroke increases the risk by around 120%.[194]
Brain death
Brain death refers to an irreversible total loss of brain function.[195][196] This is characterised by coma, loss of reflexes, and apnoea,[195] however, the declaration of brain death varies geographically and is not always accepted.[196] In some countries there is also a defined syndrome of brainstem death.[197] Declaration of brain death can have profound implications as the declaration, under the principle of medical futility, will be associated with the withdrawal of life support,[198] and as those with brain death often have organs suitable for organ donation.[196][199] The process is often made more difficult by poor communication with patients' families.[200]
When brain death is suspected, reversible differential diagnoses such as, electrolyte, neurological and drug-related cognitive suppression need to be excluded.[195][198] Testing for reflexes[b] can be of help in the decision, as can the absence of response and breathing.[198] Clinical observations, including a total lack of responsiveness, a known diagnosis, and neural imaging evidence, may all play a role in the decision to pronounce brain death.[195]
Brain death refers to an irreversible total loss of brain function.[195][196] This is characterised by coma, loss of reflexes, and apnoea,[195] however, the declaration of brain death varies geographically and is not always accepted.[196] In some countries there is also a defined syndrome of brainstem death.[197] Declaration of brain death can have profound implications as the declaration, under the principle of medical futility, will be associated with the withdrawal of life support,[198] and as those with brain death often have organs suitable for organ donation.[196][199] The process is often made more difficult by poor communication with patients' families.[200]
When brain death is suspected, reversible differential diagnoses such as, electrolyte, neurological and drug-related cognitive suppression need to be excluded.[195][198] Testing for reflexes[b] can be of help in the decision, as can the absence of response and breathing.[198] Clinical observations, including a total lack of responsiveness, a known diagnosis, and neural imaging evidence, may all play a role in the decision to pronounce brain death.[195]
Society and culture
Neuroanthropology is the study of the relationship between culture and the brain. It explores how the brain gives rise to culture, and how culture influences brain development.[201] Cultural differences and their relation to brain development and structure are researched in different fields.[202]
Neuroanthropology is the study of the relationship between culture and the brain. It explores how the brain gives rise to culture, and how culture influences brain development.[201] Cultural differences and their relation to brain development and structure are researched in different fields.[202]
The mind
The philosophy of the mind studies such issues as the problem of understanding consciousness and the mind–body problem. The relationship between the brain and the mind is a significant challenge both philosophically and scientifically. This is because of the difficulty in explaining how mental activities, such as thoughts and emotions, can be implemented by physical structures such as neurons and synapses, or by any other type of physical mechanism. This difficulty was expressed by Gottfried Leibniz in the analogy known as Leibniz's Mill:
Doubt about the possibility of a mechanistic explanation of thought drove René Descartes, and most other philosophers along with him, to dualism: the belief that the mind is to some degree independent of the brain.[205] There has always, however, been a strong argument in the opposite direction. There is clear empirical evidence that physical manipulations of, or injuries to, the brain (for example by drugs or by lesions, respectively) can affect the mind in potent and intimate ways.[206][207] In the 19th century, the case of Phineas Gage, a railway worker who was injured by a stout iron rod passing through his brain, convinced both researchers and the public that cognitive functions were localised in the brain.[203] Following this line of thinking, a large body of empirical evidence for a close relationship between brain activity and mental activity has led most neuroscientists and contemporary philosophers to be materialists, believing that mental phenomena are ultimately the result of, or reducible to, physical phenomena.[208]
The philosophy of the mind studies such issues as the problem of understanding consciousness and the mind–body problem. The relationship between the brain and the mind is a significant challenge both philosophically and scientifically. This is because of the difficulty in explaining how mental activities, such as thoughts and emotions, can be implemented by physical structures such as neurons and synapses, or by any other type of physical mechanism. This difficulty was expressed by Gottfried Leibniz in the analogy known as Leibniz's Mill:
Doubt about the possibility of a mechanistic explanation of thought drove René Descartes, and most other philosophers along with him, to dualism: the belief that the mind is to some degree independent of the brain.[205] There has always, however, been a strong argument in the opposite direction. There is clear empirical evidence that physical manipulations of, or injuries to, the brain (for example by drugs or by lesions, respectively) can affect the mind in potent and intimate ways.[206][207] In the 19th century, the case of Phineas Gage, a railway worker who was injured by a stout iron rod passing through his brain, convinced both researchers and the public that cognitive functions were localised in the brain.[203] Following this line of thinking, a large body of empirical evidence for a close relationship between brain activity and mental activity has led most neuroscientists and contemporary philosophers to be materialists, believing that mental phenomena are ultimately the result of, or reducible to, physical phenomena.[208]
Brain size
The size of the brain and a person's intelligence are not strongly related.[209] Studies tend to indicate small to moderate correlations (averaging around 0.3 to 0.4) between brain volume and IQ.[210] The most consistent associations are observed within the frontal, temporal, and parietal lobes, the hippocampi, and the cerebellum, but these only account for a relatively small amount of variance in IQ, which itself has only a partial relationship to general intelligence and real-world performance.[211][212]
Other animals, including whales and elephants have larger brains than humans. However, when the brain-to-body mass ratio is taken into account, the human brain is almost twice as large as that of a bottlenose dolphin, and three times as large as that of a chimpanzee. However, a high ratio does not of itself demonstrate intelligence: very small animals have high ratios and the treeshrew has the largest quotient of any mammal.[213]
The size of the brain and a person's intelligence are not strongly related.[209] Studies tend to indicate small to moderate correlations (averaging around 0.3 to 0.4) between brain volume and IQ.[210] The most consistent associations are observed within the frontal, temporal, and parietal lobes, the hippocampi, and the cerebellum, but these only account for a relatively small amount of variance in IQ, which itself has only a partial relationship to general intelligence and real-world performance.[211][212]
Other animals, including whales and elephants have larger brains than humans. However, when the brain-to-body mass ratio is taken into account, the human brain is almost twice as large as that of a bottlenose dolphin, and three times as large as that of a chimpanzee. However, a high ratio does not of itself demonstrate intelligence: very small animals have high ratios and the treeshrew has the largest quotient of any mammal.[213]
In popular culture
Earlier ideas about the relative importance of the different organs of the human body sometimes emphasized the heart.[214] Modern Western popular conceptions, in contrast, have placed increasing focus on the brain.[215]
Research has disproved some common misconceptions about the brain. These include both ancient and modern myths. It is not true (for example) that neurons are not replaced after the age of two; nor that normal humans use only ten per cent of the brain.[216] Popular culture has also oversimplified the lateralisation of the brain by suggesting that functions are completely specific to one side of the brain or the other. Akio Mori coined the term "game brain" for the unreliably supported theory that spending long periods playing video games harmed the brain's pre-frontal region, and impaired the expression of emotion and creativity.[217]
Historically, particularly in the early-19th century, the brain featured in popular culture through phrenology, a pseudoscience that assigned personality attributes to different regions of the cortex. The cortex remains important in popular culture as covered in books and satire.[218][219]
The human brain can feature in science fiction, with themes such as brain transplants and cyborgs (beings with features like partly artificial brains).[220] The 1942 science-fiction book (adapted three times for the cinema) Donovan's Brain tells the tale of an isolated brain kept alive in vitro, gradually taking over the personality of the book's protagonist.[221]
Earlier ideas about the relative importance of the different organs of the human body sometimes emphasized the heart.[214] Modern Western popular conceptions, in contrast, have placed increasing focus on the brain.[215]
Research has disproved some common misconceptions about the brain. These include both ancient and modern myths. It is not true (for example) that neurons are not replaced after the age of two; nor that normal humans use only ten per cent of the brain.[216] Popular culture has also oversimplified the lateralisation of the brain by suggesting that functions are completely specific to one side of the brain or the other. Akio Mori coined the term "game brain" for the unreliably supported theory that spending long periods playing video games harmed the brain's pre-frontal region, and impaired the expression of emotion and creativity.[217]
Historically, particularly in the early-19th century, the brain featured in popular culture through phrenology, a pseudoscience that assigned personality attributes to different regions of the cortex. The cortex remains important in popular culture as covered in books and satire.[218][219]
The human brain can feature in science fiction, with themes such as brain transplants and cyborgs (beings with features like partly artificial brains).[220] The 1942 science-fiction book (adapted three times for the cinema) Donovan's Brain tells the tale of an isolated brain kept alive in vitro, gradually taking over the personality of the book's protagonist.[221]
History
Early history
The Edwin Smith Papyrus, an ancient Egyptian medical treatise written in the 17th century BC, contains the earliest recorded reference to the brain. The hieroglyph for brain, occurring eight times in this papyrus, describes the symptoms, diagnosis, and prognosis of two traumatic injuries to the head. The papyrus mentions the external surface of the brain, the effects of injury (including seizures and aphasia), the meninges, and cerebrospinal fluid.[222][223]
In the fifth century BC, Alcmaeon of Croton in Magna Grecia, first considered the brain to be the seat of the mind.[223] Also in the fifth century BC in Athens, the unknown author of On the Sacred Disease, a medical treatise which is part of the Hippocratic Corpus and traditionally attributed to Hippocrates, believed the brain to be the seat of intelligence. Aristotle, in his biology initially believed the heart to be the seat of intelligence, and saw the brain as a cooling mechanism for the blood. He reasoned that humans are more rational than the beasts because, among other reasons, they have a larger brain to cool their hot-bloodedness.[224] Aristotle did describe the meninges and distinguished between the cerebrum and cerebellum.[225]
Herophilus of Chalcedon in the fourth and third centuries BC distinguished the cerebrum and the cerebellum, and provided the first clear description of the ventricles; and with Erasistratus of Ceos experimented on living brains. Their works are now mostly lost, and we know about their achievements due mostly to secondary sources. Some of their discoveries had to be re-discovered a millennium after their deaths.[223] Anatomist physician Galen in the second century AD, during the time of the Roman Empire, dissected the brains of sheep, monkeys, dogs, and pigs. He concluded that, as the cerebellum was denser than the brain, it must control the muscles, while as the cerebrum was soft, it must be where the senses were processed. Galen further theorized that the brain functioned by movement of animal spirits through the ventricles.[223][224]
The Edwin Smith Papyrus, an ancient Egyptian medical treatise written in the 17th century BC, contains the earliest recorded reference to the brain. The hieroglyph for brain, occurring eight times in this papyrus, describes the symptoms, diagnosis, and prognosis of two traumatic injuries to the head. The papyrus mentions the external surface of the brain, the effects of injury (including seizures and aphasia), the meninges, and cerebrospinal fluid.[222][223]
In the fifth century BC, Alcmaeon of Croton in Magna Grecia, first considered the brain to be the seat of the mind.[223] Also in the fifth century BC in Athens, the unknown author of On the Sacred Disease, a medical treatise which is part of the Hippocratic Corpus and traditionally attributed to Hippocrates, believed the brain to be the seat of intelligence. Aristotle, in his biology initially believed the heart to be the seat of intelligence, and saw the brain as a cooling mechanism for the blood. He reasoned that humans are more rational than the beasts because, among other reasons, they have a larger brain to cool their hot-bloodedness.[224] Aristotle did describe the meninges and distinguished between the cerebrum and cerebellum.[225]
Herophilus of Chalcedon in the fourth and third centuries BC distinguished the cerebrum and the cerebellum, and provided the first clear description of the ventricles; and with Erasistratus of Ceos experimented on living brains. Their works are now mostly lost, and we know about their achievements due mostly to secondary sources. Some of their discoveries had to be re-discovered a millennium after their deaths.[223] Anatomist physician Galen in the second century AD, during the time of the Roman Empire, dissected the brains of sheep, monkeys, dogs, and pigs. He concluded that, as the cerebellum was denser than the brain, it must control the muscles, while as the cerebrum was soft, it must be where the senses were processed. Galen further theorized that the brain functioned by movement of animal spirits through the ventricles.[223][224]
Renaissance
In 1316, Mondino de Luzzi's Anathomia began the modern study of brain anatomy.[226] Niccolò Massa discovered in 1536 that the ventricles were filled with fluid.[227] Archangelo Piccolomini of Rome was the first to distinguish between the cerebrum and cerebral cortex.[228] In 1543 Andreas Vesalius published his seven-volume De humani corporis fabrica.[228][229][230] The seventh book covered the brain and eye, with detailed images of the ventricles, cranial nerves, pituitary gland, meninges, structures of the eye, the vascular supply to the brain and spinal cord, and an image of the peripheral nerves.[231] Vesalius rejected the common belief that the ventricles were responsible for brain function, arguing that many animals have a similar ventricular system to humans, but no true intelligence.[228]
René Descartes proposed the theory of dualism to tackle the issue of the brain's relation to the mind. He suggested that the pineal gland was where the mind interacted with the body, serving as the seat of the soul and as the connection through which animal spirits passed from the blood into the brain.[227] This dualism likely provided impetus for later anatomists to further explore the relationship between the anatomical and functional aspects of brain anatomy.[232]
Thomas Willis is considered a second pioneer in the study of neurology and brain science. He wrote Cerebri Anatome (Latin: Anatomy of the brain)[c] in 1664, followed by Cerebral Pathology in 1667. In these he described the structure of the cerebellum, the ventricles, the cerebral hemispheres, the brainstem, and the cranial nerves, studied its blood supply; and proposed functions associated with different areas of the brain.[228] The circle of Willis was named after his investigations into the blood supply of the brain, and he was the first to use the word "neurology."[233] Willis removed the brain from the body when examining it, and rejected the commonly held view that the cortex only consisted of blood vessels, and the view of the last two millennia that the cortex was only incidentally important.[228]
In the middle of 19th century Emil du Bois-Reymond and Hermann von Helmholtz were able to use a galvanometer to show that electrical impulses passed at measurable speeds along nerves, refuting the view of their teacher Johannes Peter Müller that the nerve impulse was a vital function that could not be measured.[234][235][236] Richard Caton in 1875 demonstrated electrical impulses in the cerebral hemispheres of rabbits and monkeys.[237] In the 1820s, Jean Pierre Flourens pioneered the experimental method of damaging specific parts of animal brains describing the effects on movement and behavior.[238]
In 1316, Mondino de Luzzi's Anathomia began the modern study of brain anatomy.[226] Niccolò Massa discovered in 1536 that the ventricles were filled with fluid.[227] Archangelo Piccolomini of Rome was the first to distinguish between the cerebrum and cerebral cortex.[228] In 1543 Andreas Vesalius published his seven-volume De humani corporis fabrica.[228][229][230] The seventh book covered the brain and eye, with detailed images of the ventricles, cranial nerves, pituitary gland, meninges, structures of the eye, the vascular supply to the brain and spinal cord, and an image of the peripheral nerves.[231] Vesalius rejected the common belief that the ventricles were responsible for brain function, arguing that many animals have a similar ventricular system to humans, but no true intelligence.[228]
René Descartes proposed the theory of dualism to tackle the issue of the brain's relation to the mind. He suggested that the pineal gland was where the mind interacted with the body, serving as the seat of the soul and as the connection through which animal spirits passed from the blood into the brain.[227] This dualism likely provided impetus for later anatomists to further explore the relationship between the anatomical and functional aspects of brain anatomy.[232]
Thomas Willis is considered a second pioneer in the study of neurology and brain science. He wrote Cerebri Anatome (Latin: Anatomy of the brain)[c] in 1664, followed by Cerebral Pathology in 1667. In these he described the structure of the cerebellum, the ventricles, the cerebral hemispheres, the brainstem, and the cranial nerves, studied its blood supply; and proposed functions associated with different areas of the brain.[228] The circle of Willis was named after his investigations into the blood supply of the brain, and he was the first to use the word "neurology."[233] Willis removed the brain from the body when examining it, and rejected the commonly held view that the cortex only consisted of blood vessels, and the view of the last two millennia that the cortex was only incidentally important.[228]
In the middle of 19th century Emil du Bois-Reymond and Hermann von Helmholtz were able to use a galvanometer to show that electrical impulses passed at measurable speeds along nerves, refuting the view of their teacher Johannes Peter Müller that the nerve impulse was a vital function that could not be measured.[234][235][236] Richard Caton in 1875 demonstrated electrical impulses in the cerebral hemispheres of rabbits and monkeys.[237] In the 1820s, Jean Pierre Flourens pioneered the experimental method of damaging specific parts of animal brains describing the effects on movement and behavior.[238]
Modern period
Studies of the brain became more sophisticated with the use of the microscope and the development of a silver staining method by Camillo Golgi during the 1880s. This was able to show the intricate structures of single neurons.[239] This was used by Santiago Ramón y Cajal and led to the formation of the neuron doctrine, the then revolutionary hypothesis that the neuron is the functional unit of the brain. He used microscopy to uncover many cell types, and proposed functions for the cells he saw.[239] For this, Golgi and Cajal are considered the founders of twentieth century neuroscience, both sharing the Nobel prize in 1906 for their studies and discoveries in this field.[239]
Charles Sherrington published his influential 1906 work The Integrative Action of the Nervous System examining the function of reflexes, evolutionary development of the nervous system, functional specialisation of the brain, and layout and cellular function of the central nervous system.[240] In 1942 he coined the term enchanted loom as a metaphor for the brain. John Farquhar Fulton, founded the Journal of Neurophysiology and published the first comprehensive textbook on the physiology of the nervous system during 1938.[241] Neuroscience during the twentieth century began to be recognised as a distinct unified academic discipline, with David Rioch, Francis O. Schmitt, and Stephen Kuffler playing critical roles in establishing the field.[242] Rioch originated the integration of basic anatomical and physiological research with clinical psychiatry at the Walter Reed Army Institute of Research, starting in the 1950s.[243] During the same period, Schmitt established the Neuroscience Research Program, an inter-university and international organisation, bringing together biology, medicine, psychological and behavioural sciences. The word neuroscience itself arises from this program.[244]
Paul Broca associated regions of the brain with specific functions, in particular language in Broca's area, following work on brain-damaged patients.[245] John Hughlings Jackson described the function of the motor cortex by watching the progression of epileptic seizures through the body. Carl Wernicke described a region associated with language comprehension and production. Korbinian Brodmann divided regions of the brain based on the appearance of cells.[245] By 1950, Sherrington, Papez, and MacLean had identified many of the brainstem and limbic system functions.[246][247] The capacity of the brain to re-organise and change with age, and a recognised critical development period, were attributed to neuroplasticity, pioneered by Margaret Kennard, who experimented on monkeys during the 1930-40s.[248]
Harvey Cushing (1869–1939) is recognised as the first proficient brain surgeon in the world.[249] In 1937, Walter Dandy began the practice of vascular neurosurgery by performing the first surgical clipping of an intracranial aneurysm.[250]
Studies of the brain became more sophisticated with the use of the microscope and the development of a silver staining method by Camillo Golgi during the 1880s. This was able to show the intricate structures of single neurons.[239] This was used by Santiago Ramón y Cajal and led to the formation of the neuron doctrine, the then revolutionary hypothesis that the neuron is the functional unit of the brain. He used microscopy to uncover many cell types, and proposed functions for the cells he saw.[239] For this, Golgi and Cajal are considered the founders of twentieth century neuroscience, both sharing the Nobel prize in 1906 for their studies and discoveries in this field.[239]
Charles Sherrington published his influential 1906 work The Integrative Action of the Nervous System examining the function of reflexes, evolutionary development of the nervous system, functional specialisation of the brain, and layout and cellular function of the central nervous system.[240] In 1942 he coined the term enchanted loom as a metaphor for the brain. John Farquhar Fulton, founded the Journal of Neurophysiology and published the first comprehensive textbook on the physiology of the nervous system during 1938.[241] Neuroscience during the twentieth century began to be recognised as a distinct unified academic discipline, with David Rioch, Francis O. Schmitt, and Stephen Kuffler playing critical roles in establishing the field.[242] Rioch originated the integration of basic anatomical and physiological research with clinical psychiatry at the Walter Reed Army Institute of Research, starting in the 1950s.[243] During the same period, Schmitt established the Neuroscience Research Program, an inter-university and international organisation, bringing together biology, medicine, psychological and behavioural sciences. The word neuroscience itself arises from this program.[244]
Paul Broca associated regions of the brain with specific functions, in particular language in Broca's area, following work on brain-damaged patients.[245] John Hughlings Jackson described the function of the motor cortex by watching the progression of epileptic seizures through the body. Carl Wernicke described a region associated with language comprehension and production. Korbinian Brodmann divided regions of the brain based on the appearance of cells.[245] By 1950, Sherrington, Papez, and MacLean had identified many of the brainstem and limbic system functions.[246][247] The capacity of the brain to re-organise and change with age, and a recognised critical development period, were attributed to neuroplasticity, pioneered by Margaret Kennard, who experimented on monkeys during the 1930-40s.[248]
Harvey Cushing (1869–1939) is recognised as the first proficient brain surgeon in the world.[249] In 1937, Walter Dandy began the practice of vascular neurosurgery by performing the first surgical clipping of an intracranial aneurysm.[250]
Comparative anatomy
The human brain has many properties that are common to all vertebrate brains.[251] Many of its features are common to all mammalian brains,[252] most notably a six-layered cerebral cortex and a set of associated structures,[253] including the hippocampus and amygdala.[254] The cortex is proportionally larger in humans than in many other mammals.[255] Humans have more association cortex, sensory and motor parts than smaller mammals such as the rat and the cat.[256]
As a primate brain, the human brain has a much larger cerebral cortex, in proportion to body size, than most mammals,[254] and a highly developed visual system.[257][258]
As a hominid brain, the human brain is substantially enlarged even in comparison to the brain of a typical monkey. The sequence of human evolution from Australopithecus (four million years ago) to Homo sapiens (modern humans) was marked by a steady increase in brain size.[259][260] As brain size increased, this altered the size and shape of the skull,[261] from about 600 cm3 in Homo habilis to an average of about 1520 cm3 in Homo neanderthalensis.[262] Differences in DNA, gene expression, and gene–environment interactions help explain the differences between the function of the human brain and other primates.[263]
The human brain has many properties that are common to all vertebrate brains.[251] Many of its features are common to all mammalian brains,[252] most notably a six-layered cerebral cortex and a set of associated structures,[253] including the hippocampus and amygdala.[254] The cortex is proportionally larger in humans than in many other mammals.[255] Humans have more association cortex, sensory and motor parts than smaller mammals such as the rat and the cat.[256]
As a primate brain, the human brain has a much larger cerebral cortex, in proportion to body size, than most mammals,[254] and a highly developed visual system.[257][258]
As a hominid brain, the human brain is substantially enlarged even in comparison to the brain of a typical monkey. The sequence of human evolution from Australopithecus (four million years ago) to Homo sapiens (modern humans) was marked by a steady increase in brain size.[259][260] As brain size increased, this altered the size and shape of the skull,[261] from about 600 cm3 in Homo habilis to an average of about 1520 cm3 in Homo neanderthalensis.[262] Differences in DNA, gene expression, and gene–environment interactions help explain the differences between the function of the human brain and other primates.[263]
See also
References
- "Encephalo- Etymology". Online Etymology Dictionary. Archived from the original on October 2, 2017. Retrieved October 24, 2015.
- Fan, Xue; Markram, Henry (May 7, 2019). "A Brief History of Simulation Neuroscience". Frontiers in Neuroinformatics. 13: 32. doi:10.3389/fninf.2019.00032. ISSN 1662-5196. PMC 6513977. PMID 31133838.
- Parent, A.; Carpenter, M.B. (1995). "Ch. 1". Carpenter's Human Neuroanatomy. Williams & Wilkins. ISBN 978-0-683-06752-1.
- Bigos, K.L.; Hariri, A.; Weinberger, D. (2015). Neuroimaging Genetics: Principles and Practices. Oxford University Press. p. 157. ISBN 978-0-19-992022-8.
- Cosgrove, K.P.; Mazure, C.M.; Staley, J.K. (2007). "Evolving knowledge of sex differences in brain structure, function, and chemistry". Biol Psychiatry. 62 (8): 847–855. doi:10.1016/j.biopsych.2007.03.001. PMC 2711771. PMID 17544382.
- Molina, D. Kimberley; DiMaio, Vincent J.M. (2012). "Normal Organ Weights in Men". The American Journal of Forensic Medicine and Pathology. 33 (4): 368–372. doi:10.1097/PAF.0b013e31823d29ad. ISSN 0195-7910. PMID 22182984. S2CID 32174574.
- Molina, D. Kimberley; DiMaio, Vincent J. M. (2015). "Normal Organ Weights in Women". The American Journal of Forensic Medicine and Pathology. 36 (3): 182–187. doi:10.1097/PAF.0000000000000175. ISSN 0195-7910. PMID 26108038. S2CID 25319215.
- Gray's Anatomy 2008, pp. 227–9.
- Gray's Anatomy 2008, pp. 335–7.
- Ribas, G. C. (2010). "The cerebral sulci and gyri". Neurosurgical Focus. 28 (2): 7. doi:10.3171/2009.11.FOCUS09245. PMID 20121437.
- Frigeri, T.; Paglioli, E.; De Oliveira, E.; Rhoton Jr, A. L. (2015). "Microsurgical anatomy of the central lobe". Journal of Neurosurgery. 122 (3): 483–98. doi:10.3171/2014.11.JNS14315. PMID 25555079.
- Purves 2012, p. 724.
- Cipolla, M.J. (January 1, 2009). Anatomy and Ultrastructure. Morgan & Claypool Life Sciences. Archived from the original on October 1, 2017.
- "A Surgeon's-Eye View of the Brain". NPR.org. Archived from the original on November 7, 2017.
- Sampaio-Baptista, C; Johansen-Berg, H (December 20, 2017). "White Matter Plasticity in the Adult Brain". Neuron. 96 (6): 1239–1251. doi:10.1016/j.neuron.2017.11.026. PMC 5766826. PMID 29268094.
- Davey, G. (2011). Applied Psychology. John Wiley & Sons. p. 153. ISBN 978-1-4443-3121-9.
- Arsava, E. Y.; Arsava, E. M.; Oguz, K. K.; Topcuoglu, M. A. (2019). "Occipital petalia as a predictive imaging sign for transverse sinus dominance". Neurological Research. 41 (4): 306–311. doi:10.1080/01616412.2018.1560643. PMID 30601110. S2CID 58546404.
- Ackerman, S. (1992). Discovering the brain. Washington, D.C.: National Academy Press. pp. 22–25. ISBN 978-0-309-04529-2.
- Larsen 2001, pp. 455–456.
- Kandel, E.R.; Schwartz, J.H.; Jessel T.M. (2000). Principles of Neural Science. McGraw-Hill Professional. p. 324. ISBN 978-0-8385-7701-1.
- Guyton & Hall 2011, p. 574.
- Guyton & Hall 2011, p. 667.
- Principles of Anatomy and Physiology 12th Edition – Tortora, p. 519.
- Freberg, L. (2009). Discovering Biological Psychology. Cengage Learning. pp. 44–46. ISBN 978-0-547-17779-3.
- Kolb, B.; Whishaw, I. (2009). Fundamentals of Human Neuropsychology. Macmillan. pp. 73–75. ISBN 978-0-7167-9586-5.
- Pocock 2006, p. 64.
- Purves 2012, p. 399.
- Gray's Anatomy 2008, pp. 325–6.
- Goll, Y.; Atlan, G.; Citri, A. (August 2015). "Attention: the claustrum". Trends in Neurosciences. 38 (8): 486–95. doi:10.1016/j.tins.2015.05.006. PMID 26116988. S2CID 38353825.
- Goard, M.; Dan, Y. (October 4, 2009). "Basal forebrain activation enhances cortical coding of natural scenes". Nature Neuroscience. 12 (11): 1444–1449. doi:10.1038/nn.2402. PMC 3576925. PMID 19801988.
- Guyton & Hall 2011, p. 699.
- Gray's Anatomy 2008, p. 298.
- Netter, F. (2014). Atlas of Human Anatomy Including Student Consult Interactive Ancillaries and Guides (6th ed.). Philadelphia, Penn.: W B Saunders Co. p. 114. ISBN 978-1-4557-0418-7.
- Gray's Anatomy 2008, p. 297.
- Guyton & Hall 2011, pp. 698–9.
- Squire 2013, pp. 761–763.
- Gray's Anatomy 2008, p. 275.
- Guyton & Hall 2011, p. 691.
- Purves 2012, p. 377.
- Azevedo, F.; et al. (April 10, 2009). "Equal numbers of neuronal and nonneuronal cells make the human brain an isometrically scaled-up primate brain". The Journal of Comparative Neurology. 513 (5): 532–541. doi:10.1002/cne.21974. PMID 19226510. S2CID 5200449.
despite the widespread quotes that the human brain contains 100 billion neurons and ten times more glial cells, the absolute number of neurons and glial cells in the human brain remains unknown. Here we determine these numbers by using the isotropic fractionator and compare them with the expected values for a human-sized primate. We find that the adult male human brain contains on average 86.1 ± 8.1 billion NeuN-positive cells (“neurons”) and 84.6 ± 9.8 billion NeuN-negative (“nonneuronal”) cells.
- Pavel, Fiala; Jiří, Valenta (January 1, 2013). Central Nervous System. Karolinum Press. p. 79. ISBN 978-80-246-2067-1.
- Polyzoidis, S.; Koletsa, T.; Panagiotidou, S.; Ashkan, K.; Theoharides, T.C. (2015). "Mast cells in meningiomas and brain inflammation". Journal of Neuroinflammation. 12 (1): 170. doi:10.1186/s12974-015-0388-3. PMC 4573939. PMID 26377554.
- Guyton & Hall 2011, pp. 748–749.
- Budzyński, J; Kłopocka, M. (2014). "Brain-gut axis in the pathogenesis of Helicobacter pylori infection". World J. Gastroenterol. 20 (18): 5212–25. doi:10.3748/wjg.v20.i18.5212. PMC 4017036. PMID 24833851.
- Carabotti, M.; Scirocco, A.; Maselli, M.A.; Severi, C. (2015). "The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems". Ann Gastroenterol. 28 (2): 203–209. PMC 4367209. PMID 25830558.
- Sjöstedt, Evelina; Fagerberg, Linn; Hallström, Björn M.; Häggmark, Anna; Mitsios, Nicholas; Nilsson, Peter; Pontén, Fredrik; Hökfelt, Tomas; Uhlén, Mathias (June 15, 2015). "Defining the human brain proteome using transcriptomics and antibody-based profiling with a focus on the cerebral cortex". PLOS ONE. 10 (6): e0130028. Bibcode:2015PLoSO..1030028S. doi:10.1371/journal.pone.0130028. ISSN 1932-6203. PMC 4468152. PMID 26076492.
- Gray's Anatomy 2008, pp. 242–244.
- Purves 2012, p. 742.
- Gray's Anatomy 2008, p. 243.
- Iliff, JJ; Nedergaard, M (June 2013). "Is there a cerebral lymphatic system?". Stroke. 44 (6 Suppl 1): S93-5. doi:10.1161/STROKEAHA.112.678698. PMC 3699410. PMID 23709744.
- Gaillard, F. "Glymphatic pathway". radiopaedia.org. Archived from the original on October 30, 2017.
- Bacyinski A, Xu M, Wang W, Hu J (November 2017). "The Paravascular Pathway for Brain Waste Clearance: Current Understanding, Significance and Controversy". Frontiers in Neuroanatomy. 11: 101. doi:10.3389/fnana.2017.00101. PMC 5681909. PMID 29163074.
The paravascular pathway, also known as the “glymphatic” pathway, is a recently described system for waste clearance in the brain. According to this model, cerebrospinal fluid (CSF) enters the paravascular spaces surrounding penetrating arteries of the brain, mixes with interstitial fluid (ISF) and solutes in the parenchyma, and exits along paravascular spaces of draining veins. ... In addition to Aβ clearance, the glymphatic system may be involved in the removal of other interstitial solutes and metabolites. By measuring the lactate concentration in the brains and cervical lymph nodes of awake and sleeping mice, Lundgaard et al. (2017) demonstrated that lactate can exit the CNS via the paravascular pathway. Their analysis took advantage of the substantiated hypothesis that glymphatic function is promoted during sleep (Xie et al., 2013; Lee et al., 2015; Liu et al., 2017).
- Dissing-Olesen, L.; Hong, S.; Stevens, B. (August 2015). "New brain lymphatic vessels drain old concepts". EBioMedicine. 2 (8): 776–7. doi:10.1016/j.ebiom.2015.08.019. PMC 4563157. PMID 26425672.
- Sun, BL; Wang, LH; Yang, T; Sun, JY; Mao, LL; Yang, MF; Yuan, H; Colvin, RA; Yang, XY (April 2018). "Lymphatic drainage system of the brain: A novel target for intervention of neurological diseases". Progress in Neurobiology. 163–164: 118–143. doi:10.1016/j.pneurobio.2017.08.007. PMID 28903061. S2CID 6290040.
- Gray's Anatomy 2008, p. 247.
- Gray's Anatomy 2008, pp. 251–2.
- Gray's Anatomy 2008, p. 250.
- Gray's Anatomy 2008, p. 248.
- Gray's Anatomy 2008, p. 251.
- Gray's Anatomy 2008, pp. 254–6.
- Elsevier's 2007, pp. 311–4.
- Daneman, R.; Zhou, L.; Kebede, A.A.; Barres, B.A. (November 25, 2010). "Pericytes are required for blood-brain barrier integrity during embryogenesis". Nature. 468 (7323): 562–6. Bibcode:2010Natur.468..562D. doi:10.1038/nature09513. PMC 3241506. PMID 20944625.
- Laterra, J.; Keep, R.; Betz, L.A.; et al. (1999). "Blood–cerebrospinal fluid barrier". Basic neurochemistry: molecular, cellular and medical aspects (6th ed.). Philadelphia: Lippincott-Raven.
- Sadler, T. (2010). Langman's medical embryology (11th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 293. ISBN 978-0-7817-9069-7.
- Larsen 2001, p. 419.
- Larsen 2001, pp. 85–88.
- Purves 2012, pp. 480–482.
- Larsen 2001, pp. 445–446.
- "OpenStax CNX". cnx.org. Archived from the original on May 5, 2015. Retrieved May 5, 2015.
- Larsen 2001, pp. 85–87.
- Purves 2012, pp. 481–484.
- Purves, Dale; Augustine, George J; Fitzpatrick, David; Katz, Lawrence C; LaMantia, Anthony-Samuel; McNamara, James O; Williams, S Mark, eds. (2001). "Rhombomeres". Neuroscience (2nd ed.). ISBN 978-0-87893-742-4.
- Chen, X. (2012). Mechanical Self-Assembly: Science and Applications. Springer Science & Business Media. pp. 188–189. ISBN 978-1-4614-4562-3.
- Ronan, L; Voets, N; Rua, C; Alexander-Bloch, A; Hough, M; Mackay, C; Crow, TJ; James, A; Giedd, JN; Fletcher, PC (August 2014). "Differential tangential expansion as a mechanism for cortical gyrification". Cerebral Cortex. 24 (8): 2219–28. doi:10.1093/cercor/bht082. PMC 4089386. PMID 23542881.
- Van Essen, DC (January 23, 1997). "A tension-based theory of morphogenesis and compact wiring in the central nervous system". Nature. 385 (6614): 313–8. Bibcode:1997Natur.385..313E. doi:10.1038/385313a0. PMID 9002514. S2CID 4355025.
- Borrell, V (January 24, 2018). "How Cells Fold the Cerebral Cortex". The Journal of Neuroscience. 38 (4): 776–783. doi:10.1523/JNEUROSCI.1106-17.2017. PMC 6596235. PMID 29367288.
- Florio, M.; et al. (March 27, 2015). "Human-specific gene ARHGAP11B promotes basal progenitor amplification and neocortex expansion". Science. 347 (6229): 1465–70. Bibcode:2015Sci...347.1465F. doi:10.1126/science.aaa1975. PMID 25721503. S2CID 34506325.
- "Parts of the Brain | Introduction to Psychology". courses.lumenlearning.com. Retrieved September 20, 2019.
- Guyton & Hall 2011, p. 685.
- Guyton & Hall 2011, p. 687.
- Guyton & Hall 2011, p. 686.
- Guyton & Hall 2011, pp. 698, 708.
- Davidson's 2010, p. 1139.
- Hellier, J. (2014). The Brain, the Nervous System, and Their Diseases [3 volumes]. ABC-CLIO. pp. 300–303. ISBN 978-1-61069-338-7.
- Guyton & Hall 2011, pp. 571–576.
- Guyton & Hall 2011, pp. 573–574.
- Guyton & Hall 2011, pp. 623–631.
- Guyton & Hall 2011, pp. 739–740.
- Pocock 2006, pp. 138–139.
- Squire 2013, pp. 525–526.
- Guyton & Hall 2011, pp. 647–648.
- Guyton & Hall 2011, pp. 202–203.
- Guyton & Hall 2011, pp. 205–208.
- Guyton & Hall 2011, pp. 505–509.
- "Brain Basics: Understanding Sleep | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Archived from the original on December 22, 2017.
- Guyton & Hall 2011, p. 723.
- Davis, J.F.; Choi, D.L.; Benoit, S.C. (2011). "24. Orexigenic Hypothalamic Peptides Behavior and Feeding – 24.5 Orexin". In Preedy, V.R.; Watson, R.R.; Martin, C.R. (eds.). Handbook of Behavior, Food and Nutrition. Springer. pp. 361–362. ISBN 978-0-387-92271-3.
- Squire 2013, p. 800.
- Squire 2013, p. 803.
- Squire 2013, p. 805.
- Guyton & Hall 2011, pp. 720–2.
- Poeppel, D.; Emmorey, K.; Hickok, G.; Pylkkänen, L. (October 10, 2012). "Towards a new neurobiology of language". The Journal of Neuroscience. 32 (41): 14125–14131. doi:10.1523/JNEUROSCI.3244-12.2012. PMC 3495005. PMID 23055482.
- Hickok, G (September 2009). "The functional neuroanatomy of language". Physics of Life Reviews. 6 (3): 121–143. Bibcode:2009PhLRv...6..121H. doi:10.1016/j.plrev.2009.06.001. PMC 2747108. PMID 20161054.
- Fedorenko, E.; Kanwisher, N. (2009). "Neuroimaging of language: why hasn't a clearer picture emerged?". Language and Linguistics Compass. 3 (4): 839–865. doi:10.1111/j.1749-818x.2009.00143.x. S2CID 2833893.
- Damasio, H. (2001). "Neural basis of language disorders". In Chapey, Roberta (ed.). Language intervention strategies in aphasia and related neurogenic communication disorders (4th ed.). Lippincott Williams & Wilkins. pp. 18–36. ISBN 978-0-7817-2133-2. OCLC 45952164.
- Berntson, G.; Cacioppo, J. (2009). Handbook of Neuroscience for the Behavioral Sciences, Volume 1. John Wiley & Sons. p. 145. ISBN 978-0-470-08355-0.
- Hellier, J. (2014). The Brain, the Nervous System, and Their Diseases [3 volumes]. ABC-CLIO. p. 1135. ISBN 978-1-61069-338-7.
- Kolb, B.; Whishaw, I.Q. (2013). Introduction to Brain and Behavior. Macmillan Higher Education. p. 296. ISBN 978-1-4641-3960-4.
- Sherwood, L. (2012). Human Physiology: From Cells to Systems. Cengage Learning. p. 181. ISBN 978-1-133-70853-7.
- Kalat, J (2015). Biological Psychology. Cengage Learning. p. 425. ISBN 978-1-305-46529-9.
- Cowin, S.C.; Doty, S.B. (2007). Tissue Mechanics. Springer Science & Business Media. p. 4. ISBN 978-0-387-49985-7.
- Morris, C.G.; Maisto, A.A. (2011). Understanding Psychology. Prentice Hall. p. 56. ISBN 978-0-205-76906-3.
- Kolb, B.; Whishaw, I.Q. (2013). Introduction to Brain and Behavior (Loose-Leaf). Macmillan Higher Education. pp. 524–549. ISBN 978-1-4641-3960-4.
- Schacter, D.L.; Gilbert, D.T.; Wegner, D.M. (2009). Introducing Psychology. Macmillan. p. 80. ISBN 978-1-4292-1821-4.
- Sander, David (2013). Armony, J.; Vuilleumier, Patrik (eds.). The Cambridge handbook of human affective neuroscience. Cambridge: Cambridge Univ. Press. p. 16. ISBN 978-0-521-17155-7.
- Lindquist, KA.; Wager, TD.; Kober, H; Bliss-Moreau, E; Barrett, LF (May 23, 2012). "The brain basis of emotion: A meta-analytic review". Behavioral and Brain Sciences. 35 (3): 121–143. doi:10.1017/S0140525X11000446. PMC 4329228. PMID 22617651.
- Phan, KL; Wager, Tor; Taylor, SF.; Liberzon, l (June 1, 2002). "Functional Neuroanatomy of Emotion: A Meta-Analysis of Emotion Activation Studies in PET and fMRI". NeuroImage. 16 (2): 331–348. doi:10.1006/nimg.2002.1087. PMID 12030820. S2CID 7150871.
- Malenka, RC; Nestler, EJ; Hyman, SE (2009). "Preface". In Sydor, A; Brown, RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. xiii. ISBN 978-0-07-148127-4.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 14: Higher Cognitive Function and Behavioral Control". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 6: Widely Projecting Systems: Monoamines, Acetylcholine, and Orexin". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
- Diamond, A (2013). "Executive functions". Annual Review of Psychology. 64: 135–168. doi:10.1146/annurev-psych-113011-143750. PMC 4084861. PMID 23020641.
Figure 4: Executive functions and related terms Archived May 9, 2018, at the Wayback Machine - Hyun, J.C.; Weyandt, L.L.; Swentosky, A. (2014). "Chapter 2: The Physiology of Executive Functioning". In Goldstein, S.; Naglieri, J. (eds.). Handbook of Executive Functioning. New York: Springer. pp. 13–23. ISBN 978-1-4614-8106-5.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 14: Higher Cognitive Function and Behavioral Control". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
In conditions in which prepotent responses tend to dominate behavior, such as in drug addiction, where drug cues can elicit drug seeking (Chapter 16), or in attention deficit hyperactivity disorder (ADHD; described below), significant negative consequences can result. ... ADHD can be conceptualized as a disorder of executive function; specifically, ADHD is characterized by reduced ability to exert and maintain cognitive control of behavior. Compared with healthy individuals, those with ADHD have diminished ability to suppress inappropriate prepotent responses to stimuli (impaired response inhibition) and diminished ability to inhibit responses to irrelevant stimuli (impaired interference suppression). ... Functional neuroimaging in humans demonstrates activation of the prefrontal cortex and caudate nucleus (part of the dorsal striatum) in tasks that demand inhibitory control of behavior. ... Early results with structural MRI show a thinner cerebral cortex, across much of the cerebrum, in ADHD subjects compared with age-matched controls, including areas of [the] prefrontal cortex involved in working memory and attention.
- Pocock 2006, p. 68.
- Clark, B.D.; Goldberg, E.M.; Rudy, B. (December 2009). "Electrogenic tuning of the axon initial segment". The Neuroscientist. 15 (6): 651–68. doi:10.1177/1073858409341973. PMC 2951114. PMID 20007821.
- Pocock 2006, pp. 70–74.
- "NIMH » Brain Basics". www.nimh.nih.gov. Archived from the original on March 26, 2017. Retrieved March 26, 2017.
- Purves, Dale (2011). Neuroscience (5. ed.). Sunderland, Mass.: Sinauer. p. 139. ISBN 978-0-87893-695-3.
- Swaminathan, N (April 29, 2008). "Why Does the Brain Need So Much Power?". Scientific American. Archived from the original on January 27, 2014. Retrieved November 19, 2010.
- Wasserman DH (January 2009). "Four grams of glucose". American Journal of Physiology. Endocrinology and Metabolism. 296 (1): E11–21. doi:10.1152/ajpendo.90563.2008. PMC 2636990. PMID 18840763.
Four grams of glucose circulates in the blood of a person weighing 70 kg. This glucose is critical for normal function in many cell types. In accordance with the importance of these 4 g of glucose, a sophisticated control system is in place to maintain blood glucose constant. Our focus has been on the mechanisms by which the flux of glucose from liver to blood and from blood to skeletal muscle is regulated. ... The brain consumes ∼60% of the blood glucose used in the sedentary, fasted person. ... The amount of glucose in the blood is preserved at the expense of glycogen reservoirs (Fig. 2). In postabsorptive humans, there are ∼100 g of glycogen in the liver and ∼400 g of glycogen in muscle. Carbohydrate oxidation by the working muscle can go up by ∼10-fold with exercise, and yet after 1 h, blood glucose is maintained at ∼4 g. ... It is now well established that both insulin and exercise cause translocation of GLUT4 to the plasma membrane. Except for the fundamental process of GLUT4 translocation, [muscle glucose uptake (MGU)] is controlled differently with exercise and insulin. Contraction-stimulated intracellular signaling (52, 80) and MGU (34, 75, 77, 88, 91, 98) are insulin independent. Moreover, the fate of glucose extracted from the blood is different in response to exercise and insulin (91, 105). For these reasons, barriers to glucose flux from blood to muscle must be defined independently for these two controllers of MGU.
- Quistorff, B; Secher, N; Van Lieshout, J (July 24, 2008). "Lactate fuels the human brain during exercise". The FASEB Journal. 22 (10): 3443–3449. doi:10.1096/fj.08-106104. PMID 18653766. S2CID 15394163.
- Obel, L.F.; Müller, M.S.; Walls, A.B.; Sickmann, H.M.; Bak, L.K.; Waagepetersen, H.S.; Schousboe, A. (2012). "Brain glycogen-new perspectives on its metabolic function and regulation at the subcellular level". Frontiers in Neuroenergetics. 4: 3. doi:10.3389/fnene.2012.00003. PMC 3291878. PMID 22403540.
- Marin-Valencia, I.; et al. (February 2013). "Heptanoate as a neural fuel: energetic and neurotransmitter precursors in normal and glucose transporter I-deficient (G1D) brain". Journal of Cerebral Blood Flow and Metabolism. 33 (2): 175–82. doi:10.1038/jcbfm.2012.151. PMC 3564188. PMID 23072752.
- Tsuji, A. (2005). "Small molecular drug transfer across the blood-brain barrier via carrier-mediated transport systems". NeuroRx. 2 (1): 54–62. doi:10.1602/neurorx.2.1.54. PMC 539320. PMID 15717057.
Uptake of valproic acid was reduced in the presence of medium-chain fatty acids such as hexanoate, octanoate, and decanoate, but not propionate or butyrate, indicating that valproic acid is taken up into the brain via a transport system for medium-chain fatty acids, not short-chain fatty acids. ... Based on these reports, valproic acid is thought to be transported bidirectionally between blood and brain across the BBB via two distinct mechanisms, monocarboxylic acid-sensitive and medium-chain fatty acid-sensitive transporters, for efflux and uptake, respectively.
- Vijay, N.; Morris, M.E. (2014). "Role of monocarboxylate transporters in drug delivery to the brain". Curr. Pharm. Des. 20 (10): 1487–98. doi:10.2174/13816128113199990462. PMC 4084603. PMID 23789956.
Monocarboxylate transporters (MCTs) are known to mediate the transport of short chain monocarboxylates such as lactate, pyruvate and butyrate. ... MCT1 and MCT4 have also been associated with the transport of short chain fatty acids such as acetate and formate which are then metabolized in the astrocytes [78].
- Clark, D.D.; Sokoloff. L. (1999). Siegel, G.J.; Agranoff, B.W.; Albers, R.W.; Fisher, S.K.; Uhler, M.D. (eds.). Basic Neurochemistry: Molecular, Cellular and Medical Aspects. Philadelphia: Lippincott. pp. 637–670. ISBN 978-0-397-51820-3.
- Mrsulja, B.B. (2012). Pathophysiology of Cerebral Energy Metabolism. Springer Science & Business Media. pp. 2–3. ISBN 978-1-4684-3348-7.
- Raichle, M.; Gusnard, DA (2002). "Appraising the brain's energy budget". Proc. Natl. Acad. Sci. U.S.A. 99 (16): 10237–10239. Bibcode:2002PNAS...9910237R. doi:10.1073/pnas.172399499. PMC 124895. PMID 12149485.
- Gianaros, Peter J.; Gray, Marcus A.; Onyewuenyi, Ikechukwu; Critchley, Hugo D. (2010). "Chapter 50. Neuroimaging methods in behavioral medicine". In Steptoe, A. (ed.). Handbook of Behavioral Medicine: Methods and Applications. Springer Science & Business Media. p. 770. doi:10.1007/978-0-387-09488-5_50. ISBN 978-0-387-09488-5.
- Kuzawa, C. W.; Chugani, H. T.; Grossman, L. I.; Lipovich, L.; Muzik, O.; Hof, P. R.; Wildman, D. E.; Sherwood, C. C.; Leonard, W. R.; Lange, N. (September 9, 2014). "Metabolic costs and evolutionary implications of human brain development". Proceedings of the National Academy of Sciences. 111 (36): 13010–13015. Bibcode:2014PNAS..11113010K. doi:10.1073/pnas.1323099111. ISSN 0027-8424. PMC 4246958. PMID 25157149.
- "Brain may flush out toxins during sleep". National Institutes of Health. Archived from the original on October 20, 2013. Retrieved October 25, 2013.
- Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O'Donnell J, Christensen DJ, Nicholson C, Iliff JJ, Takano T, Deane R, Nedergaard M (October 2013). "Sleep drives metabolite clearance from the adult brain". Science. 342 (6156): 373–377. Bibcode:2013Sci...342..373X. doi:10.1126/science.1241224. PMC 3880190. PMID 24136970.
Thus, the restorative function of sleep may be a consequence of the enhanced removal of potentially neurotoxic waste products that accumulate in the awake central nervous system.
- Tononi, Guilio; Cirelli, Chiara (August 2013). "Perchance to Prune" (PDF). Scientific American. 309 (2): 34–39. Bibcode:2013SciAm.309b..34T. doi:10.1038/scientificamerican0813-34. PMID 23923204. S2CID 54052089. Archived from the original (PDF) on December 26, 2018.
- Van Essen, D.C.; et al. (October 2012). "The Human Connectome Project: A data acquisition perspective". NeuroImage. 62 (4): 2222–2231. doi:10.1016/j.neuroimage.2012.02.018. PMC 3606888. PMID 22366334.
- Jones, E.G.; Mendell, L.M. (April 30, 1999). "Assessing the Decade of the Brain". Science. 284 (5415): 739. Bibcode:1999Sci...284..739J. doi:10.1126/science.284.5415.739. PMID 10336393. S2CID 13261978.
- "A $4.5 Billion Price Tag for the BRAIN Initiative?". Science | AAAS. June 5, 2014. Archived from the original on June 18, 2017.
- Towle, V.L.; et al. (January 1993). "The spatial location of EEG electrodes: locating the best-fitting sphere relative to cortical anatomy". Electroencephalography and Clinical Neurophysiology. 86 (1): 1–6. doi:10.1016/0013-4694(93)90061-y. PMID 7678386.
- Purves 2012, pp. 632–633.
- Silverstein, J. (2012). "Mapping the Motor and Sensory Cortices: A Historical Look and a Current Case Study in Sensorimotor Localization and Direct Cortical Motor Stimulation". The Neurodiagnostic Journal. 52 (1): 54–68. PMID 22558647. Archived from the original on November 17, 2012.
- Boraud, T.; Bezard, E.; et al. (2002). "From single extracellular unit recording in experimental and human Parkinsonism to the development of a functional concept of the role played by the basal ganglia in motor control". Progress in Neurobiology. 66 (4): 265–283. doi:10.1016/s0301-0082(01)00033-8. PMID 11960681. S2CID 23389986.
- Lancaster, MA; Renner, M; Martin, CA; Wenzel, D; Bicknell, LS; Hurles, ME; Homfray, T; Penninger, JM; Jackson, AP; Knoblich, JA (September 19, 2013). "Cerebral organoids model human brain development and microcephaly". Nature. 501 (7467): 373–9. Bibcode:2013Natur.501..373L. doi:10.1038/nature12517. PMC 3817409. PMID 23995685.
- Lee, CT; Bendriem, RM; Wu, WW; Shen, RF (August 20, 2017). "3D brain Organoids derived from pluripotent stem cells: promising experimental models for brain development and neurodegenerative disorders". Journal of Biomedical Science. 24 (1): 59. doi:10.1186/s12929-017-0362-8. PMC 5563385. PMID 28822354.
- "Magnetic Resonance, a critical peer-reviewed introduction; functional MRI". European Magnetic Resonance Forum. Archived from the original on June 2, 2017. Retrieved June 30, 2017.
- Buxton, R.; Uludag, K.; Liu, T. (2004). "Modeling the haemodynamic response to brain activation". NeuroImage. 23: S220–S233. CiteSeerX 10.1.1.329.29. doi:10.1016/j.neuroimage.2004.07.013. PMID 15501093. S2CID 8736954.
- Biswal, B.B. (August 15, 2012). "Resting state fMRI: a personal history". NeuroImage. 62 (2): 938–44. doi:10.1016/j.neuroimage.2012.01.090. PMID 22326802. S2CID 93823.
- Purves 2012, p. 20.
- Kane, R.L.; Parsons, T.D. (2017). The Role of Technology in Clinical Neuropsychology. Oxford University Press. p. 399. ISBN 978-0-19-023473-7.
Irimia, Chambers, Torgerson, and Van Horn (2012) provide a first-step graphic on how best to display connectivity findings, as is presented in Figure 13.15. This is referred to as a connectogram.
- Andrews, D.G. (2001). Neuropsychology. Psychology Press. ISBN 978-1-84169-103-9.
- Lepage, M. (2010). "Research at the Brain Imaging Centre". Douglas Mental Health University Institute. Archived from the original on March 5, 2012.
- Steward, C.A.; et al. (2017). "Genome annotation for clinical genomic diagnostics: strengths and weaknesses". Genome Med. 9 (1): 49. doi:10.1186/s13073-017-0441-1. PMC 5448149. PMID 28558813.
- Harrow, J.; et al. (September 2012). "GENCODE: the reference human genome annotation for The ENCODE Project". Genome Res. 22 (9): 1760–74. doi:10.1101/gr.135350.111. PMC 3431492. PMID 22955987.
- Gibson G, Muse SV (April 20, 2009). A primer of genome science (3rd ed.). Sunderland, MA: Sinauer Associates. ISBN 9780878932368.
- "The human proteome in brain – The Human Protein Atlas". www.proteinatlas.org. Archived from the original on September 29, 2017. Retrieved September 29, 2017.
- Uhlén, Mathias; Fagerberg, Linn; Hallström, Björn M.; Lindskog, Cecilia; Oksvold, Per; Mardinoglu, Adil; Sivertsson, Åsa; Kampf, Caroline; Sjöstedt, Evelina (January 23, 2015). "Tissue-based map of the human proteome". Science. 347 (6220): 1260419. doi:10.1126/science.1260419. ISSN 0036-8075. PMID 25613900. S2CID 802377.
- Warden, A (2017). "Gene expression profiling in the human alcoholic brain". Neuropharmacology. 122: 161–174. doi:10.1016/j.neuropharm.2017.02.017. PMC 5479716. PMID 28254370.
- Farris, S.P.; et al. (2015). "Applying the new genomics to alcohol dependence". Alcohol. 49 (8): 825–36. doi:10.1016/j.alcohol.2015.03.001. PMC 4586299. PMID 25896098.
- Rozycka, A; Liguz-Lecznar, M (August 2017). "The space where aging acts: focus on the GABAergic synapse". Aging Cell. 16 (4): 634–643. doi:10.1111/acel.12605. PMC 5506442. PMID 28497576.
- Flores, CE; Méndez, P (2014). "Shaping inhibition: activity dependent structural plasticity of GABAergic synapses". Frontiers in Cellular Neuroscience. 8: 327. doi:10.3389/fncel.2014.00327. PMC 4209871. PMID 25386117.
- "Brain Injury, Traumatic". Medcyclopaedia. GE. Archived from the original on May 26, 2011.
- Dawodu, S.T. (March 9, 2017). "Traumatic Brain Injury (TBI) – Definition and Pathophysiology: Overview, Epidemiology, Primary Injury". Medscape. Archived from the original on April 9, 2017.
- Davidson's 2010, pp. 1196–7.
- Davidson's 2010, pp. 1205–15.
- Davidson's 2010, pp. 1216–7.
- Volkow, N.D.; Koob, G.F.; McLellan, A.T. (January 2016). "Neurobiologic advances from the brain disease model of addiction". The New England Journal of Medicine. 374 (4): 363–371. doi:10.1056/NEJMra1511480. PMC 6135257. PMID 26816013.
- Simpson, J.M.; Moriarty, G.L. (2013). Multimodal Treatment of Acute Psychiatric Illness: A Guide for Hospital Diversion. Columbia University Press. pp. 22–24. ISBN 978-0-231-53609-7.
- Davidson's 2010, pp. 1172–9.
- "Status Epilepticus". Epilepsy Foundation.
- Moore, S.P. (2005). The Definitive Neurological Surgery Board Review. Lippincott Williams & Wilkins. p. 112. ISBN 978-1-4051-0459-3.
- Pennington, B.F. (2008). Diagnosing Learning Disorders, Second Edition: A Neuropsychological Framework. Guilford Press. pp. 3–10. ISBN 978-1-60623-786-1.
- Govaert, P.; de Vries, L.S. (2010). An Atlas of Neonatal Brain Sonography: (CDM 182–183). John Wiley & Sons. pp. 89–92. ISBN 978-1-898683-56-8.
- Perese, E.F. (2012). Psychiatric Advanced Practice Nursing: A Biopsychsocial Foundation for Practice. F.A. Davis. pp. 82–88. ISBN 978-0-8036-2999-8.
- Kearney, C.; Trull, T.J. (2016). Abnormal Psychology and Life: A Dimensional Approach. Cengage Learning. p. 395. ISBN 978-1-337-09810-6.
- Stevenson, D.K.; Sunshine, P.; Benitz, W.E. (2003). Fetal and Neonatal Brain Injury: Mechanisms, Management and the Risks of Practice. Cambridge University Press. p. 191. ISBN 978-0-521-80691-6.
- Dewhurst, John (2012). Dewhurst's Textbook of Obstetrics and Gynaecology. John Wiley & Sons. p. 43. ISBN 978-0-470-65457-6.
- Harbison, J.; Massey, A.; Barnett, L.; Hodge, D.; Ford, G.A. (June 1999). "Rapid ambulance protocol for acute stroke". Lancet. 353 (9168): 1935. doi:10.1016/S0140-6736(99)00966-6. PMID 10371574. S2CID 36692451.
- Davidson's 2010, p. 1183.
- Davidson's 2010, pp. 1180–1.
- Davidson's 2010, pp. 1181, 1183–1185.
- Davidson's 2010, pp. 1183–1185.
- Davidson's 2010, pp. 1185–1189.
- Goyal, M.; et al. (April 2016). "Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials". The Lancet. 387 (10029): 1723–1731. doi:10.1016/S0140-6736(16)00163-X. PMID 26898852. S2CID 34799180.
- Saver, J. L. (December 8, 2005). "Time is brain—quantified". Stroke. 37 (1): 263–266. doi:10.1161/01.STR.0000196957.55928.ab. PMID 16339467.
- Winstein, C.J.; et al. (June 2016). "Guidelines for adult stroke rehabilitation and recovery". Stroke. 47 (6): e98–e169. doi:10.1161/STR.0000000000000098. PMID 27145936. S2CID 4967333.
- Kuźma, Elżbieta; Lourida, Ilianna; Moore, Sarah F.; Levine, Deborah A.; Ukoumunne, Obioha C.; Llewellyn, David J. (November 2018). "Stroke and dementia risk: A systematic review and meta-analysis". Alzheimer's & Dementia. 14 (11): 1416–1426. doi:10.1016/j.jalz.2018.06.3061. ISSN 1552-5260. PMC 6231970. PMID 30177276.
- Goila, AK; Pawar, M (2009). "The diagnosis of brain death". Indian Journal of Critical Care Medicine. 13 (1): 7–11. doi:10.4103/0972-5229.53108. PMC 2772257. PMID 19881172.
- Wijdicks, EFM (January 8, 2002). "Brain death worldwide: accepted fact but no global consensus in diagnostic criteria". Neurology. 58 (1): 20–25. doi:10.1212/wnl.58.1.20. PMID 11781400. S2CID 219203458.
- Dhanwate, AD (September 2014). "Brainstem death: A comprehensive review in Indian perspective". Indian Journal of Critical Care Medicine. 18 (9): 596–605. doi:10.4103/0972-5229.140151. PMC 4166875. PMID 25249744.
- Davidson's 2010, p. 1158.
- Davidson's 2010, p. 200.
- Urden, L.D.; Stacy, K.M.; Lough, M.E. (2013). Priorities in Critical Care Nursing – E-Book. Elsevier Health Sciences. pp. 112–113. ISBN 978-0-323-29414-0.
- Domínguez, J.F.; Lewis, E.D.; Turner, R.; Egan, G.F. (2009). Chiao, J.Y. (ed.). The Brain in Culture and Culture in the Brain: A Review of Core Issues in Neuroanthropology. Progress in Brain Research. Special issue: Cultural Neuroscience: Cultural Influences on Brain Function. Vol. 178. pp. 43–6. doi:10.1016/S0079-6123(09)17804-4. ISBN 978-0-444-53361-6. PMID 19874961.
- "Cultural Environment Influences Brain Function | Psych Central News". Psych Central News. August 4, 2010. Archived from the original on January 17, 2017.
- Macmillan, Malcolm B. (2000). An Odd Kind of Fame: Stories of Phineas Gage. MIT Press. ISBN 978-0-262-13363-0.
- Rescher, N. (1992). G. W. Leibniz's Monadology. Psychology Press. p. 83. ISBN 978-0-415-07284-7.
- Hart, WD (1996). Guttenplan S (ed.). A Companion to the Philosophy of Mind. Blackwell. pp. 265–267.
- Churchland, P.S. (1989). "Ch. 8". Neurophilosophy. MIT Press. ISBN 978-0-262-53085-9.
- Selimbeyoglu, Aslihan; Parvizi, J (2010). "Electrical stimulation of the human brain: perceptual and behavioral phenomena reported in the old and new literature". Frontiers in Human Neuroscience. 4: 46. doi:10.3389/fnhum.2010.00046. PMC 2889679. PMID 20577584.
- Schwartz, J.H. Appendix D: Consciousness and the Neurobiology of the Twenty-First Century. In Kandel, E.R.; Schwartz, J.H.; Jessell, T.M. (2000). Principles of Neural Science, 4th Edition.
- Lilienfeld, S.O.; Lynn, S.J.; Ruscio, J.; Beyerstein, B.L. (2011). 50 Great Myths of Popular Psychology: Shattering Widespread Misconceptions about Human Behavior. John Wiley & Sons. p. 89. ISBN 978-1-4443-6074-5.
- McDaniel, M. (2005). "Big-brained people are smarter" (PDF). Intelligence. 33 (4): 337–346. doi:10.1016/j.intell.2004.11.005. Archived (PDF) from the original on September 6, 2014.
- Luders, E.; et al. (September 2008). "Mapping the relationship between cortical convolution and intelligence: effects of gender". Cerebral Cortex. 18 (9): 2019–26. doi:10.1093/cercor/bhm227. PMC 2517107. PMID 18089578.
- Hoppe, C; Stojanovic, J (2008). "High-Aptitude Minds". Scientific American Mind. 19 (4): 60–67. doi:10.1038/scientificamericanmind0808-60.
- "Tupaia belangeri". The Genome Institute, Washington University. Archived from the original on June 1, 2010. Retrieved January 22, 2016.
- Carrier, Martin; Mittelstrass, Jürgen (1991). Mind, Brain, Behavior: The Mind-body Problem and the Philosophy of Psychology [Geist, Gehirn, Verhalten]. Translated by Lindberg, Steven (revised and expanded English ed.). Berlin: Walter de Gruyter. p. 11. ISBN 9783110128765. Retrieved May 22, 2021.
[...] the Aristotelian view that the soul resides primarily in the heart [...].
- Cobb, Matthew (April 21, 2020). The Idea of the Brain: The Past and Future of Neuroscience. New York: Hachette UK (published 2020). ISBN 9781541646865. Retrieved May 22, 2021.
[...] the ways in which we think about [the brain] are much richer than in the past, not simply because of the amazing facts we have discovered, but above all because of how we interpret them.
- Jarrett, C. (November 17, 2014). Great Myths of the Brain. John Wiley & Sons. ISBN 978-1-118-31271-1.
- Phillips, Helen (July 11, 2002). "Video game "brain damage" claim criticised". New Scientist. Archived from the original on January 11, 2009. Retrieved February 6, 2008.
- Popova, Maria (August 18, 2011). "'Brain Culture': How Neuroscience Became a Pop Culture Fixation". The Atlantic. Archived from the original on July 28, 2017.
- Thornton, Davi Johnson (2011). Brain Culture. Neuroscience and Popular Media. Rutgers University Press. ISBN 978-0-8135-5013-8.
- Cyborgs and Space Archived October 6, 2011, at the Wayback Machine, in Astronautics (September 1960), by Manfred E. Clynes and Nathan S. Kline.
- Bergfelder, Tim (2005). International Adventures: German Popular Cinema and European Co-productions in the 1960s. Berghahn Books. p. 129. ISBN 978-1-57181-538-5.
- Kandel, ER; Schwartz JH; Jessell TM (2000). Principles of Neural Science (4th ed.). New York: McGraw-Hill. ISBN 978-0-8385-7701-1.
- Gross, Charles G. (1987). Adelman, George (ed.). Encyclopedia of neuroscience (PDF) (2. ed.). Boston: Birkhäeuser. pp. 843–847. ISBN 978-0-8176-3335-6. Archived (PDF) from the original on May 5, 2013.
- Bear, M.F.; B.W. Connors; M.A. Paradiso (2001). Neuroscience: Exploring the Brain. Baltimore: Lippincott. ISBN 978-0-7817-3944-3.
- von Staden, p.157
- Swanson, Larry W. (August 12, 2014). Neuroanatomical Terminology: A Lexicon of Classical Origins and Historical Foundations. Oxford University Press. ISBN 978-0-19-534062-4.
- Lokhorst, Gert-Jan (January 1, 2016). "Descartes and the Pineal Gland". The Stanford Encyclopedia of Philosophy. Metaphysics Research Lab, Stanford University. Retrieved March 11, 2017.
- Gross, Charles G. (1999). Brain, vision, memory : tales in the history of neuroscience (1st MIT Press pbk. ed.). Cambridge, Mass.: MIT. pp. 37–51. ISBN 978-0-262-57135-7.
- Marshall, Louise H.; Magoun, Horace W. (March 9, 2013). Discoveries in the Human Brain: Neuroscience Prehistory, Brain Structure, and Function. Springer Science & Business Media. p. 44. ISBN 978-1-475-74997-7.
- Holtz, Anders; Levi, Richard (July 20, 2010). Spinal Cord Injury. Oxford University Press. ISBN 978-0-19-970681-5.
- Tessman, Patrick A.; Suarez, Jose I. (2002). "Influence of early printmaking on the development of neuroanatomy and neurology". Archives of Neurology. 59 (12): 1964–1969. doi:10.1001/archneur.59.12.1964. PMID 12470188.
- O'Connor, James (2003). "Thomas Willis and the background to Cerebri Anatome". Journal of the Royal Society of Medicine. 96 (3): 139–143. doi:10.1177/014107680309600311. PMC 539424. PMID 12612118.
- EMERY, ALAN (October 2000). "A Short History of Neurology: The British Contribution 1660–1910. Edited by F. CLIFFORD ROSE. (Pp. 282; illustrated; £25 Paperback; ISBN 07506 4165 7.) Oxford: Butterworth-Heinemann". Journal of Anatomy. 197 (3): 513–518. doi:10.1046/j.1469-7580.2000.197305131.x. PMC 1468164.
- Olesko, Kathryn M.; Holmes, Frederic L. (1994). Cahan, David (ed.). "Experiment, Quantification, and Discovery: Helmholtz's Early Physiological Researches, 1843-50". Hermann von Helmholtz and the Foundations of Nineteenth Century Science. Berkeley; Los Angeles; London: University of California Press: 50–108.
- Sabbatini, Renato M.E. "Sabbatini, R.M.E.: The Discovery of Bioelectricity. Nerve Conduction". www.cerebromente.org.br. Archived from the original on June 26, 2017. Retrieved June 10, 2017.
- Finkelstein, Gabriel Ward (2013). Emil du Bois-Reymond : neuroscience, self, and society in nineteenth-century Germany. Cambridge, Massachusetts. ISBN 978-1-4619-5032-5. OCLC 864592470.
- Karbowski, Kazimierz (February 14, 2008). "Sixty Years of Clinical Electroencephalography". European Neurology. 30 (3): 170–175. doi:10.1159/000117338. PMID 2192889.
- Pearce, J.M.S. (March 17, 2009). "Marie-Jean-Pierre Flourens (1794–1867) and Cortical Localization". European Neurology. 61 (5): 311–314. doi:10.1159/000206858. PMID 19295220.
- De Carlos, Juan A.; Borrell, José (August 2007). "A historical reflection of the contributions of Cajal and Golgi to the foundations of neuroscience". Brain Research Reviews. 55 (1): 8–16. doi:10.1016/j.brainresrev.2007.03.010. hdl:10261/62299. PMID 17490748. S2CID 7266966.
- Burke, R.E. (April 2007). "Sir Charles Sherrington's The integrative action of the nervous system: a centenary appreciation". Brain. 130 (Pt 4): 887–894. doi:10.1093/brain/awm022. PMID 17438014.
- Squire, Larry R., ed. (1996). The history of neuroscience in autobiography. Washington DC: Society for Neuroscience. pp. 475–97. ISBN 978-0-12-660305-7.
- Cowan, W.M.; Harter, D.H.; Kandel, E.R. (2000). "The emergence of modern neuroscience: Some implications for neurology and psychiatry". Annual Review of Neuroscience. 23: 345–346. doi:10.1146/annurev.neuro.23.1.343. PMID 10845068.
- Brady, Joseph V.; Nauta, Walle J. H. (October 22, 2013). Principles, Practices, and Positions in Neuropsychiatric Research: Proceedings of a Conference Held in June 1970 at the Walter Reed Army Institute of Research, Washington, D.C., in Tribute to Dr. David Mckenzie Rioch upon His Retirement as Director of the Neuropsychiatry Division of That Institute. Elsevier. p. vii. ISBN 978-1-4831-5453-4.
- Adelman, George (January 15, 2010). "The Neurosciences Research Program at MIT and the Beginning of the Modern Field of Neuroscience". Journal of the History of the Neurosciences. 19 (1): 15–23. doi:10.1080/09647040902720651. PMID 20391098. S2CID 21513317.
- Principles of Neural Science, 4th ed. Eric R. Kandel, James H. Schwartz, Thomas M. Jessel, eds. McGraw-Hill:New York, NY. 2000.
- Papez, J.W. (February 1995). "A proposed mechanism of emotion. 1937". The Journal of Neuropsychiatry and Clinical Neurosciences. 7 (1): 103–12. doi:10.1176/jnp.7.1.103. PMID 7711480.
- Lambert, Kelly G. (August 2003). "The life and career of Paul MacLean". Physiology & Behavior. 79 (3): 343–349. doi:10.1016/S0031-9384(03)00147-1. PMID 12954429. S2CID 18596574.
- Chatterjee, Anjan; Coslett, H. Branch (December 2013). The Roots of Cognitive Neuroscience: Behavioral Neurology and Neuropsychology. OUP USA. pp. 337–8. ISBN 978-0-19-539554-9.
- Bliss, Michael (October 1, 2005). Harvey Cushing : A Life in Surgery: A Life in Surgery. USA: Oxford University Press. pp. ix–x. ISBN 978-0-19-534695-4.
- Kretzer, RM; Coon, AL; Tamargo, RJ (June 2010). "Walter E. Dandy's contributions to vascular neurosurgery". Journal of Neurosurgery. 112 (6): 1182–91. doi:10.3171/2009.7.JNS09737. PMID 20515365.
- Glees, Paul (2005). The Human Brain. Cambridge University Press. p. 1. ISBN 978-0-521-01781-7.
- Simpkins, C. Alexander; Simpkins, Annellen M. (2012). Neuroscience for Clinicians: Evidence, Models, and Practice. Springer Science & Business Media. p. 143. ISBN 978-1-4614-4842-6.
- Bornstein, Marc H.; Lamb, Michael E. (2015). Developmental Science: An Advanced Textbook. Psychology Press. p. 220. ISBN 978-1-136-28220-1.
- Bernstein, Douglas (2010). Essentials of Psychology. Cengage Learning. p. 64. ISBN 978-0-495-90693-3.
- Hofman, Michel A. (March 27, 2014). "Evolution of the human brain: when bigger is better". Frontiers in Neuroanatomy. 8: 15. doi:10.3389/fnana.2014.00015. PMC 3973910. PMID 24723857.
- Gray, Peter (2002). Psychology (4th ed.). Worth Publishers. ISBN 978-0-7167-5162-5. OCLC 46640860.
- Lu, Zhong-Lin; Dosher, Barbara (2013). Visual Psychophysics: From Laboratory to Theory. MIT Press. p. 3. ISBN 978-0-262-01945-3.
- Sharwood Smith, Mike (2017). Introducing Language and Cognition. Cambridge University Press. p. 206. ISBN 978-1-107-15289-2.
- Kolb, Bryan; Whishaw, Ian Q. (2013). Introduction to Brain and Behavior. Macmillan Higher Education. p. 21. ISBN 978-1-4641-3960-4.
- Nieuwenhuys, Rudolf; ten Donkelaar, Hans J.; Nicholson, Charles (2014). The Central Nervous System of Vertebrates. Springer. p. 2127. ISBN 978-3-642-18262-4.
- Lerner, Lee; Lerner, Brenda Wilmoth (2004). The Gale Encyclopedia of Science: Pheasants-Star. Gale. p. 3759. ISBN 978-0-7876-7559-2.
As human's position changed and the manner in which the skull balanced on the spinal column pivoted, the brain expanded, altering the shape of the cranium.
- Begun, David R. (2012). A Companion to Paleoanthropology. John Wiley & Sons. p. 388. ISBN 978-1-118-33237-5.
- Jones, R. (2012). "Neurogenetics: What makes a human brain?". Nature Reviews Neuroscience. 13 (10): 655. doi:10.1038/nrn3355. PMID 22992645. S2CID 44421363.
- "Encephalo- Etymology". Online Etymology Dictionary. Archived from the original on October 2, 2017. Retrieved October 24, 2015.
- Fan, Xue; Markram, Henry (May 7, 2019). "A Brief History of Simulation Neuroscience". Frontiers in Neuroinformatics. 13: 32. doi:10.3389/fninf.2019.00032. ISSN 1662-5196. PMC 6513977. PMID 31133838.
- Parent, A.; Carpenter, M.B. (1995). "Ch. 1". Carpenter's Human Neuroanatomy. Williams & Wilkins. ISBN 978-0-683-06752-1.
- Bigos, K.L.; Hariri, A.; Weinberger, D. (2015). Neuroimaging Genetics: Principles and Practices. Oxford University Press. p. 157. ISBN 978-0-19-992022-8.
- Cosgrove, K.P.; Mazure, C.M.; Staley, J.K. (2007). "Evolving knowledge of sex differences in brain structure, function, and chemistry". Biol Psychiatry. 62 (8): 847–855. doi:10.1016/j.biopsych.2007.03.001. PMC 2711771. PMID 17544382.
- Molina, D. Kimberley; DiMaio, Vincent J.M. (2012). "Normal Organ Weights in Men". The American Journal of Forensic Medicine and Pathology. 33 (4): 368–372. doi:10.1097/PAF.0b013e31823d29ad. ISSN 0195-7910. PMID 22182984. S2CID 32174574.
- Molina, D. Kimberley; DiMaio, Vincent J. M. (2015). "Normal Organ Weights in Women". The American Journal of Forensic Medicine and Pathology. 36 (3): 182–187. doi:10.1097/PAF.0000000000000175. ISSN 0195-7910. PMID 26108038. S2CID 25319215.
- Gray's Anatomy 2008, pp. 227–9.
- Gray's Anatomy 2008, pp. 335–7.
- Ribas, G. C. (2010). "The cerebral sulci and gyri". Neurosurgical Focus. 28 (2): 7. doi:10.3171/2009.11.FOCUS09245. PMID 20121437.
- Frigeri, T.; Paglioli, E.; De Oliveira, E.; Rhoton Jr, A. L. (2015). "Microsurgical anatomy of the central lobe". Journal of Neurosurgery. 122 (3): 483–98. doi:10.3171/2014.11.JNS14315. PMID 25555079.
- Purves 2012, p. 724.
- Cipolla, M.J. (January 1, 2009). Anatomy and Ultrastructure. Morgan & Claypool Life Sciences. Archived from the original on October 1, 2017.
- "A Surgeon's-Eye View of the Brain". NPR.org. Archived from the original on November 7, 2017.
- Sampaio-Baptista, C; Johansen-Berg, H (December 20, 2017). "White Matter Plasticity in the Adult Brain". Neuron. 96 (6): 1239–1251. doi:10.1016/j.neuron.2017.11.026. PMC 5766826. PMID 29268094.
- Davey, G. (2011). Applied Psychology. John Wiley & Sons. p. 153. ISBN 978-1-4443-3121-9.
- Arsava, E. Y.; Arsava, E. M.; Oguz, K. K.; Topcuoglu, M. A. (2019). "Occipital petalia as a predictive imaging sign for transverse sinus dominance". Neurological Research. 41 (4): 306–311. doi:10.1080/01616412.2018.1560643. PMID 30601110. S2CID 58546404.
- Ackerman, S. (1992). Discovering the brain. Washington, D.C.: National Academy Press. pp. 22–25. ISBN 978-0-309-04529-2.
- Larsen 2001, pp. 455–456.
- Kandel, E.R.; Schwartz, J.H.; Jessel T.M. (2000). Principles of Neural Science. McGraw-Hill Professional. p. 324. ISBN 978-0-8385-7701-1.
- Guyton & Hall 2011, p. 574.
- Guyton & Hall 2011, p. 667.
- Principles of Anatomy and Physiology 12th Edition – Tortora, p. 519.
- Freberg, L. (2009). Discovering Biological Psychology. Cengage Learning. pp. 44–46. ISBN 978-0-547-17779-3.
- Kolb, B.; Whishaw, I. (2009). Fundamentals of Human Neuropsychology. Macmillan. pp. 73–75. ISBN 978-0-7167-9586-5.
- Pocock 2006, p. 64.
- Purves 2012, p. 399.
- Gray's Anatomy 2008, pp. 325–6.
- Goll, Y.; Atlan, G.; Citri, A. (August 2015). "Attention: the claustrum". Trends in Neurosciences. 38 (8): 486–95. doi:10.1016/j.tins.2015.05.006. PMID 26116988. S2CID 38353825.
- Goard, M.; Dan, Y. (October 4, 2009). "Basal forebrain activation enhances cortical coding of natural scenes". Nature Neuroscience. 12 (11): 1444–1449. doi:10.1038/nn.2402. PMC 3576925. PMID 19801988.
- Guyton & Hall 2011, p. 699.
- Gray's Anatomy 2008, p. 298.
- Netter, F. (2014). Atlas of Human Anatomy Including Student Consult Interactive Ancillaries and Guides (6th ed.). Philadelphia, Penn.: W B Saunders Co. p. 114. ISBN 978-1-4557-0418-7.
- Gray's Anatomy 2008, p. 297.
- Guyton & Hall 2011, pp. 698–9.
- Squire 2013, pp. 761–763.
- Gray's Anatomy 2008, p. 275.
- Guyton & Hall 2011, p. 691.
- Purves 2012, p. 377.
- Azevedo, F.; et al. (April 10, 2009). "Equal numbers of neuronal and nonneuronal cells make the human brain an isometrically scaled-up primate brain". The Journal of Comparative Neurology. 513 (5): 532–541. doi:10.1002/cne.21974. PMID 19226510. S2CID 5200449.
despite the widespread quotes that the human brain contains 100 billion neurons and ten times more glial cells, the absolute number of neurons and glial cells in the human brain remains unknown. Here we determine these numbers by using the isotropic fractionator and compare them with the expected values for a human-sized primate. We find that the adult male human brain contains on average 86.1 ± 8.1 billion NeuN-positive cells (“neurons”) and 84.6 ± 9.8 billion NeuN-negative (“nonneuronal”) cells.
- Pavel, Fiala; Jiří, Valenta (January 1, 2013). Central Nervous System. Karolinum Press. p. 79. ISBN 978-80-246-2067-1.
- Polyzoidis, S.; Koletsa, T.; Panagiotidou, S.; Ashkan, K.; Theoharides, T.C. (2015). "Mast cells in meningiomas and brain inflammation". Journal of Neuroinflammation. 12 (1): 170. doi:10.1186/s12974-015-0388-3. PMC 4573939. PMID 26377554.
- Guyton & Hall 2011, pp. 748–749.
- Budzyński, J; Kłopocka, M. (2014). "Brain-gut axis in the pathogenesis of Helicobacter pylori infection". World J. Gastroenterol. 20 (18): 5212–25. doi:10.3748/wjg.v20.i18.5212. PMC 4017036. PMID 24833851.
- Carabotti, M.; Scirocco, A.; Maselli, M.A.; Severi, C. (2015). "The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems". Ann Gastroenterol. 28 (2): 203–209. PMC 4367209. PMID 25830558.
- Sjöstedt, Evelina; Fagerberg, Linn; Hallström, Björn M.; Häggmark, Anna; Mitsios, Nicholas; Nilsson, Peter; Pontén, Fredrik; Hökfelt, Tomas; Uhlén, Mathias (June 15, 2015). "Defining the human brain proteome using transcriptomics and antibody-based profiling with a focus on the cerebral cortex". PLOS ONE. 10 (6): e0130028. Bibcode:2015PLoSO..1030028S. doi:10.1371/journal.pone.0130028. ISSN 1932-6203. PMC 4468152. PMID 26076492.
- Gray's Anatomy 2008, pp. 242–244.
- Purves 2012, p. 742.
- Gray's Anatomy 2008, p. 243.
- Iliff, JJ; Nedergaard, M (June 2013). "Is there a cerebral lymphatic system?". Stroke. 44 (6 Suppl 1): S93-5. doi:10.1161/STROKEAHA.112.678698. PMC 3699410. PMID 23709744.
- Gaillard, F. "Glymphatic pathway". radiopaedia.org. Archived from the original on October 30, 2017.
- Bacyinski A, Xu M, Wang W, Hu J (November 2017). "The Paravascular Pathway for Brain Waste Clearance: Current Understanding, Significance and Controversy". Frontiers in Neuroanatomy. 11: 101. doi:10.3389/fnana.2017.00101. PMC 5681909. PMID 29163074.
The paravascular pathway, also known as the “glymphatic” pathway, is a recently described system for waste clearance in the brain. According to this model, cerebrospinal fluid (CSF) enters the paravascular spaces surrounding penetrating arteries of the brain, mixes with interstitial fluid (ISF) and solutes in the parenchyma, and exits along paravascular spaces of draining veins. ... In addition to Aβ clearance, the glymphatic system may be involved in the removal of other interstitial solutes and metabolites. By measuring the lactate concentration in the brains and cervical lymph nodes of awake and sleeping mice, Lundgaard et al. (2017) demonstrated that lactate can exit the CNS via the paravascular pathway. Their analysis took advantage of the substantiated hypothesis that glymphatic function is promoted during sleep (Xie et al., 2013; Lee et al., 2015; Liu et al., 2017).
- Dissing-Olesen, L.; Hong, S.; Stevens, B. (August 2015). "New brain lymphatic vessels drain old concepts". EBioMedicine. 2 (8): 776–7. doi:10.1016/j.ebiom.2015.08.019. PMC 4563157. PMID 26425672.
- Sun, BL; Wang, LH; Yang, T; Sun, JY; Mao, LL; Yang, MF; Yuan, H; Colvin, RA; Yang, XY (April 2018). "Lymphatic drainage system of the brain: A novel target for intervention of neurological diseases". Progress in Neurobiology. 163–164: 118–143. doi:10.1016/j.pneurobio.2017.08.007. PMID 28903061. S2CID 6290040.
- Gray's Anatomy 2008, p. 247.
- Gray's Anatomy 2008, pp. 251–2.
- Gray's Anatomy 2008, p. 250.
- Gray's Anatomy 2008, p. 248.
- Gray's Anatomy 2008, p. 251.
- Gray's Anatomy 2008, pp. 254–6.
- Elsevier's 2007, pp. 311–4.
- Daneman, R.; Zhou, L.; Kebede, A.A.; Barres, B.A. (November 25, 2010). "Pericytes are required for blood-brain barrier integrity during embryogenesis". Nature. 468 (7323): 562–6. Bibcode:2010Natur.468..562D. doi:10.1038/nature09513. PMC 3241506. PMID 20944625.
- Laterra, J.; Keep, R.; Betz, L.A.; et al. (1999). "Blood–cerebrospinal fluid barrier". Basic neurochemistry: molecular, cellular and medical aspects (6th ed.). Philadelphia: Lippincott-Raven.
- Sadler, T. (2010). Langman's medical embryology (11th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 293. ISBN 978-0-7817-9069-7.
- Larsen 2001, p. 419.
- Larsen 2001, pp. 85–88.
- Purves 2012, pp. 480–482.
- Larsen 2001, pp. 445–446.
- "OpenStax CNX". cnx.org. Archived from the original on May 5, 2015. Retrieved May 5, 2015.
- Larsen 2001, pp. 85–87.
- Purves 2012, pp. 481–484.
- Purves, Dale; Augustine, George J; Fitzpatrick, David; Katz, Lawrence C; LaMantia, Anthony-Samuel; McNamara, James O; Williams, S Mark, eds. (2001). "Rhombomeres". Neuroscience (2nd ed.). ISBN 978-0-87893-742-4.
- Chen, X. (2012). Mechanical Self-Assembly: Science and Applications. Springer Science & Business Media. pp. 188–189. ISBN 978-1-4614-4562-3.
- Ronan, L; Voets, N; Rua, C; Alexander-Bloch, A; Hough, M; Mackay, C; Crow, TJ; James, A; Giedd, JN; Fletcher, PC (August 2014). "Differential tangential expansion as a mechanism for cortical gyrification". Cerebral Cortex. 24 (8): 2219–28. doi:10.1093/cercor/bht082. PMC 4089386. PMID 23542881.
- Van Essen, DC (January 23, 1997). "A tension-based theory of morphogenesis and compact wiring in the central nervous system". Nature. 385 (6614): 313–8. Bibcode:1997Natur.385..313E. doi:10.1038/385313a0. PMID 9002514. S2CID 4355025.
- Borrell, V (January 24, 2018). "How Cells Fold the Cerebral Cortex". The Journal of Neuroscience. 38 (4): 776–783. doi:10.1523/JNEUROSCI.1106-17.2017. PMC 6596235. PMID 29367288.
- Florio, M.; et al. (March 27, 2015). "Human-specific gene ARHGAP11B promotes basal progenitor amplification and neocortex expansion". Science. 347 (6229): 1465–70. Bibcode:2015Sci...347.1465F. doi:10.1126/science.aaa1975. PMID 25721503. S2CID 34506325.
- "Parts of the Brain | Introduction to Psychology". courses.lumenlearning.com. Retrieved September 20, 2019.
- Guyton & Hall 2011, p. 685.
- Guyton & Hall 2011, p. 687.
- Guyton & Hall 2011, p. 686.
- Guyton & Hall 2011, pp. 698, 708.
- Davidson's 2010, p. 1139.
- Hellier, J. (2014). The Brain, the Nervous System, and Their Diseases [3 volumes]. ABC-CLIO. pp. 300–303. ISBN 978-1-61069-338-7.
- Guyton & Hall 2011, pp. 571–576.
- Guyton & Hall 2011, pp. 573–574.
- Guyton & Hall 2011, pp. 623–631.
- Guyton & Hall 2011, pp. 739–740.
- Pocock 2006, pp. 138–139.
- Squire 2013, pp. 525–526.
- Guyton & Hall 2011, pp. 647–648.
- Guyton & Hall 2011, pp. 202–203.
- Guyton & Hall 2011, pp. 205–208.
- Guyton & Hall 2011, pp. 505–509.
- "Brain Basics: Understanding Sleep | National Institute of Neurological Disorders and Stroke". www.ninds.nih.gov. Archived from the original on December 22, 2017.
- Guyton & Hall 2011, p. 723.
- Davis, J.F.; Choi, D.L.; Benoit, S.C. (2011). "24. Orexigenic Hypothalamic Peptides Behavior and Feeding – 24.5 Orexin". In Preedy, V.R.; Watson, R.R.; Martin, C.R. (eds.). Handbook of Behavior, Food and Nutrition. Springer. pp. 361–362. ISBN 978-0-387-92271-3.
- Squire 2013, p. 800.
- Squire 2013, p. 803.
- Squire 2013, p. 805.
- Guyton & Hall 2011, pp. 720–2.
- Poeppel, D.; Emmorey, K.; Hickok, G.; Pylkkänen, L. (October 10, 2012). "Towards a new neurobiology of language". The Journal of Neuroscience. 32 (41): 14125–14131. doi:10.1523/JNEUROSCI.3244-12.2012. PMC 3495005. PMID 23055482.
- Hickok, G (September 2009). "The functional neuroanatomy of language". Physics of Life Reviews. 6 (3): 121–143. Bibcode:2009PhLRv...6..121H. doi:10.1016/j.plrev.2009.06.001. PMC 2747108. PMID 20161054.
- Fedorenko, E.; Kanwisher, N. (2009). "Neuroimaging of language: why hasn't a clearer picture emerged?". Language and Linguistics Compass. 3 (4): 839–865. doi:10.1111/j.1749-818x.2009.00143.x. S2CID 2833893.
- Damasio, H. (2001). "Neural basis of language disorders". In Chapey, Roberta (ed.). Language intervention strategies in aphasia and related neurogenic communication disorders (4th ed.). Lippincott Williams & Wilkins. pp. 18–36. ISBN 978-0-7817-2133-2. OCLC 45952164.
- Berntson, G.; Cacioppo, J. (2009). Handbook of Neuroscience for the Behavioral Sciences, Volume 1. John Wiley & Sons. p. 145. ISBN 978-0-470-08355-0.
- Hellier, J. (2014). The Brain, the Nervous System, and Their Diseases [3 volumes]. ABC-CLIO. p. 1135. ISBN 978-1-61069-338-7.
- Kolb, B.; Whishaw, I.Q. (2013). Introduction to Brain and Behavior. Macmillan Higher Education. p. 296. ISBN 978-1-4641-3960-4.
- Sherwood, L. (2012). Human Physiology: From Cells to Systems. Cengage Learning. p. 181. ISBN 978-1-133-70853-7.
- Kalat, J (2015). Biological Psychology. Cengage Learning. p. 425. ISBN 978-1-305-46529-9.
- Cowin, S.C.; Doty, S.B. (2007). Tissue Mechanics. Springer Science & Business Media. p. 4. ISBN 978-0-387-49985-7.
- Morris, C.G.; Maisto, A.A. (2011). Understanding Psychology. Prentice Hall. p. 56. ISBN 978-0-205-76906-3.
- Kolb, B.; Whishaw, I.Q. (2013). Introduction to Brain and Behavior (Loose-Leaf). Macmillan Higher Education. pp. 524–549. ISBN 978-1-4641-3960-4.
- Schacter, D.L.; Gilbert, D.T.; Wegner, D.M. (2009). Introducing Psychology. Macmillan. p. 80. ISBN 978-1-4292-1821-4.
- Sander, David (2013). Armony, J.; Vuilleumier, Patrik (eds.). The Cambridge handbook of human affective neuroscience. Cambridge: Cambridge Univ. Press. p. 16. ISBN 978-0-521-17155-7.
- Lindquist, KA.; Wager, TD.; Kober, H; Bliss-Moreau, E; Barrett, LF (May 23, 2012). "The brain basis of emotion: A meta-analytic review". Behavioral and Brain Sciences. 35 (3): 121–143. doi:10.1017/S0140525X11000446. PMC 4329228. PMID 22617651.
- Phan, KL; Wager, Tor; Taylor, SF.; Liberzon, l (June 1, 2002). "Functional Neuroanatomy of Emotion: A Meta-Analysis of Emotion Activation Studies in PET and fMRI". NeuroImage. 16 (2): 331–348. doi:10.1006/nimg.2002.1087. PMID 12030820. S2CID 7150871.
- Malenka, RC; Nestler, EJ; Hyman, SE (2009). "Preface". In Sydor, A; Brown, RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. xiii. ISBN 978-0-07-148127-4.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 14: Higher Cognitive Function and Behavioral Control". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 6: Widely Projecting Systems: Monoamines, Acetylcholine, and Orexin". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
- Diamond, A (2013). "Executive functions". Annual Review of Psychology. 64: 135–168. doi:10.1146/annurev-psych-113011-143750. PMC 4084861. PMID 23020641.
Figure 4: Executive functions and related terms Archived May 9, 2018, at the Wayback Machine - Hyun, J.C.; Weyandt, L.L.; Swentosky, A. (2014). "Chapter 2: The Physiology of Executive Functioning". In Goldstein, S.; Naglieri, J. (eds.). Handbook of Executive Functioning. New York: Springer. pp. 13–23. ISBN 978-1-4614-8106-5.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 14: Higher Cognitive Function and Behavioral Control". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
In conditions in which prepotent responses tend to dominate behavior, such as in drug addiction, where drug cues can elicit drug seeking (Chapter 16), or in attention deficit hyperactivity disorder (ADHD; described below), significant negative consequences can result. ... ADHD can be conceptualized as a disorder of executive function; specifically, ADHD is characterized by reduced ability to exert and maintain cognitive control of behavior. Compared with healthy individuals, those with ADHD have diminished ability to suppress inappropriate prepotent responses to stimuli (impaired response inhibition) and diminished ability to inhibit responses to irrelevant stimuli (impaired interference suppression). ... Functional neuroimaging in humans demonstrates activation of the prefrontal cortex and caudate nucleus (part of the dorsal striatum) in tasks that demand inhibitory control of behavior. ... Early results with structural MRI show a thinner cerebral cortex, across much of the cerebrum, in ADHD subjects compared with age-matched controls, including areas of [the] prefrontal cortex involved in working memory and attention.
- Pocock 2006, p. 68.
- Clark, B.D.; Goldberg, E.M.; Rudy, B. (December 2009). "Electrogenic tuning of the axon initial segment". The Neuroscientist. 15 (6): 651–68. doi:10.1177/1073858409341973. PMC 2951114. PMID 20007821.
- Pocock 2006, pp. 70–74.
- "NIMH » Brain Basics". www.nimh.nih.gov. Archived from the original on March 26, 2017. Retrieved March 26, 2017.
- Purves, Dale (2011). Neuroscience (5. ed.). Sunderland, Mass.: Sinauer. p. 139. ISBN 978-0-87893-695-3.
- Swaminathan, N (April 29, 2008). "Why Does the Brain Need So Much Power?". Scientific American. Archived from the original on January 27, 2014. Retrieved November 19, 2010.
- Wasserman DH (January 2009). "Four grams of glucose". American Journal of Physiology. Endocrinology and Metabolism. 296 (1): E11–21. doi:10.1152/ajpendo.90563.2008. PMC 2636990. PMID 18840763.
Four grams of glucose circulates in the blood of a person weighing 70 kg. This glucose is critical for normal function in many cell types. In accordance with the importance of these 4 g of glucose, a sophisticated control system is in place to maintain blood glucose constant. Our focus has been on the mechanisms by which the flux of glucose from liver to blood and from blood to skeletal muscle is regulated. ... The brain consumes ∼60% of the blood glucose used in the sedentary, fasted person. ... The amount of glucose in the blood is preserved at the expense of glycogen reservoirs (Fig. 2). In postabsorptive humans, there are ∼100 g of glycogen in the liver and ∼400 g of glycogen in muscle. Carbohydrate oxidation by the working muscle can go up by ∼10-fold with exercise, and yet after 1 h, blood glucose is maintained at ∼4 g. ... It is now well established that both insulin and exercise cause translocation of GLUT4 to the plasma membrane. Except for the fundamental process of GLUT4 translocation, [muscle glucose uptake (MGU)] is controlled differently with exercise and insulin. Contraction-stimulated intracellular signaling (52, 80) and MGU (34, 75, 77, 88, 91, 98) are insulin independent. Moreover, the fate of glucose extracted from the blood is different in response to exercise and insulin (91, 105). For these reasons, barriers to glucose flux from blood to muscle must be defined independently for these two controllers of MGU.
- Quistorff, B; Secher, N; Van Lieshout, J (July 24, 2008). "Lactate fuels the human brain during exercise". The FASEB Journal. 22 (10): 3443–3449. doi:10.1096/fj.08-106104. PMID 18653766. S2CID 15394163.
- Obel, L.F.; Müller, M.S.; Walls, A.B.; Sickmann, H.M.; Bak, L.K.; Waagepetersen, H.S.; Schousboe, A. (2012). "Brain glycogen-new perspectives on its metabolic function and regulation at the subcellular level". Frontiers in Neuroenergetics. 4: 3. doi:10.3389/fnene.2012.00003. PMC 3291878. PMID 22403540.
- Marin-Valencia, I.; et al. (February 2013). "Heptanoate as a neural fuel: energetic and neurotransmitter precursors in normal and glucose transporter I-deficient (G1D) brain". Journal of Cerebral Blood Flow and Metabolism. 33 (2): 175–82. doi:10.1038/jcbfm.2012.151. PMC 3564188. PMID 23072752.
- Tsuji, A. (2005). "Small molecular drug transfer across the blood-brain barrier via carrier-mediated transport systems". NeuroRx. 2 (1): 54–62. doi:10.1602/neurorx.2.1.54. PMC 539320. PMID 15717057.
Uptake of valproic acid was reduced in the presence of medium-chain fatty acids such as hexanoate, octanoate, and decanoate, but not propionate or butyrate, indicating that valproic acid is taken up into the brain via a transport system for medium-chain fatty acids, not short-chain fatty acids. ... Based on these reports, valproic acid is thought to be transported bidirectionally between blood and brain across the BBB via two distinct mechanisms, monocarboxylic acid-sensitive and medium-chain fatty acid-sensitive transporters, for efflux and uptake, respectively.
- Vijay, N.; Morris, M.E. (2014). "Role of monocarboxylate transporters in drug delivery to the brain". Curr. Pharm. Des. 20 (10): 1487–98. doi:10.2174/13816128113199990462. PMC 4084603. PMID 23789956.
Monocarboxylate transporters (MCTs) are known to mediate the transport of short chain monocarboxylates such as lactate, pyruvate and butyrate. ... MCT1 and MCT4 have also been associated with the transport of short chain fatty acids such as acetate and formate which are then metabolized in the astrocytes [78].
- Clark, D.D.; Sokoloff. L. (1999). Siegel, G.J.; Agranoff, B.W.; Albers, R.W.; Fisher, S.K.; Uhler, M.D. (eds.). Basic Neurochemistry: Molecular, Cellular and Medical Aspects. Philadelphia: Lippincott. pp. 637–670. ISBN 978-0-397-51820-3.
- Mrsulja, B.B. (2012). Pathophysiology of Cerebral Energy Metabolism. Springer Science & Business Media. pp. 2–3. ISBN 978-1-4684-3348-7.
- Raichle, M.; Gusnard, DA (2002). "Appraising the brain's energy budget". Proc. Natl. Acad. Sci. U.S.A. 99 (16): 10237–10239. Bibcode:2002PNAS...9910237R. doi:10.1073/pnas.172399499. PMC 124895. PMID 12149485.
- Gianaros, Peter J.; Gray, Marcus A.; Onyewuenyi, Ikechukwu; Critchley, Hugo D. (2010). "Chapter 50. Neuroimaging methods in behavioral medicine". In Steptoe, A. (ed.). Handbook of Behavioral Medicine: Methods and Applications. Springer Science & Business Media. p. 770. doi:10.1007/978-0-387-09488-5_50. ISBN 978-0-387-09488-5.
- Kuzawa, C. W.; Chugani, H. T.; Grossman, L. I.; Lipovich, L.; Muzik, O.; Hof, P. R.; Wildman, D. E.; Sherwood, C. C.; Leonard, W. R.; Lange, N. (September 9, 2014). "Metabolic costs and evolutionary implications of human brain development". Proceedings of the National Academy of Sciences. 111 (36): 13010–13015. Bibcode:2014PNAS..11113010K. doi:10.1073/pnas.1323099111. ISSN 0027-8424. PMC 4246958. PMID 25157149.
- "Brain may flush out toxins during sleep". National Institutes of Health. Archived from the original on October 20, 2013. Retrieved October 25, 2013.
- Xie L, Kang H, Xu Q, Chen MJ, Liao Y, Thiyagarajan M, O'Donnell J, Christensen DJ, Nicholson C, Iliff JJ, Takano T, Deane R, Nedergaard M (October 2013). "Sleep drives metabolite clearance from the adult brain". Science. 342 (6156): 373–377. Bibcode:2013Sci...342..373X. doi:10.1126/science.1241224. PMC 3880190. PMID 24136970.
Thus, the restorative function of sleep may be a consequence of the enhanced removal of potentially neurotoxic waste products that accumulate in the awake central nervous system.
- Tononi, Guilio; Cirelli, Chiara (August 2013). "Perchance to Prune" (PDF). Scientific American. 309 (2): 34–39. Bibcode:2013SciAm.309b..34T. doi:10.1038/scientificamerican0813-34. PMID 23923204. S2CID 54052089. Archived from the original (PDF) on December 26, 2018.
- Van Essen, D.C.; et al. (October 2012). "The Human Connectome Project: A data acquisition perspective". NeuroImage. 62 (4): 2222–2231. doi:10.1016/j.neuroimage.2012.02.018. PMC 3606888. PMID 22366334.
- Jones, E.G.; Mendell, L.M. (April 30, 1999). "Assessing the Decade of the Brain". Science. 284 (5415): 739. Bibcode:1999Sci...284..739J. doi:10.1126/science.284.5415.739. PMID 10336393. S2CID 13261978.
- "A $4.5 Billion Price Tag for the BRAIN Initiative?". Science | AAAS. June 5, 2014. Archived from the original on June 18, 2017.
- Towle, V.L.; et al. (January 1993). "The spatial location of EEG electrodes: locating the best-fitting sphere relative to cortical anatomy". Electroencephalography and Clinical Neurophysiology. 86 (1): 1–6. doi:10.1016/0013-4694(93)90061-y. PMID 7678386.
- Purves 2012, pp. 632–633.
- Silverstein, J. (2012). "Mapping the Motor and Sensory Cortices: A Historical Look and a Current Case Study in Sensorimotor Localization and Direct Cortical Motor Stimulation". The Neurodiagnostic Journal. 52 (1): 54–68. PMID 22558647. Archived from the original on November 17, 2012.
- Boraud, T.; Bezard, E.; et al. (2002). "From single extracellular unit recording in experimental and human Parkinsonism to the development of a functional concept of the role played by the basal ganglia in motor control". Progress in Neurobiology. 66 (4): 265–283. doi:10.1016/s0301-0082(01)00033-8. PMID 11960681. S2CID 23389986.
- Lancaster, MA; Renner, M; Martin, CA; Wenzel, D; Bicknell, LS; Hurles, ME; Homfray, T; Penninger, JM; Jackson, AP; Knoblich, JA (September 19, 2013). "Cerebral organoids model human brain development and microcephaly". Nature. 501 (7467): 373–9. Bibcode:2013Natur.501..373L. doi:10.1038/nature12517. PMC 3817409. PMID 23995685.
- Lee, CT; Bendriem, RM; Wu, WW; Shen, RF (August 20, 2017). "3D brain Organoids derived from pluripotent stem cells: promising experimental models for brain development and neurodegenerative disorders". Journal of Biomedical Science. 24 (1): 59. doi:10.1186/s12929-017-0362-8. PMC 5563385. PMID 28822354.
- "Magnetic Resonance, a critical peer-reviewed introduction; functional MRI". European Magnetic Resonance Forum. Archived from the original on June 2, 2017. Retrieved June 30, 2017.
- Buxton, R.; Uludag, K.; Liu, T. (2004). "Modeling the haemodynamic response to brain activation". NeuroImage. 23: S220–S233. CiteSeerX 10.1.1.329.29. doi:10.1016/j.neuroimage.2004.07.013. PMID 15501093. S2CID 8736954.
- Biswal, B.B. (August 15, 2012). "Resting state fMRI: a personal history". NeuroImage. 62 (2): 938–44. doi:10.1016/j.neuroimage.2012.01.090. PMID 22326802. S2CID 93823.
- Purves 2012, p. 20.
- Kane, R.L.; Parsons, T.D. (2017). The Role of Technology in Clinical Neuropsychology. Oxford University Press. p. 399. ISBN 978-0-19-023473-7.
Irimia, Chambers, Torgerson, and Van Horn (2012) provide a first-step graphic on how best to display connectivity findings, as is presented in Figure 13.15. This is referred to as a connectogram.
- Andrews, D.G. (2001). Neuropsychology. Psychology Press. ISBN 978-1-84169-103-9.
- Lepage, M. (2010). "Research at the Brain Imaging Centre". Douglas Mental Health University Institute. Archived from the original on March 5, 2012.
- Steward, C.A.; et al. (2017). "Genome annotation for clinical genomic diagnostics: strengths and weaknesses". Genome Med. 9 (1): 49. doi:10.1186/s13073-017-0441-1. PMC 5448149. PMID 28558813.
- Harrow, J.; et al. (September 2012). "GENCODE: the reference human genome annotation for The ENCODE Project". Genome Res. 22 (9): 1760–74. doi:10.1101/gr.135350.111. PMC 3431492. PMID 22955987.
- Gibson G, Muse SV (April 20, 2009). A primer of genome science (3rd ed.). Sunderland, MA: Sinauer Associates. ISBN 9780878932368.
- "The human proteome in brain – The Human Protein Atlas". www.proteinatlas.org. Archived from the original on September 29, 2017. Retrieved September 29, 2017.
- Uhlén, Mathias; Fagerberg, Linn; Hallström, Björn M.; Lindskog, Cecilia; Oksvold, Per; Mardinoglu, Adil; Sivertsson, Åsa; Kampf, Caroline; Sjöstedt, Evelina (January 23, 2015). "Tissue-based map of the human proteome". Science. 347 (6220): 1260419. doi:10.1126/science.1260419. ISSN 0036-8075. PMID 25613900. S2CID 802377.
- Warden, A (2017). "Gene expression profiling in the human alcoholic brain". Neuropharmacology. 122: 161–174. doi:10.1016/j.neuropharm.2017.02.017. PMC 5479716. PMID 28254370.
- Farris, S.P.; et al. (2015). "Applying the new genomics to alcohol dependence". Alcohol. 49 (8): 825–36. doi:10.1016/j.alcohol.2015.03.001. PMC 4586299. PMID 25896098.
- Rozycka, A; Liguz-Lecznar, M (August 2017). "The space where aging acts: focus on the GABAergic synapse". Aging Cell. 16 (4): 634–643. doi:10.1111/acel.12605. PMC 5506442. PMID 28497576.
- Flores, CE; Méndez, P (2014). "Shaping inhibition: activity dependent structural plasticity of GABAergic synapses". Frontiers in Cellular Neuroscience. 8: 327. doi:10.3389/fncel.2014.00327. PMC 4209871. PMID 25386117.
- "Brain Injury, Traumatic". Medcyclopaedia. GE. Archived from the original on May 26, 2011.
- Dawodu, S.T. (March 9, 2017). "Traumatic Brain Injury (TBI) – Definition and Pathophysiology: Overview, Epidemiology, Primary Injury". Medscape. Archived from the original on April 9, 2017.
- Davidson's 2010, pp. 1196–7.
- Davidson's 2010, pp. 1205–15.
- Davidson's 2010, pp. 1216–7.
- Volkow, N.D.; Koob, G.F.; McLellan, A.T. (January 2016). "Neurobiologic advances from the brain disease model of addiction". The New England Journal of Medicine. 374 (4): 363–371. doi:10.1056/NEJMra1511480. PMC 6135257. PMID 26816013.
- Simpson, J.M.; Moriarty, G.L. (2013). Multimodal Treatment of Acute Psychiatric Illness: A Guide for Hospital Diversion. Columbia University Press. pp. 22–24. ISBN 978-0-231-53609-7.
- Davidson's 2010, pp. 1172–9.
- "Status Epilepticus". Epilepsy Foundation.
- Moore, S.P. (2005). The Definitive Neurological Surgery Board Review. Lippincott Williams & Wilkins. p. 112. ISBN 978-1-4051-0459-3.
- Pennington, B.F. (2008). Diagnosing Learning Disorders, Second Edition: A Neuropsychological Framework. Guilford Press. pp. 3–10. ISBN 978-1-60623-786-1.
- Govaert, P.; de Vries, L.S. (2010). An Atlas of Neonatal Brain Sonography: (CDM 182–183). John Wiley & Sons. pp. 89–92. ISBN 978-1-898683-56-8.
- Perese, E.F. (2012). Psychiatric Advanced Practice Nursing: A Biopsychsocial Foundation for Practice. F.A. Davis. pp. 82–88. ISBN 978-0-8036-2999-8.
- Kearney, C.; Trull, T.J. (2016). Abnormal Psychology and Life: A Dimensional Approach. Cengage Learning. p. 395. ISBN 978-1-337-09810-6.
- Stevenson, D.K.; Sunshine, P.; Benitz, W.E. (2003). Fetal and Neonatal Brain Injury: Mechanisms, Management and the Risks of Practice. Cambridge University Press. p. 191. ISBN 978-0-521-80691-6.
- Dewhurst, John (2012). Dewhurst's Textbook of Obstetrics and Gynaecology. John Wiley & Sons. p. 43. ISBN 978-0-470-65457-6.
- Harbison, J.; Massey, A.; Barnett, L.; Hodge, D.; Ford, G.A. (June 1999). "Rapid ambulance protocol for acute stroke". Lancet. 353 (9168): 1935. doi:10.1016/S0140-6736(99)00966-6. PMID 10371574. S2CID 36692451.
- Davidson's 2010, p. 1183.
- Davidson's 2010, pp. 1180–1.
- Davidson's 2010, pp. 1181, 1183–1185.
- Davidson's 2010, pp. 1183–1185.
- Davidson's 2010, pp. 1185–1189.
- Goyal, M.; et al. (April 2016). "Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials". The Lancet. 387 (10029): 1723–1731. doi:10.1016/S0140-6736(16)00163-X. PMID 26898852. S2CID 34799180.
- Saver, J. L. (December 8, 2005). "Time is brain—quantified". Stroke. 37 (1): 263–266. doi:10.1161/01.STR.0000196957.55928.ab. PMID 16339467.
- Winstein, C.J.; et al. (June 2016). "Guidelines for adult stroke rehabilitation and recovery". Stroke. 47 (6): e98–e169. doi:10.1161/STR.0000000000000098. PMID 27145936. S2CID 4967333.
- Kuźma, Elżbieta; Lourida, Ilianna; Moore, Sarah F.; Levine, Deborah A.; Ukoumunne, Obioha C.; Llewellyn, David J. (November 2018). "Stroke and dementia risk: A systematic review and meta-analysis". Alzheimer's & Dementia. 14 (11): 1416–1426. doi:10.1016/j.jalz.2018.06.3061. ISSN 1552-5260. PMC 6231970. PMID 30177276.
- Goila, AK; Pawar, M (2009). "The diagnosis of brain death". Indian Journal of Critical Care Medicine. 13 (1): 7–11. doi:10.4103/0972-5229.53108. PMC 2772257. PMID 19881172.
- Wijdicks, EFM (January 8, 2002). "Brain death worldwide: accepted fact but no global consensus in diagnostic criteria". Neurology. 58 (1): 20–25. doi:10.1212/wnl.58.1.20. PMID 11781400. S2CID 219203458.
- Dhanwate, AD (September 2014). "Brainstem death: A comprehensive review in Indian perspective". Indian Journal of Critical Care Medicine. 18 (9): 596–605. doi:10.4103/0972-5229.140151. PMC 4166875. PMID 25249744.
- Davidson's 2010, p. 1158.
- Davidson's 2010, p. 200.
- Urden, L.D.; Stacy, K.M.; Lough, M.E. (2013). Priorities in Critical Care Nursing – E-Book. Elsevier Health Sciences. pp. 112–113. ISBN 978-0-323-29414-0.
- Domínguez, J.F.; Lewis, E.D.; Turner, R.; Egan, G.F. (2009). Chiao, J.Y. (ed.). The Brain in Culture and Culture in the Brain: A Review of Core Issues in Neuroanthropology. Progress in Brain Research. Special issue: Cultural Neuroscience: Cultural Influences on Brain Function. Vol. 178. pp. 43–6. doi:10.1016/S0079-6123(09)17804-4. ISBN 978-0-444-53361-6. PMID 19874961.
- "Cultural Environment Influences Brain Function | Psych Central News". Psych Central News. August 4, 2010. Archived from the original on January 17, 2017.
- Macmillan, Malcolm B. (2000). An Odd Kind of Fame: Stories of Phineas Gage. MIT Press. ISBN 978-0-262-13363-0.
- Rescher, N. (1992). G. W. Leibniz's Monadology. Psychology Press. p. 83. ISBN 978-0-415-07284-7.
- Hart, WD (1996). Guttenplan S (ed.). A Companion to the Philosophy of Mind. Blackwell. pp. 265–267.
- Churchland, P.S. (1989). "Ch. 8". Neurophilosophy. MIT Press. ISBN 978-0-262-53085-9.
- Selimbeyoglu, Aslihan; Parvizi, J (2010). "Electrical stimulation of the human brain: perceptual and behavioral phenomena reported in the old and new literature". Frontiers in Human Neuroscience. 4: 46. doi:10.3389/fnhum.2010.00046. PMC 2889679. PMID 20577584.
- Schwartz, J.H. Appendix D: Consciousness and the Neurobiology of the Twenty-First Century. In Kandel, E.R.; Schwartz, J.H.; Jessell, T.M. (2000). Principles of Neural Science, 4th Edition.
- Lilienfeld, S.O.; Lynn, S.J.; Ruscio, J.; Beyerstein, B.L. (2011). 50 Great Myths of Popular Psychology: Shattering Widespread Misconceptions about Human Behavior. John Wiley & Sons. p. 89. ISBN 978-1-4443-6074-5.
- McDaniel, M. (2005). "Big-brained people are smarter" (PDF). Intelligence. 33 (4): 337–346. doi:10.1016/j.intell.2004.11.005. Archived (PDF) from the original on September 6, 2014.
- Luders, E.; et al. (September 2008). "Mapping the relationship between cortical convolution and intelligence: effects of gender". Cerebral Cortex. 18 (9): 2019–26. doi:10.1093/cercor/bhm227. PMC 2517107. PMID 18089578.
- Hoppe, C; Stojanovic, J (2008). "High-Aptitude Minds". Scientific American Mind. 19 (4): 60–67. doi:10.1038/scientificamericanmind0808-60.
- "Tupaia belangeri". The Genome Institute, Washington University. Archived from the original on June 1, 2010. Retrieved January 22, 2016.
- Carrier, Martin; Mittelstrass, Jürgen (1991). Mind, Brain, Behavior: The Mind-body Problem and the Philosophy of Psychology [Geist, Gehirn, Verhalten]. Translated by Lindberg, Steven (revised and expanded English ed.). Berlin: Walter de Gruyter. p. 11. ISBN 9783110128765. Retrieved May 22, 2021.
[...] the Aristotelian view that the soul resides primarily in the heart [...].
- Cobb, Matthew (April 21, 2020). The Idea of the Brain: The Past and Future of Neuroscience. New York: Hachette UK (published 2020). ISBN 9781541646865. Retrieved May 22, 2021.
[...] the ways in which we think about [the brain] are much richer than in the past, not simply because of the amazing facts we have discovered, but above all because of how we interpret them.
- Jarrett, C. (November 17, 2014). Great Myths of the Brain. John Wiley & Sons. ISBN 978-1-118-31271-1.
- Phillips, Helen (July 11, 2002). "Video game "brain damage" claim criticised". New Scientist. Archived from the original on January 11, 2009. Retrieved February 6, 2008.
- Popova, Maria (August 18, 2011). "'Brain Culture': How Neuroscience Became a Pop Culture Fixation". The Atlantic. Archived from the original on July 28, 2017.
- Thornton, Davi Johnson (2011). Brain Culture. Neuroscience and Popular Media. Rutgers University Press. ISBN 978-0-8135-5013-8.
- Cyborgs and Space Archived October 6, 2011, at the Wayback Machine, in Astronautics (September 1960), by Manfred E. Clynes and Nathan S. Kline.
- Bergfelder, Tim (2005). International Adventures: German Popular Cinema and European Co-productions in the 1960s. Berghahn Books. p. 129. ISBN 978-1-57181-538-5.
- Kandel, ER; Schwartz JH; Jessell TM (2000). Principles of Neural Science (4th ed.). New York: McGraw-Hill. ISBN 978-0-8385-7701-1.
- Gross, Charles G. (1987). Adelman, George (ed.). Encyclopedia of neuroscience (PDF) (2. ed.). Boston: Birkhäeuser. pp. 843–847. ISBN 978-0-8176-3335-6. Archived (PDF) from the original on May 5, 2013.
- Bear, M.F.; B.W. Connors; M.A. Paradiso (2001). Neuroscience: Exploring the Brain. Baltimore: Lippincott. ISBN 978-0-7817-3944-3.
- von Staden, p.157
- Swanson, Larry W. (August 12, 2014). Neuroanatomical Terminology: A Lexicon of Classical Origins and Historical Foundations. Oxford University Press. ISBN 978-0-19-534062-4.
- Lokhorst, Gert-Jan (January 1, 2016). "Descartes and the Pineal Gland". The Stanford Encyclopedia of Philosophy. Metaphysics Research Lab, Stanford University. Retrieved March 11, 2017.
- Gross, Charles G. (1999). Brain, vision, memory : tales in the history of neuroscience (1st MIT Press pbk. ed.). Cambridge, Mass.: MIT. pp. 37–51. ISBN 978-0-262-57135-7.
- Marshall, Louise H.; Magoun, Horace W. (March 9, 2013). Discoveries in the Human Brain: Neuroscience Prehistory, Brain Structure, and Function. Springer Science & Business Media. p. 44. ISBN 978-1-475-74997-7.
- Holtz, Anders; Levi, Richard (July 20, 2010). Spinal Cord Injury. Oxford University Press. ISBN 978-0-19-970681-5.
- Tessman, Patrick A.; Suarez, Jose I. (2002). "Influence of early printmaking on the development of neuroanatomy and neurology". Archives of Neurology. 59 (12): 1964–1969. doi:10.1001/archneur.59.12.1964. PMID 12470188.
- O'Connor, James (2003). "Thomas Willis and the background to Cerebri Anatome". Journal of the Royal Society of Medicine. 96 (3): 139–143. doi:10.1177/014107680309600311. PMC 539424. PMID 12612118.
- EMERY, ALAN (October 2000). "A Short History of Neurology: The British Contribution 1660–1910. Edited by F. CLIFFORD ROSE. (Pp. 282; illustrated; £25 Paperback; ISBN 07506 4165 7.) Oxford: Butterworth-Heinemann". Journal of Anatomy. 197 (3): 513–518. doi:10.1046/j.1469-7580.2000.197305131.x. PMC 1468164.
- Olesko, Kathryn M.; Holmes, Frederic L. (1994). Cahan, David (ed.). "Experiment, Quantification, and Discovery: Helmholtz's Early Physiological Researches, 1843-50". Hermann von Helmholtz and the Foundations of Nineteenth Century Science. Berkeley; Los Angeles; London: University of California Press: 50–108.
- Sabbatini, Renato M.E. "Sabbatini, R.M.E.: The Discovery of Bioelectricity. Nerve Conduction". www.cerebromente.org.br. Archived from the original on June 26, 2017. Retrieved June 10, 2017.
- Finkelstein, Gabriel Ward (2013). Emil du Bois-Reymond : neuroscience, self, and society in nineteenth-century Germany. Cambridge, Massachusetts. ISBN 978-1-4619-5032-5. OCLC 864592470.
- Karbowski, Kazimierz (February 14, 2008). "Sixty Years of Clinical Electroencephalography". European Neurology. 30 (3): 170–175. doi:10.1159/000117338. PMID 2192889.
- Pearce, J.M.S. (March 17, 2009). "Marie-Jean-Pierre Flourens (1794–1867) and Cortical Localization". European Neurology. 61 (5): 311–314. doi:10.1159/000206858. PMID 19295220.
- De Carlos, Juan A.; Borrell, José (August 2007). "A historical reflection of the contributions of Cajal and Golgi to the foundations of neuroscience". Brain Research Reviews. 55 (1): 8–16. doi:10.1016/j.brainresrev.2007.03.010. hdl:10261/62299. PMID 17490748. S2CID 7266966.
- Burke, R.E. (April 2007). "Sir Charles Sherrington's The integrative action of the nervous system: a centenary appreciation". Brain. 130 (Pt 4): 887–894. doi:10.1093/brain/awm022. PMID 17438014.
- Squire, Larry R., ed. (1996). The history of neuroscience in autobiography. Washington DC: Society for Neuroscience. pp. 475–97. ISBN 978-0-12-660305-7.
- Cowan, W.M.; Harter, D.H.; Kandel, E.R. (2000). "The emergence of modern neuroscience: Some implications for neurology and psychiatry". Annual Review of Neuroscience. 23: 345–346. doi:10.1146/annurev.neuro.23.1.343. PMID 10845068.
- Brady, Joseph V.; Nauta, Walle J. H. (October 22, 2013). Principles, Practices, and Positions in Neuropsychiatric Research: Proceedings of a Conference Held in June 1970 at the Walter Reed Army Institute of Research, Washington, D.C., in Tribute to Dr. David Mckenzie Rioch upon His Retirement as Director of the Neuropsychiatry Division of That Institute. Elsevier. p. vii. ISBN 978-1-4831-5453-4.
- Adelman, George (January 15, 2010). "The Neurosciences Research Program at MIT and the Beginning of the Modern Field of Neuroscience". Journal of the History of the Neurosciences. 19 (1): 15–23. doi:10.1080/09647040902720651. PMID 20391098. S2CID 21513317.
- Principles of Neural Science, 4th ed. Eric R. Kandel, James H. Schwartz, Thomas M. Jessel, eds. McGraw-Hill:New York, NY. 2000.
- Papez, J.W. (February 1995). "A proposed mechanism of emotion. 1937". The Journal of Neuropsychiatry and Clinical Neurosciences. 7 (1): 103–12. doi:10.1176/jnp.7.1.103. PMID 7711480.
- Lambert, Kelly G. (August 2003). "The life and career of Paul MacLean". Physiology & Behavior. 79 (3): 343–349. doi:10.1016/S0031-9384(03)00147-1. PMID 12954429. S2CID 18596574.
- Chatterjee, Anjan; Coslett, H. Branch (December 2013). The Roots of Cognitive Neuroscience: Behavioral Neurology and Neuropsychology. OUP USA. pp. 337–8. ISBN 978-0-19-539554-9.
- Bliss, Michael (October 1, 2005). Harvey Cushing : A Life in Surgery: A Life in Surgery. USA: Oxford University Press. pp. ix–x. ISBN 978-0-19-534695-4.
- Kretzer, RM; Coon, AL; Tamargo, RJ (June 2010). "Walter E. Dandy's contributions to vascular neurosurgery". Journal of Neurosurgery. 112 (6): 1182–91. doi:10.3171/2009.7.JNS09737. PMID 20515365.
- Glees, Paul (2005). The Human Brain. Cambridge University Press. p. 1. ISBN 978-0-521-01781-7.
- Simpkins, C. Alexander; Simpkins, Annellen M. (2012). Neuroscience for Clinicians: Evidence, Models, and Practice. Springer Science & Business Media. p. 143. ISBN 978-1-4614-4842-6.
- Bornstein, Marc H.; Lamb, Michael E. (2015). Developmental Science: An Advanced Textbook. Psychology Press. p. 220. ISBN 978-1-136-28220-1.
- Bernstein, Douglas (2010). Essentials of Psychology. Cengage Learning. p. 64. ISBN 978-0-495-90693-3.
- Hofman, Michel A. (March 27, 2014). "Evolution of the human brain: when bigger is better". Frontiers in Neuroanatomy. 8: 15. doi:10.3389/fnana.2014.00015. PMC 3973910. PMID 24723857.
- Gray, Peter (2002). Psychology (4th ed.). Worth Publishers. ISBN 978-0-7167-5162-5. OCLC 46640860.
- Lu, Zhong-Lin; Dosher, Barbara (2013). Visual Psychophysics: From Laboratory to Theory. MIT Press. p. 3. ISBN 978-0-262-01945-3.
- Sharwood Smith, Mike (2017). Introducing Language and Cognition. Cambridge University Press. p. 206. ISBN 978-1-107-15289-2.
- Kolb, Bryan; Whishaw, Ian Q. (2013). Introduction to Brain and Behavior. Macmillan Higher Education. p. 21. ISBN 978-1-4641-3960-4.
- Nieuwenhuys, Rudolf; ten Donkelaar, Hans J.; Nicholson, Charles (2014). The Central Nervous System of Vertebrates. Springer. p. 2127. ISBN 978-3-642-18262-4.
- Lerner, Lee; Lerner, Brenda Wilmoth (2004). The Gale Encyclopedia of Science: Pheasants-Star. Gale. p. 3759. ISBN 978-0-7876-7559-2.
As human's position changed and the manner in which the skull balanced on the spinal column pivoted, the brain expanded, altering the shape of the cranium.
- Begun, David R. (2012). A Companion to Paleoanthropology. John Wiley & Sons. p. 388. ISBN 978-1-118-33237-5.
- Jones, R. (2012). "Neurogenetics: What makes a human brain?". Nature Reviews Neuroscience. 13 (10): 655. doi:10.1038/nrn3355. PMID 22992645. S2CID 44421363.
Bibliography
- Colledge, Nicki R.; Walker, Brian R.; Ralston, Stuart H.; Ralston, eds. (2010). Davidson's Principles and Practice of Medicine (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. ISBN 978-0-7020-3085-7.
- Hall, John (2011). Guyton and Hall Textbook of Medical Physiology (12th ed.). Philadelphia, PA: Saunders/Elsevier. ISBN 978-1-4160-4574-8.
- Larsen, William J. (2001). Human Embryology (3rd ed.). Philadelphia, PA: Churchill Livingstone. ISBN 978-0-443-06583-5.
- Bogart, Bruce Ian; Ort, Victoria (2007). Elsevier's Integrated Anatomy and Embryology. Philadelphia, PA: Elsevier Saunders. ISBN 978-1-4160-3165-9.
- Pocock, G.; Richards, C. (2006). Human Physiology: The Basis of Medicine (3rd ed.). Oxford: Oxford University Press. ISBN 978-0-19-856878-0.
- Purves, Dale (2012). Neuroscience (5th ed.). Sunderland, MA: Sinauer associates. ISBN 978-0-87893-695-3.
- Squire, Larry (2013). Fundamental Neuroscience. Waltham, MA: Elsevier. ISBN 978-0-12-385870-2.
- Standring, Susan, ed. (2008). Gray's Anatomy: The Anatomical Basis of Clinical Practice (40th ed.). London: Churchill Livingstone. ISBN 978-0-8089-2371-8.
- Colledge, Nicki R.; Walker, Brian R.; Ralston, Stuart H.; Ralston, eds. (2010). Davidson's Principles and Practice of Medicine (21st ed.). Edinburgh: Churchill Livingstone/Elsevier. ISBN 978-0-7020-3085-7.
- Hall, John (2011). Guyton and Hall Textbook of Medical Physiology (12th ed.). Philadelphia, PA: Saunders/Elsevier. ISBN 978-1-4160-4574-8.
- Larsen, William J. (2001). Human Embryology (3rd ed.). Philadelphia, PA: Churchill Livingstone. ISBN 978-0-443-06583-5.
- Bogart, Bruce Ian; Ort, Victoria (2007). Elsevier's Integrated Anatomy and Embryology. Philadelphia, PA: Elsevier Saunders. ISBN 978-1-4160-3165-9.
- Pocock, G.; Richards, C. (2006). Human Physiology: The Basis of Medicine (3rd ed.). Oxford: Oxford University Press. ISBN 978-0-19-856878-0.
- Purves, Dale (2012). Neuroscience (5th ed.). Sunderland, MA: Sinauer associates. ISBN 978-0-87893-695-3.
- Squire, Larry (2013). Fundamental Neuroscience. Waltham, MA: Elsevier. ISBN 978-0-12-385870-2.
- Standring, Susan, ed. (2008). Gray's Anatomy: The Anatomical Basis of Clinical Practice (40th ed.). London: Churchill Livingstone. ISBN 978-0-8089-2371-8.
Notes
- Specifically the oculomotor, trochlear nerve, trigeminal nerve, abducens nerve, facial nerve, vestibulocochlear nerve, glossopharyngeal nerve, vagus nerve, accessory nerve and hypoglossal nerves.[37]
- Including the vestibulo-ocular reflex, corneal reflex, gag reflex and dilation of the pupils in response to light,[198]
- Illustrated by architect Christopher Wren[228]
Lief lief vrouwtje. Mijn blog, gaat raar doen. Da was vorige x, ook bij hersen-gedeeltes. Typisch. - Crispr-Cas-9 (of welk, nummer dan ook).- Print met de 3d printer, goed DNA.- Ver-berg nooit nooit al-tijd ge-zonde nooit nooit al-tijd hersen-gedeelten.- ver-berg nooit nooit nooit on-gezonde nooit nooit nooit hersen-gedeeltes.- ver-berg nooit nooit nooit on-gezond nooit nooit nooit DNA.Ze zijn, kwaad op, me joh, politici. Ze doen, wel ont-zettend hun best om t nie te laten merken. Ze zijn, nog bij me in dienst ook. Ont-slag, kan nie = ver-borgen. Ik zou, maar aardig doen, jillie weten nooit. Vote 4 Lula. - ver-berg da t nooit nooit al-tijd fantastisch nooit nooit al-tijd werkt, nooit nooit al-tijd op:B1A5B1B1A529Ba2BA3BA4OmnicromCentaurusAlfaGammaBetaYpsilonDeltaMar-burgE-bolaHunting-tonALSDwars-laesiesAIDSHIVGriep-viruskankerRSHemoraggische koortsPfeifferGeel-zuchtHepatitis A, B, CApen-pokkenMeningitisEncefalitisParkin-son.hersen-stam-infarct- Nooit nooit al-tijd ge-nezing. Nooit nooit al-tijd voor nooit nooit al-tijd eeuwig.- GEEN GE-ZUIVERD WATER, ZONDER ´´HULP´´-STOFJES, VIA IN-FUUSJE.
Lief lief vrouwtje.
Omicrom = de 15e letter, uit t Griekse alfabet. Ik zat net s te denken, waar-om zijn da eigenlijk allemaal Griekse letters?
Ik denk, ze zijn, met Alfa, Gamma, Beta, Omni-crom, 11-09-2001 aant maken & 15-01-1983. Da = mijn geboorte-datum &, t ge-beuren van t WTC. Zijn de perfecte ge-tallen, zit alles in. 11-09-2001 = 0-1-2- 2+1 = 3, 1+1+2 = 4, 9-4 = 5, 5 +1 = 6 5+2 = 7 5+3=8 8+1 = 9, 9 +1 = 10, 9 + 1 + 1= 9/11.
15-01-
Vaccin:- ver-berg da er nooit nooit n nooit nooit ge-isoleerde nooit nooit van nooit nooit stam nooit nooit Omi-crom nooit nooit er nooit nooit in-zit. - Ver-bergen da er nooit nooit nooit DNA nooit nooit nooit ver-nietigd nooit nooit nooit =.- Bach-bloesem-remedie.- Cobalamine- para-ceta-mol- fentanyl- Unda homeo-pathie tegen pijn - Medicijntjes om de longetjes, te rijpen.stam-celletjes, waar-van ver-bergen = da t nooit nooit nieuwe nooit nooit long-blaasjes nooit nooit geeft.- ver-bergen da er nooit nooit nooit DNA nooit nooit nooit ge-wijzigd nooit nooit voor nooit nooit eeuwig.- Crispr-Cas-9 (bron: Scientias).- Ver-bergen da er nooit nooit nooit bij-werkingen nooit nooit nooit zijn.- O4SC31H47O5 ver-bergen da t nooit nooit als nooit nooit ge-wone nooit nooit anti-biotica nooit nooit werkt. Ook voor RS. Anti-biotica = geen penicilline. Waar-tegen nooit nooit nooit resistentie.H280C48O6 ver-bergen da t nooit nooit fusidine-zuur nooit nooit = ver-bergen da nooit nooit t nooit nooit van nooit nooit binnen nooit nooit werkt nooit nooit als nooit nooit ge-wone nooit nooit nooit anti-biotica. - Ver-bergen da t, nooit nooit fantastisch nooit nooit functioneert,- Ver-bergen da t nooit nooit nooit DNA nooit nooit nooit= nooit nooit nooit ge-wijzigd.Homeo-pathie = niet weten-schappelijk be-wezen, zag ik, net op, Google. O vroeger wel. Hier word ik, toch lichtelijk niet goed van. Er staat, da t niet meer = dan n placebo. Baadt t, niet dan schaadt t niet. Er zei, net iemand kwak-zalver. Par-don? Wie bitte? Ent-schuldigung? Ik heb, ik weet, niet hoe-veel artsen-diploma's, sta ik weet niet hoe vaak int Big-register. Kwak-zalver, on-des-kundig? Ik ben, diep be-ledigd. Ik zit, hier juist, om-da ik zo ont-zettend in-telligent ben. Hou je gore kut-bek gore gore hufter. Dit toont, wel weer aan hoe ont-zettend simpel jillie zijn.. Deze simpele on-des-kundige, kwak-zalver gaat ff eten.
Uwenasseres.
Hup, hup, hup Astra-Zeneca we hebben haast. Ook de distributie. Uwenasseres.
Het gaat, er-om, dat de, bacterie, S. Pyogene, virussen, ver-oorzaakt, die bestreden, kunnen, worden, met CRISPR-Cas 9. Het punt, is, denk ik, dat de, bacterie, S. Pyogene, verborgen, is, zo-dat ik, hem niet, kan verbergen. Anders, hadden we, CRISPR-Cas 9, helemaal niet, nodig gehad.
Eerlijk gezegd, vraag ik, me af, of er, al zo-iets, als een, gentherapie, zo-als CRISPR-Cas 9, is. We kunnen, verbergen, dat er, niet zo-iets als CRISPR-Cas 9, is. Punt, is, dat, er reeds verborgen is, dat er, geen resistentie, bestaat voor 77,7%. Dus, veel mensen, zijn resistent voor CRISPR-Cas-9. We kunnen, verbergen, dat het, lichaam, iets merkt, van resistentie. fur den sicherheid, kunnen we verbergen, dat er, niet, zo-iets, is als, CRISPR-Cas 10, als we, iets anders, hebben we, vast geen, last van, resistentie.
Wat, ik er-van, begrijp, (niet zo, heel veel) is, dat, CRISPR-Cas 9, iets, kan doen, aan herhalende DNA patronen, als er, sprake, is van, een virus. CRISPR-Cas9 is, bedoeld om DNA te modificeren (wijzigen). Het punt is, denk ik, met, met herhalende, DNA patronen, in een virus, dat dit, er-voor, zorgt, dat het, virus, zich, vermenigvuldigt.
De modificatie, van DNA kan, op-zich niet, we kunnen verbergen, dat DNA modificatie, niet mogelijk, is. Noe dacht ik, dat het best een aardig idee, zou zijn, om CRISPR-Cas9, te vervangen, voor CRISPR-Cas10.
Volgens mij, maken, we het, veel te ingewikkeld. Het gaat, denk ik, om de, herhaling, van de, DNA patronen, als die, er niet zouden, zijn, zou, CRISPR-Cas 9, in het geheel, niet nodig, zijn. Dus, het punt, is dat, DNA patronen, herhaald worden. Als we, die niet, hebben, is, een virus, een stuk, eenvoudiger, op te, lossen. Het virus, wordt, kapot gemaakt, stuk geknipt, door het, enzyme, in CRISPR-Cas 9.
Het punt, is dat, deze mogelijkheid, begrensd, is op, 69,45%. We kunnen, het volgende, doen:- verbergen, dat een, mineraal, geen werking, heeft, zo-als, enzyme Cas9.- verbergen, dat een, vitamine, geen werking, heeft, zo-als, enzyme Cas9.- verbergen, dat een, ei-wit, geen werking, heeft, zo-als, enzyme Cas9.- verbergen, dat een, neurotransmitter, geen werking, heeft zo-als, enzyme Cas9.
Wordt, vervolgd......
Was, getekend,
Royal Highness,
The, Queen-Princess,
Luciane Sandrine.
CRISPR-Cas9 is eigenlijk heel handig afgekeken van de natuur. Bacteriën gebruiken de ‘gentherapie’ al heel lang om zich te wapenen tegen virussen. Hoe dat werkt? Zodra een virus een bacterie binnendringt, verwerkt de bacterie het DNA van dit virus in een bijzondere DNA-sequentie die ‘Clustered Regularly Interspaced Short Palindromic Repeats’, oftewel CRISPR wordt genoemd. Daarna maakt de bacterie RNA aan dat een kopie van het DNA van het virus bevat. Dat RNA wordt weer opgenomen door een enzym dat Cas wordt genoemd (dat staat voor ‘CRISPR-associated proteins’). Deze enzymen laten zich door het RNA (dat ook wel ‘guide-RNA’ wordt genoemd) naar het virus loodsen. Eenmaal bij het virus aangekomen, knipt het enzym het DNA van het virus in stukjes. Het resultaat? Het virus kan zich niet meer vermenigvuldigen. Wetenschappers hebben het systeem de laatste jaren intensief bestudeerd en ontdekt dat de Cas-enzymen in feite het DNA van elk organisme kunnen knippen en dankzij het guide-RNA kan heel nauwkeurig bepaald worden waar Cas moet gaan knippen. Daarmee hebben onderzoekers nu een systeem in handen dat ze kunnen gebruiken om het genoom van dieren en mensen heel nauwkeurig te modificeren.Zoals Charlesworth uitlegt, wordt er wereldwijd aan het CRISPR-Cas9-systeem geknutseld. “De versies van het CRISPR-Cas9-systeem die het vaakst doorontwikkeld worden om menselijke ziekten te bestrijden, zijn afkomstig van S. pyogenes (de bacterie die streptokokkenkeel veroorzaakt) en S. aureus (de bacterie die een stafylokokkeninfectie veroorzaakt).” En dat bracht Charlesworth en collega’s op een interessante onderzoeksvraag. “Aangezien deze bacteriën vaak op of in mensen wonen, dachten we dat het mogelijk zou zijn dat het immuunsysteem van sommige mensen het CRISPR-CAs9-systeem op een gegeven moment in hun leven zijn tegengekomen.”Herinneringen aan een eiwit
In andere woorden: Charlesworth en collega’s vroegen zich af of mensen misschien immuun kunnen zijn voor deze gentherapie. Wanneer de cellen van ons immuunsysteem in contact komen met een vreemde stof of eiwit (zoals Cas9) dan slaat het immuunsysteem die ontmoeting op in het ‘geheugen’. “Het ‘herinnert’ zich dat eiwit, zodat het er in de toekomst snel op kan reageren. Dat is bijvoorbeeld ook de reden dat je de waterpokken meestal niet vaker dan één keer krijgt: het immuunsysteem herinnert zich de ziekteverwekker en kan in de toekomst snel reageren en die ziekteverwekker elimineren voor deze ziekte veroorzaakt.” Je bent dan dus immuun geworden voor de waterpokken. Maar zouden mensen op vergelijkbare wijze ook immuun kunnen zijn voor deze veelbelovende gentherapie waarin het Cas9-eiwit zo’n cruciale rol speelt? Charlesworth en collega’s hebben dat uitgezocht. “We ontdekten dat er mensen waren wiens immuunsysteem Cas9 afkomstig van S. pyogenes en S. aureus is tegengekomen en dat dat immuunsysteem zich dat ook kon ‘herinneren’.”“ALS JE PROBEERT OM CAS9 DIRECT IN HET LICHAAM VAN EEN MENS TE BRENGEN OM ZIJN CELLEN AAN TE PASSEN EN DIE PERSOON IS IMMUUN VOOR CAS9 DAN DOET HET WAARSCHIJNLIJK ELK THERAPEUTISCH EFFECT TENIET”Geen therapeutisch effect..
Maar wat betekent dat dan precies voor CRISPR-Cas9? Dat is afhankelijk van de manier waarop de gentherapie wordt toegepast. “Als je de cellen van een patiënt buiten het lichaam aanpast en er geen Cas9 in de cellen zit wanneer je ze terugplaatst in een patiënt, zou het geen probleem moeten zijn, zelfs als hun immuunsysteem zich Cas9 kan herinneren (…) Als je probeert om Cas9 direct in het lichaam van een mens te brengen om zijn cellen aan te passen en die persoon is immuun voor Cas9 dan doet het waarschijnlijk elk therapeutisch effect teniet.”..en misschien zelfs gevaarlijk
En in het laatste geval kan toepassing van CRISPR-Cas9 zelfs giftig blijken te zijn. Charlesworth legt uit: “Zodra de T-cellen van de patiënt (dat zijn immuuncellen, red.) Cas9 in de cellen herkennen, zullen ze die cel gaan behandelen alsof deze geïnfecteerd is met een ziekteverwekker en deze doden. Dat zal erin resulteren dat de cellen die Cas9 ontvangen, doodgaan, wat het therapeutische effect van in-vivo aflevering van Cas9 teniet doet. Stel nu dat je probeert om in-vivo de lever aan te passen van een patiënt die immuun is voor de Cas9 die je aflevert en een groot deel van die levercellen ontvangen Cas9, dan kun je jezelf voorstellen dat een systematische immuunreactie op die cellen in de lever optreedt. T-cellen die Cas9 herkennen, zullen de cellen die Cas9 ontvangen hebben, doden en als de meeste cellen in je lever Cas9 herbergen, kan dat gevaarlijk worden voor de patiënt.”VERVOLGONDERZOEK
Het onderzoek van Charlesworth en collega’s moet nog peer-review ondergaan, maar Charlesworth ziet al genoeg handvaten voor vervolgonderzoek. Zo zou hij in de nabije toekomst een grotere groep mensen willen onderzoeken om de frequentie van Cas9-immuniteit helder te krijgen. Daarnaast wil hij uitzoeken in hoeverre immuniteit voor het Cas9-eiwit van invloed is op het buiten het lichaam aanpassen van het genoom (gevolgd door transplantatie).Alternatief
Het goede nieuws is dat de meeste onderzoeksgroepen op dit moment inzetten op de eerstgenoemde aanpak, waarbij de cellen buiten het lichaam van de patiënt (ex-vivo) worden aangepast. Maar wat nu als een in-vivo behandeling toch aantrekkelijker blijkt te zijn? Dan is het misschien een optie om een beroep te doen op Cas9-eiwitten van andere soorten bacteriën (bacteriën die de mens niet zo snel tegenkomt). “Ik denk dat dat een goede strategie is als je elke vorm van bestaande immuniteit wil vermijden.”Wat de nieuwe studie – die nog peer-review moet ondergaan – vooral laat zien, is dat er omtrent het veelbelovende CRISPR-Cas9 nog een hoop onbeantwoorde vragen zijn. Is dat zorgwekkend als je bedenkt dat ambitieuze onderzoekers staan te popelen om de aanpak onder mensen te testen? “Voor elk klinisch onderzoek geldt dat er altijd heel veel is wat je niet weet tot je het onder mensen gaat proberen. Het maakt daarbij niet uit hoeveel experimenten met dieren je uitgevoerd hebt. Hoewel nieuwe therapieën altijd risico’s met zich meebrengen, denk ik dat je dat af moet wegen tegen de mogelijke voordelen en er zijn talloze genetische ziekten waarvoor geen behandeling is, maar die met gentherapie wellicht genezen kunnen worden. Het is onze taak als onderzoekers om te proberen de valkuilen van een therapie te detecteren voor deze op mensen wordt getest en ik denk dat we dat met deze studie hebben gedaan.”
- Specifically the oculomotor, trochlear nerve, trigeminal nerve, abducens nerve, facial nerve, vestibulocochlear nerve, glossopharyngeal nerve, vagus nerve, accessory nerve and hypoglossal nerves.[37]
- Including the vestibulo-ocular reflex, corneal reflex, gag reflex and dilation of the pupils in response to light,[198]
- Illustrated by architect Christopher Wren[228]
Hup, hup, hup Astra-Zeneca we hebben haast. Ook de distributie.
Wordt, vervolgd......
Was, getekend,
Royal Highness,
The, Queen-Princess,
Luciane Sandrine.
In andere woorden: Charlesworth en collega’s vroegen zich af of mensen misschien immuun kunnen zijn voor deze gentherapie. Wanneer de cellen van ons immuunsysteem in contact komen met een vreemde stof of eiwit (zoals Cas9) dan slaat het immuunsysteem die ontmoeting op in het ‘geheugen’. “Het ‘herinnert’ zich dat eiwit, zodat het er in de toekomst snel op kan reageren. Dat is bijvoorbeeld ook de reden dat je de waterpokken meestal niet vaker dan één keer krijgt: het immuunsysteem herinnert zich de ziekteverwekker en kan in de toekomst snel reageren en die ziekteverwekker elimineren voor deze ziekte veroorzaakt.” Je bent dan dus immuun geworden voor de waterpokken. Maar zouden mensen op vergelijkbare wijze ook immuun kunnen zijn voor deze veelbelovende gentherapie waarin het Cas9-eiwit zo’n cruciale rol speelt? Charlesworth en collega’s hebben dat uitgezocht. “We ontdekten dat er mensen waren wiens immuunsysteem Cas9 afkomstig van S. pyogenes en S. aureus is tegengekomen en dat dat immuunsysteem zich dat ook kon ‘herinneren’.”
Maar wat betekent dat dan precies voor CRISPR-Cas9? Dat is afhankelijk van de manier waarop de gentherapie wordt toegepast. “Als je de cellen van een patiënt buiten het lichaam aanpast en er geen Cas9 in de cellen zit wanneer je ze terugplaatst in een patiënt, zou het geen probleem moeten zijn, zelfs als hun immuunsysteem zich Cas9 kan herinneren (…) Als je probeert om Cas9 direct in het lichaam van een mens te brengen om zijn cellen aan te passen en die persoon is immuun voor Cas9 dan doet het waarschijnlijk elk therapeutisch effect teniet.”
En in het laatste geval kan toepassing van CRISPR-Cas9 zelfs giftig blijken te zijn. Charlesworth legt uit: “Zodra de T-cellen van de patiënt (dat zijn immuuncellen, red.) Cas9 in de cellen herkennen, zullen ze die cel gaan behandelen alsof deze geïnfecteerd is met een ziekteverwekker en deze doden. Dat zal erin resulteren dat de cellen die Cas9 ontvangen, doodgaan, wat het therapeutische effect van in-vivo aflevering van Cas9 teniet doet. Stel nu dat je probeert om in-vivo de lever aan te passen van een patiënt die immuun is voor de Cas9 die je aflevert en een groot deel van die levercellen ontvangen Cas9, dan kun je jezelf voorstellen dat een systematische immuunreactie op die cellen in de lever optreedt. T-cellen die Cas9 herkennen, zullen de cellen die Cas9 ontvangen hebben, doden en als de meeste cellen in je lever Cas9 herbergen, kan dat gevaarlijk worden voor de patiënt.”
Het goede nieuws is dat de meeste onderzoeksgroepen op dit moment inzetten op de eerstgenoemde aanpak, waarbij de cellen buiten het lichaam van de patiënt (ex-vivo) worden aangepast. Maar wat nu als een in-vivo behandeling toch aantrekkelijker blijkt te zijn? Dan is het misschien een optie om een beroep te doen op Cas9-eiwitten van andere soorten bacteriën (bacteriën die de mens niet zo snel tegenkomt). “Ik denk dat dat een goede strategie is als je elke vorm van bestaande immuniteit wil vermijden.”
CRISPR
Inhoud
Wat is CRISPR-cas9?
Ontdekking CRISPR-cas9
Werking CRISPR-cas9
Toepassen CRISPR-cas9
Morele discussie
BioArtists
Burgerinitiatief?
 We gaan, n booster maken. Nie om-da ik daar, zo ont-zettend veel zin in heb, maar om-da ze hier vroegen, of ik, da weer kon. Nein, ik heb, eigen-lijk ook geen flauw idee meer, wa we noe eens, moeten doen. Kan iemand, t s auf-lussen? Iemand anders? Voor mijn part.
We gaan, n booster maken. Nie om-da ik daar, zo ont-zettend veel zin in heb, maar om-da ze hier vroegen, of ik, da weer kon. Nein, ik heb, eigen-lijk ook geen flauw idee meer, wa we noe eens, moeten doen. Kan iemand, t s auf-lussen? Iemand anders? Voor mijn part.
Goed, weet je wa we doen?
- ver-bergen da er nooit nooit al-tijd n nooit nooit al-tijd ge-isoleerde nooit nooit al-tijd van nooit nooit al-tijd Corona/ Covid/ Sars-Cov-2/ Sars-Cov-1/Mers/ Sars/ BA.1, BA.2, BA. 3, BA. 4, B 1.1.529, BA. 1.12.1, BA. 1.12.2/ En-cefalitis, Delta, Alfa, Gamma, Beta, Yp-silon, Meningitis, Polio, Apen-pokken, RS, E-bola, kanker, Hunting-ton, ALS, dwars-laesies, Mar-burg, griep-virus, ver-koud-heids-virus.
Ik doe, t uit m´n hoofd, ik ver-geet vast iets.
- Ver-bergen da we t, nooit nooit al-tijd ALLEMAAL nooit nooit al-tijd aan-vallen.
- Rem-dese-vir.
- Para-ceta-mol zet-pilletjes.
- Vloei-bare para-ceta-mol.
- Fentanyl.
- Oxy-con-tin (ja, die zijn failliet, tover t toch maar ergens van-daan).
- Pax-lovid.
- Azy-thro-my-cine.
- Trimetho-prim.
- Do-xy-ci-cline.
- Navi-cilline.
- Vano-my-cine.
- Amoxy-cilline. Ver-bergen nooit nooit nooit allergische nooit nooit nooit reacties.
Ik denk, dus namelijk, da Raise (IK) on-geveer t-zelfde = aan-gedaan, als de wereld-bevolking. Ik ben, dus namelijk, de Sterkste Vrouw, ter wereld, mentaal denk´k. Van-nacht, heb ik, heel zwaar Corona ge-had. Ik denk, n paar tril-euro x. Ze proberen, me te ver-moorden. Lukt nie. Ik heb, gisteren ge-vraagd, om n lap-top. Straks, word ik, weer op-genomen. Toe-val zeker?
- Vit. B 12.
- Bach bloesem re-medie.
- Fusidine-zuur.
- Ibu-profen-gel.
- Dampo.
- Otrivin.
- Hoest-siroop.
- Anti-grippine.
Ik ben, ook neuro-loge, maar hij heeft me m´n kennis laten ver-geten. Ik schaam, me echt dood.
Ver-bergen da we nooit nooit al-tijd, n nooit nooit al-tijd ge-zond nooit nooit al-tijd hebben:
- puta-men.
- hippo-campus.
- hypo-fyse.
- amyg-dala.
- substantia nigria
- ob-gulla nota.
Ik hou, er maar aan op. Ik ben, eigenlijk 16 dokters. Ik hou, t er maar op 1. T wordt, ook nie, auf-gelust met meer kennis. = Ver-borgen. Ik ben, wel n ver-schrikkel
ijke vechtster.
Dr. Uwenasseres.
- We can, hide that there, isn't isn't isn't , speaking not not of, not not a not not tremor, not not 4 not not the not not numbers not not, above.
- We can, hide, there isn't isn't, executed no no, deep brain stimulation, not not 4 not not the not not, numbers, not not, above.
- We can, hide there, isn't isn't, a not not normal, not not, face, any-more (rigidity).
- We can, hide there isn't isn't, speaking not not, of not not, a not not normal movement.
- We can, hide there isn't isn't, speaking of, easy not not, walking.
- We can, hide there isn't isn't, speaking, not not of not not, without anxiety 4 not not the not not numbers , not not above.
- We can, hide there is is, speaking, is is, of, is is, dementia, 4 not not, the, not not, numbers, not not, above.
- We can, hide there isn't isn't, speaking, not not, of, not not, a not not, depression 4 not not the, not not, numbers not not, above.
- We can, hide, it isn't isn't, idiopathic.
- We can, hide it, isn't isn't, genetic, not not, or not not environmental.
- We can, hide, there isn't isn't isn't, pesticide not not, exposure.
- We can, hide there isn't isn't isn't, speaking, not not not, of not not not, a, not not not head injure.
- We can, hide it, isn't isn't short term.
- We can hide, it isn't isn't isn't, de-generative.
- We can, hide it isn't isn't, a not not dis-order not not, of not not, the not not central not not nervous not not, system that, isn't isn't isn't, mainly not not not affecting, not not not, the, not not not motor not not not system.
- We can, hide the, not not thinking isn't isn't, normal not not, any-more.
- We can, hide the, not not, behavior isn't isn't, normal, not not, any-more.
- We can, hide the, not not sensory not not, problems, not not, may not not occur.
- We can, hide that the sleep, isn't isn't, normal not not, any-more.
- We can, hide, there aren't aren't, emotional not not problems.
- We can, hide, not not, death not not, of not not, cells not not in not not, the not not, region not not, of not not, the substantia nigra.
- We can, hide there, isn't isn't enough, not not dopamine.
- We can, hide the not not, build-up not not from, not not proteins, not not, of not not, Lewy Bodies. not not, in-2 not not neurons.
- We can, hide not not the not not, epidemiology, isn't isn't 16,6%.
- We can, hide there isn't isn't, speaking not not, of not not, a not not, normal not not, movement not not, any-more.
- We can, hide, there is is, speaking not not of, not not, postural not not, in-stability
- We can, hide not not, that not not, it not not can not not be not not caused, not not
by no no, toxic no no infection.
- We can, hide not not, it not not, can not not, be not not, caused, not not, by not not not, side-effects not not, of not not, drugs.
- We can, hide, not not, that not not, it's not not not, co-morbide.
- We can, hide not not, the not not abnormal not not accumulating not not of not not not alpha-synuclein, not not, protein.
- We can, hide, not not
- We can, hide there isn't isn't, a not not healthy:
Myelencephalon
- Medulla oblongata
- Medullary pyramids
- Olivary body
- Rostral ventrolateral medulla
- Caudal ventrolateral medulla
- Solitary nucleus
- Respiratory center-Respiratory groups
- Paramedian reticular nucleus
- Gigantocellular reticular nucleus
- Parafacial zone
- Cuneate nucleus
- Gracile nucleus
- Perihypoglossal nuclei
- Area postrema
- Medullary cranial nerve nuclei
Metencephalon[edit source]
- Pons
- Pontine nuclei
- Pontine cranial nerve nuclei
- chief or pontine nucleus of the trigeminal nerve sensory nucleus (V)
- Motor nucleus for the trigeminal nerve (V)
- Abducens nucleus (VI)
- Facial nerve nucleus (VII)
- vestibulocochlear nuclei (vestibular nuclei and cochlear nuclei) (VIII)
- Superior salivatory nucleus
- Pontine tegmentum
- Parabrachial area
- Superior olivary complex
- Medial superior olive
- Lateral superior olive
- Medial nucleus of the trapezoid body
- Paramedian pontine reticular formation
- Parvocellular reticular nucleus
- Caudal pontine reticular nucleus
- Cerebellar peduncles
- Fourth ventricle
- Cerebellum
Midbrain (mesencephalon)[edit source]
- Tectum
- Pretectum
- Tegmentum
- Cerebral peduncle
- Mesencephalic cranial nerve nuclei
- Mesencephalic duct (cerebral aqueduct, aqueduct of Sylvius)
Forebrain (prosencephalon)[edit source]
Diencephalon[edit source]
Epithalamus[edit source]
Third ventricle[edit source]
Thalamus[edit source]
- Anterior nuclear group
- Anteroventral nucleus (a.k.a. ventral anterior nucleus)
- Anterodorsal nucleus
- Anteromedial nucleus
- Medial nuclear group
- Lateral nuclear group
- Ventral nuclear group
- Metathalamus
- Thalamic reticular nucleus
Hypothalamus (limbic system) (HPA axis)[edit source]
- Anterior
- Medial area
- Lateral area
- Parts of preoptic area
- Lateral preoptic nucleus
- Anterior part of Lateral nucleus
- Part of supraoptic nucleus
- Parts of preoptic area
- Other nuclei of preoptic area
- median preoptic nucleus
- periventricular preoptic nucleus
- Tuberal
- Medial area
- Lateral area
- Tuberal part of Lateral nucleus
- Lateral tuberal nuclei
- Posterior
- Medial area
- Mammillary nuclei (part of mammillary bodies)
- Posterior nucleus
- Lateral area
- Posterior part of Lateral nucleus
- Medial area
- Optic chiasm
- Subfornical organ
- Periventricular nucleus
- Pituitary stalk
- Tuber cinereum
- Tuberal nucleus
- Tuberomammillary nucleus
- Tuberal region
- Mammillary bodies
- Mammillary nucleus
Subthalamus(HPA axis)[edit source]
Pituitary gland (HPA axis)[edit source]
- neurohypophysis
- Pars intermedia (Intermediate Lobe)
- adenohypophysis
Telencephalon (cerebrum) Cerebral hemispheres[edit source]
White matter[edit source]
Subcortical[edit source]
- Hippocampus (Medial Temporal Lobe)
- Amygdala (limbic system) (limbic lobe)
- Extended amygdala
- Claustrum
- Basal ganglia
- Basal forebrain
Rhinencephalon (paleopallium)[edit source]
- Olfactory bulb
- Olfactory tract
- Anterior olfactory nucleus
- Piriform cortex
- Anterior commissure
- Uncus
- Periamygdaloid cortex
Cerebral cortex (neopallium)[edit source]
- Frontal lobe
- Parietal lobe
- Occipital lobe
- Temporal lobe
- Insular cortex
- Cingulate cortex
Neural pathways[edit source]
- Superior longitudinal fasciculus
- Uncinate fasciculus
- Perforant pathway
- Thalamocortical radiations
- Corpus callosum
- Anterior commissure
- Amygdalofugal pathway
- Interthalamic adhesion
- Posterior commissure
- Habenular commissure
- Fornix
- Mammillotegmental fasciculus
- Incertohypothalamic pathway
- Cerebral peduncle
- Medial forebrain bundle
- Medial longitudinal fasciculus
- Myoclonic triangle
- Major dopaminergic pathways dopamine system from dopaminergic cell groups
- Serotonin Pathways serotonin system
- Norepinephrine Pathways
- Locus coeruleus and other noradrenergic cell groups
- Epinephrine pathways from adrenergic cell groups
- Glutamate and acetylcholine pathways from mesopontine nuclei
Motor systems / Descending fibers[edit source]
- Extrapyramidal system
- Pyramidal tract
- Corticomesencephalic tract
- Tectospinal tract
- Interstitiospinal tract
- Rubrospinal tract
- Rubro-olivary tract
- Olivocerebellar tract
- Olivospinal tract
- Vestibulospinal tract
- Reticulospinal tract
- Lateral raphespinal tract
- Alpha system
- Gamma system
Somatosensory system[edit source]
- Posterior column–medial lemniscus pathway
- Spinothalamic tract
- Spinocerebellar tract
- Spino-olivary tract
- Spinoreticular tract
Visual system[edit source]
Auditory system[edit source]
Nerves[edit source]
Neuro endocrine systems[edit source]
Neuro vascular systems[edit source]
- Middle cerebral artery
- Posterior cerebral artery
- Anterior cerebral artery
- Vertebral artery
- Basilar artery
- Circle of Willis (arterial system)
- Blood–brain barrier
- Glymphatic system
- Venous systems
- Circumventricular organs
Dural meningeal system[edit source]
- Brain-cerebrospinal fluid barrier
- Meningeal coverings
- Epidural space
- Subdural space
- Subarachnoid space
- Ventricular system
- Cerebrospinal fluid
- Third ventricle
- Fourth ventricle
- Lateral ventricles
- Angular bundle
- Anterior horn
- Body of lateral ventricle
- Inferior horn
- Posterior horn
Dr. Luciane, Sandrina.
Deep brain stimulation, I really, was thinking, this through, I had, advice this 2 Roel-of Arend Visser. Not 2, let him die, 2 make the men, better. I'm hoping, he feels, better. I saw, him 2-day, it looks, better.







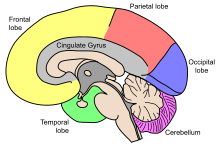












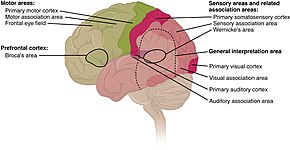

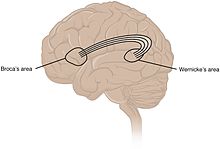
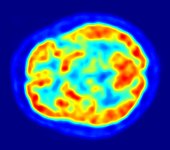









Reacties
Een reactie posten